Zurnai: Package Insert / Prescribing Info
Package insert / product label
Generic name: nalmefene hydrochloride
Dosage form: injection, solution
Drug class: Antidotes
Medically reviewed by Drugs.com. Last updated on Aug 12, 2025.
On This Page
- Indications and Usage
- Dosage and Administration
- Dosage Forms and Strengths
- Contraindications
- Warnings and Precautions
- Adverse Reactions/Side Effects
- Use In Specific Populations
- Description
- Clinical Pharmacology
- Nonclinical Toxicology
- How Supplied/Storage and Handling
- Storage and Handling
- Patient Counseling Information
Highlights of Prescribing Information
ZURNAI (nalmefene injection), for intramuscular or subcutaneous use
Initial U.S. Approval: 1995
Indications and Usage for Zurnai
ZURNAI is an opioid antagonist indicated for the emergency treatment of known or suspected opioid overdose induced by natural or synthetic opioids in adults and pediatric patients aged 12 years and older, as manifested by respiratory and/or central nervous system depression. (1)
ZURNAI is intended for immediate administration as emergency therapy in settings where opioids may be present. (1)
ZURNAI is not a substitute for emergency medical care. (1)
Zurnai Dosage and Administration
- ZURNAI is for intramuscular and subcutaneous use only. (2.1)
- Seek emergency medical care immediately after use. (2.1)
- Administer ZURNAI to the outer thigh, through clothing if necessary. (2.1)
- Administer additional doses of ZURNAI using a new ZURNAI auto-injector for each dose. If the patient does not respond or responds and then relapses into respiratory depression, additional doses of ZURNAI may be given every 2 to 5 minutes until emergency medical assistance arrives. (2.2)
- See Full Prescribing Information and Instructions for Use for important information on how to safely administer ZURNAI. (2.1)
- Additional supportive and/or resuscitative measures may be helpful while awaiting emergency medical assistance. (2.2)
Dosage Forms and Strengths
Injection: 1.5 mg nalmefene base/0.5 mL in a prefilled, single-dose auto-injector (3)
Contraindications
- Hypersensitivity to nalmefene hydrochloride or to any other ingredients in ZURNAI. (4)
Warnings and Precautions
- Risk of Recurrent Respiratory and CNS Depression: A recurrence of respiratory depression is possible, therefore, keep the patient under continued surveillance and administer repeat doses of ZURNAI using a new auto-injector with each dose while awaiting emergency medical assistance. (5.1)
- Risk of Limited Efficacy with Partial Agonists or Mixed Agonists/Antagonists: Reversal of respiratory depression by partial agonists or mixed agonist/antagonists such as buprenorphine and pentazocine, may be incomplete. Repeat doses may be required. (5.2)
- Precipitation of Severe Opioid Withdrawal: The use of ZURNAI in patients who are opioid dependent may precipitate opioid withdrawal. In neonates, opioid withdrawal may be life-threatening if not recognized and properly treated. Monitor for the development of opioid withdrawal. (5.3)
- Risk of Cardiovascular (CV) Effects: Abrupt postoperative reversal of opioid depression may result in adverse CV effects. These events have primarily occurred in patients who had preexisting CV disorders or received other drugs that may have similar adverse CV effects. Monitor these patients closely in an appropriate healthcare setting after use of nalmefene hydrochloride. (5.3)
- Risk of Opioid Overdose from Attempts to Overcome the Blockade: Attempts to overcome opioid withdrawal symptoms caused by opioid antagonists with high or repeated doses of exogenous opioids may lead to opioid intoxication and death. (5.4)
Adverse Reactions/Side Effects
Most common adverse reactions (incidence > 5%) are feeling hot, nausea, headache, dizziness, chills, vomiting, allodynia, palpitations, tinnitus, ear discomfort, feeling abnormal, burning sensation, hot flush, and irritability. (6)
To report Suspected Adverse Reactions, contact Purdue Pharma L.P. at 1-888-726-7535 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 8/2024
Full Prescribing Information
1. Indications and Usage for Zurnai
ZURNAI is indicated for the emergency treatment of known or suspected opioid overdose induced by natural or synthetic opioids in adults and pediatric patients aged 12 years and older, as manifested by respiratory and/or central nervous system depression.
ZURNAI is intended for immediate administration as emergency therapy in settings where opioids may be present.
ZURNAI is not a substitute for emergency medical care.
2. Zurnai Dosage and Administration
2.1 Important Administration Instructions
- All approved nalmefene products achieve plasma concentrations that have been shown to be efficacious in reversing the effects of opioid overdose. Comparing different products on a nominal mg-for-mg basis may be misleading.
- ZURNAI is for intramuscular and subcutaneous use only.
- The device is ready to use. No device assembly is required.
- Do not prime or test prior to administration. ZURNAI delivers its entire contents automatically, upon injection.
- Inject ZURNAI into the anterolateral aspect of the thigh.
- ZURNAI can be administered through clothing if necessary.
- Do not reuse ZURNAI. Each ZURNAI device contains a single dose of nalmefene and cannot be reused.
- Because treatment of suspected opioid overdose must be performed by someone other than the patient, instruct the prescription recipient to inform those around them about the presence of ZURNAI and the Instructions for Use.
- Instruct the patient or caregiver to read the Instructions for Use at the time they receive a prescription for ZURNAI. Emphasize the following instructions to the patient or caregiver:
- –
- Administer ZURNAI as quickly as possible because prolonged respiratory depression may result in damage to the central nervous system or death.
- –
- Always seek emergency medical assistance after administration of the first dose of ZURNAI in the event of a suspected, potentially life-threatening opioid emergency. Keep the patient under continued surveillance until emergency personnel arrive.
- –
- Additional doses of ZURNAI may be required until emergency medical assistance becomes available.
- –
- If available, re-administer ZURNAI using a new auto-injector, every 2 to 5 minutes if the patient does not respond or responds and then relapses into respiratory depression.
- –
- Once the safety seal is broken and blue cap is removed, ZURNAI must be used immediately or disposed of properly. Do not attempt to replace the blue cap once it is removed.
- –
- Visually inspect ZURNAI through the viewing window for particulate matter and discoloration prior to administration. Do not administer unless the solution is clear, free of particulates, and the glass container is undamaged.
- –
- Administer ZURNAI according to the printed instructions on the device label, carton, and the Instructions for Use.
- ⮚
- Place the needle guard of ZURNAI against the outer thigh. Press the needle end firmly into the injection site until you hear a click and then hold for 3 seconds. After 3 seconds, the viewing window should turn completely orange, signaling that ZURNAI has delivered the intended dose of nalmefene.
- ⮚
- Remove ZURNAI from the outer thigh.
- ⮚
- Call for emergency medical assistance immediately after administration of the first dose of ZURNAI.
- ⮚
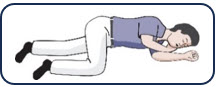
- Move the patient on their side (recovery position). Remain with the patient until emergency medical assistance arrives, even if the patient wakes up.
2.2 Dosing in Adults and Pediatric Patients 12 Years and Older
Initial Dosing:
The recommended dose of ZURNAI in adults and pediatric patients aged 12 years and older is 1.5 mg delivered by intramuscular or subcutaneous injection into the anterolateral aspect of the thigh, through clothing if necessary.
Repeat Dosing:
Seek emergency medical assistance as soon as possible after administration of the first dose of ZURNAI. The requirement for repeat doses of ZURNAI depends upon the amount, type, and route of administration of the opioid being antagonized.
If the patient responds to ZURNAI and subsequently relapses back into respiratory depression before emergency assistance arrives, administer an additional dose of ZURNAI using a new auto-injector and continue surveillance of the patient.
If the desired response is not obtained after 2 to 5 minutes, administer an additional dose of ZURNAI using a new auto-injector. If there is still no response and additional doses are available, administer additional doses of ZURNAI every 2 to 5 minutes using a new ZURNAI auto-injector for each dose until emergency medical assistance arrives.
Additional supportive and/or resuscitative measures may be helpful while awaiting emergency medical assistance.
2.3 Dosing Modifications Due to Partial Agonists or Mixed Agonists/Antagonists
Reversal of respiratory depression by partial agonists or mixed agonist/antagonists, such as buprenorphine and pentazocine, may be incomplete and require repeated administration of ZURNAI using a new auto-injector [see Warnings and Precautions (5.2)].
4. Contraindications
ZURNAI is contraindicated in patients known to be hypersensitive to nalmefene hydrochloride or to any other ingredients in the product.
5. Warnings and Precautions
5.1 Risk of Recurrent Respiratory and Central Nervous System Depression
Respiratory depression in the community overdose setting may be complex and involve the effects of multiple or unknown drugs, some of which may be long-acting opioids. While the duration of action of nalmefene is as long as most opioids, a recurrence of respiratory depression is possible, even after an apparently adequate initial response to ZURNAI treatment [see Clinical Pharmacology (12.3)]. Therefore, it is necessary to seek emergency medical assistance immediately after administration of the first dose of ZURNAI and to keep the patient under continued surveillance. A second dose may be necessary if there is recurrence of symptoms of opioid overdose. Additional supportive and/or resuscitative measures may be helpful while awaiting emergency medical assistance [see Dosage and Administration (2.2)].
5.2 Risk of Limited Efficacy with Partial Agonists or Mixed Agonist/Antagonists
Reversal of respiratory depression by partial agonists or mixed agonist/antagonists such as buprenorphine and pentazocine, may be incomplete. Repeat doses of ZURNAI may be required to antagonize buprenorphine because the latter has a long duration of action due to its slow rate of binding and subsequent slow dissociation from the opioid receptor [see Dosage and Administration (2.3)]. Buprenorphine antagonism is characterized by a gradual onset of the reversal effects and a decreased duration of action of the normally prolonged respiratory depression.
5.3 Precipitation of Severe Opioid Withdrawal
The use of ZURNAI in patients who are opioid dependent may precipitate opioid withdrawal characterized by the following signs and symptoms: body aches, diarrhea, tachycardia, fever, runny nose, sneezing, piloerection, sweating, yawning, nausea or vomiting, nervousness, restlessness or irritability, shivering or trembling, abdominal cramps, weakness, and increased blood pressure.
Abrupt postoperative reversal of opioid depression after using ZURNAI may result in nausea, vomiting, sweating, tremulousness, tachycardia, hypotension, hypertension, seizures, ventricular tachycardia and fibrillation, pulmonary edema, and cardiac arrest. Death, coma, and encephalopathy have been reported as sequelae of these events. These events have primarily occurred in patients who had pre-existing cardiovascular disorders or received other drugs that may have similar adverse cardiovascular effects. After use of ZURNAI, monitor patients with pre-existing cardiac disease or patients who have received medications with potential adverse cardiovascular effects for hypotension, ventricular tachycardia or fibrillation, and pulmonary edema in an appropriate healthcare setting. It has been suggested that the pathogenesis of pulmonary edema associated with the use of nalmefene is similar to neurogenic pulmonary edema, i.e., a centrally mediated massive catecholamine response leading to a dramatic shift of blood volume into the pulmonary vascular bed resulting in increased hydrostatic pressures.
ZURNAI is not indicated for use in patients less than 12 years of age. In neonates, opioid withdrawal may be life-threatening if not recognized and properly treated and may include the following signs and symptoms: convulsions, excessive crying, and hyperactive reflexes. Monitor the patient for the development of the signs and symptoms of opioid withdrawal. There may be clinical settings, particularly the postpartum period in neonates with known or suspected exposure to maternal opioid use, where it is preferable to avoid the abrupt precipitation of opioid withdrawal symptoms. In these settings, use an alternative, opioid antagonist product that can be titrated to effect and, where applicable, dosed according to weight [see Use in Specific Populations (8.4)].
5.4 Risk of Opioid Overdose from Attempts to Overcome the Blockade
ZURNAI is unlikely to produce acute withdrawal symptoms in non-opioid dependent patients. The use of ZURNAI in patients who are opioid dependent may precipitate opioid withdrawal. Attempting to overcome opioid withdrawal symptoms caused by opioid antagonists with high or repeated doses of exogenous opioids could lead to opioid intoxication and death.
Inform patients of the potential consequences of trying to overcome the opioid blockade. Get emergency medical assistance as soon as possible after use of ZURNAI regardless of withdrawal symptoms.
6. Adverse Reactions/Side Effects
The following serious adverse reactions are described elsewhere in the labeling:
- Recurrent Respiratory and Central Nervous System Depression [see Warnings and Precautions (5.1)]
- Precipitation of Severe Opioid Withdrawal [see Warnings and Precautions (5.3)]
6.1 Clinical Trial Experience
Adult Clinical Trial Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The safety of ZURNAI is supported by pharmacokinetic and pharmacodynamic studies of ZURNAI in healthy subjects in a normal state and under steady state opioid agonism. The following adverse reactions were observed.
In a pharmacokinetic study (NAL1005) of 21 healthy adult volunteers exposed to one dose of ZURNAI the most common adverse reactions were: dizziness and headache.
In a pharmacodynamic study (NAL1004) of 23 healthy adult volunteers exposed to one dose of ZURNAI, the most common adverse reactions were: feeling hot, chills, nausea, allodynia, and headache.
| Nalmefene Auto-Injector 1.5 mg IM | |||
|---|---|---|---|
| System Organ Class Preferred Term | Pooled NAL1004 and NAL1005 N=44 n (%) | Study NAL1004 N=23 n (%) | Study NAL1005 N=21 n (%) |
| Any AR | 28 (63.6) | 21 (91.3) | 7 (33.3) |
| Cardiac disorders | |||
| Palpitations | 4 (9.1) | 4 (17.4) | 0 |
| Ear and labyrinth disorders | |||
| Tinnitus | 4 (9.1) | 4 (17.4) | 0 |
| Ear discomfort | 3 (6.8) | 3 (13.0) | 0 |
| Gastrointestinal disorders | |||
| Nausea | 8 (18.2) | 6 (26.1) | 2 (9.5) |
| Vomiting | 5 (11.4) | 3 (13.0) | 2 (9.5) |
| General disorders and administration site conditions | |||
| Feeling hot | 11 (25.0) | 11 (47.8) | 0 |
| Chills | 6 (13.6) | 6 (26.1) | 0 |
| Feeling abnormal | 3 (6.8) | 3 (13.0) | 0 |
| Nervous system disorders | |||
| Dizziness | 7 (15.9) | 4 (17.4) | 3 (14.3) |
| Headache | 8 (18.2) | 5 (21.7) | 3 (14.3) |
| Allodynia | 5 (11.4) | 5 (21.7) | 0 |
| Burning sensation | 3 (6.8) | 3 (13.0) | 0 |
| Psychiatric disorders | |||
| Irritability | 3 (6.8) | 3 (13.0) | 0 |
| Vascular disorders | |||
| Hot flush | 3 (6.8) | 3 (13.0) | 0 |
Adverse reaction information was obtained following administration of nalmefene hydrochloride injection to 152 healthy volunteers and to 1127 patients in controlled clinical trials for the treatment of opioid overdose or for postoperative opioid reversal.
| Adverse Reaction | Nalmefene N=1127 | Placebo N=77 |
|---|---|---|
| Nausea | 18% | 6% |
| Vomiting | 9% | 4% |
| Tachycardia | 5% | - |
| Hypertension | 5% | - |
| Postoperative pain | 4% | N/A |
| Fever | 3% | - |
| Dizziness | 3% | 1% |
| Headache | 1% | 4% |
| Chills | 1% | - |
| Hypotension | 1% | - |
| Vasodilatation | 1% | - |
Incidence less than 1%
CARDIOVASCULAR: Bradycardia, arrhythmia
DIGESTIVE: Diarrhea, dry mouth
NERVOUS SYSTEM: Somnolence, depression, agitation, nervousness, tremor, confusion, withdrawal syndrome, myoclonus
RESPIRATORY: Pharyngitis
SKIN: Pruritus
UROGENITAL: Urinary retention
The incidence of adverse events was highest in patients who received more than the recommended dose of nalmefene hydrochloride injection.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of nalmefene. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Abrupt reversal of opioid depression using nalmefene in both postoperative and emergency department settings has resulted in nausea, vomiting, sweating, tremulousness, seizures, and cardiovascular instability including tachycardia, hypotension, hypertension, ventricular tachycardia and fibrillation, pulmonary edema, and cardiac arrest. Death, coma, and encephalopathy have been reported as sequelae of these events. These events have primarily occurred in patients who had pre-existing cardiovascular disorders or received other drugs that may have similar adverse cardiovascular effects.
In persons who were physically dependent on opioids, abrupt reversal of opioid effects has precipitated an acute withdrawal syndrome. Signs and symptoms have included: body aches, fever, sweating, runny nose, sneezing, piloerection, yawning, weakness, shiver or trembling, nervousness, restlessness or irritability, diarrhea, nausea or vomiting, abdominal cramps, increased blood pressure, and tachycardia. In some patients, there may be aggressive behavior upon abrupt reversal of an opioid overdose. In the neonate, opioid withdrawal symptoms also included convulsions, excessive crying, and hyperactive reflexes.
Related/similar drugs
8. Use In Specific Populations
8.1 Pregnancy
Risk Summary
Life-sustaining therapy for opioid overdose should not be withheld [see Clinical Considerations]. There are no available data on nalmefene use in pregnant women to evaluate for a drug-associated risk of major birth defects or miscarriage. In animal reproduction studies, no effects on embryo-fetal development were observed in rats and rabbits treated with nalmefene [see Data].
The background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Clinical Considerations
Disease-associated maternal and/or embryo/fetal risk
An opioid overdose is a medical emergency and can be fatal for the pregnant woman and fetus if left untreated. Treatment with ZURNAI for opioid overdose should not be withheld because of potential concerns regarding the effects of ZURNAI on the fetus.
Data
Animal Data
Reproduction studies have been performed in rats and rabbits by oral administration and in rabbits by intravenous administration of nalmefene. No effects on embryo-fetal development were observed at rat oral doses up to 1200 mg/m2/day and rabbit oral doses up to 2400 mg/m2/day, and intravenous dose up to 96 mg/m2/day, which is 52 times the human dose of 3.0 mg (two ZURNAI administrations) based on body surface area comparison. The treatment in rats did not affect offspring survival.
8.2 Lactation
Risk Summary
There are no data on the presence of nalmefene and its metabolites in human milk, the effects of nalmefene on the breastfed child, or the effects on milk production. Nalmefene and its metabolites are present in rat milk [see Data]. When a drug is present in animal milk, it is likely that the drug will be present in human milk.
Data
Nalmefene and its metabolites were secreted into rat milk, reaching concentrations approximately three times those in plasma at one hour and decreasing to about half the corresponding plasma concentrations by 24 hours following bolus administration. The concentration of nalmefene in animal milk does not necessarily predict the concentration of drug in human milk.
8.4 Pediatric Use
The safety and effectiveness of ZURNAI for the emergency treatment of known or suspected opioid overdose, as manifested by respiratory and/or central nervous system depression, have been established in pediatric patients aged 12 years and older.
Use for this indication in this age group is supported by adult studies and pharmacokinetic simulation [see Clinical Pharmacology (12.3)]. There have been no studies conducted to evaluate the use of ZURNAI in pediatric patients.
The safety and effectiveness of ZURNAI for the emergency treatment of known or suspected opioid overdose, as manifested by respiratory and/or central nervous system depression, have not been established in pediatric patients younger than 12 years of age.
8.5 Geriatric Use
Clinical studies of nalmefene hydrochloride injection did not include sufficient number of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. Geriatric patients have a greater frequency of decreased hepatic, renal, or cardiac function, or other drug therapy. Therefore, the systemic exposure of nalmefene can be higher in these patients.
8.6 Hepatic Impairment
Hepatic impairment substantially reduces the clearance of nalmefene [see Clinical Pharmacology (12.3)]. For single episodes of opioid antagonism, adjustment of ZURNAI dosage is not required.
8.7 Renal Impairment
Renal impairment substantially reduces the clearance of nalmefene [see Clinical Pharmacology (12.3)]. For single episodes of opioid antagonisms, adjustment of ZURNAI dosage is not required.
11. Zurnai Description
ZURNAI™ (nalmefene injection) is a sterile, pre-filled, single-dose auto-injector designed to deliver a dose of 1.5 mg nalmefene (provided as nalmefene hydrochloride) in 0.5 mL.
Nalmefene hydrochloride, an opioid antagonist, is a 6-methylene analogue of naltrexone. The molecular structure of nalmefene is presented below:
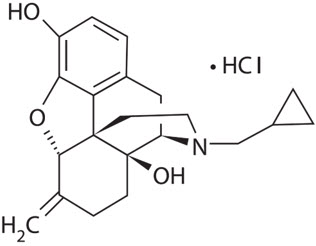
Molecular Formula: C21H25NO3∙HCl
Molecular Weight: 375.9, CAS# 58895-64-0
Chemical Name: 17-(Cyclopropylmethyl)-4,5α-epoxy-6-methylenemorphinan-3,14-diol, hydrochloride salt
Nalmefene is a white to off-white crystalline powder which is freely soluble in water up to 130 mg/mL and slightly soluble in chloroform up to 0.13 mg/mL, with a pKa of 7.63.
Each ZURNAI auto-injector delivers 1.5 mg nalmefene (equivalent to 1.7 mg nalmefene hydrochloride) in 0.5 mL solution. The pH range is 3.5 to 4.5.
The inactive ingredients in ZURNAI nalmefene injection include: hydrochloric acid to adjust pH; magnesium chloride, 4.7 mg; and water for injection.
12. Zurnai - Clinical Pharmacology
12.2 Pharmacodynamics
Nalmefene reverses the effects of natural and synthetic opioids, including respiratory depression, sedation, and hypotension. Pharmacodynamic studies have shown that nalmefene injection has a longer duration of action than naloxone injection at fully reversing doses. Nalmefene has no opioid agonist activity.
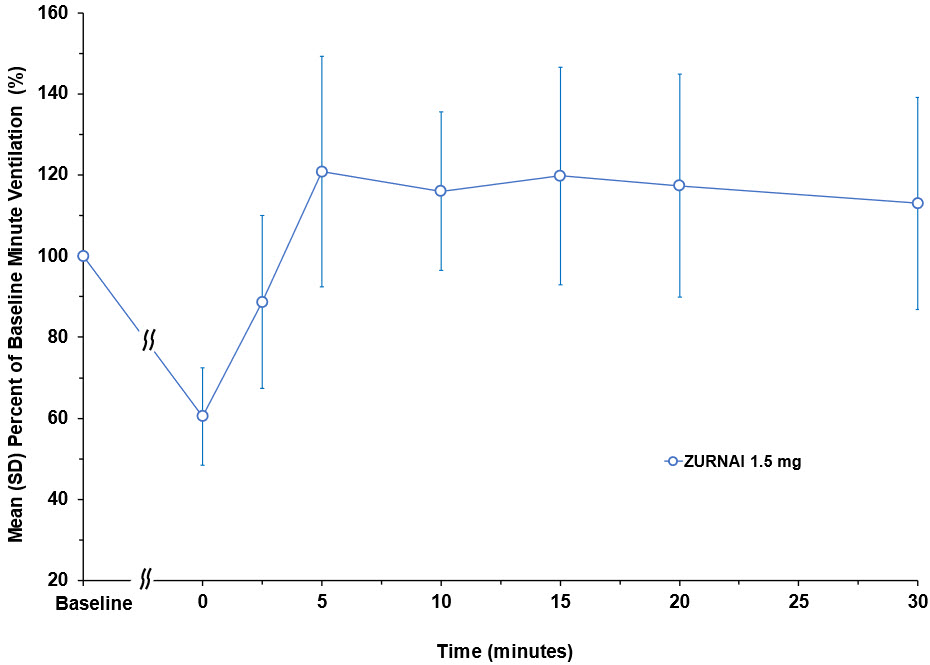
The effect of ZURNAI was studied in an experimental clinical opioid-induced respiratory depression (OIRD) model in twenty-four opioid-experienced, non-opioid dependent subjects (NAL1004). This model assessed changes in minute ventilation (MV) during administration of a 3-step intravenous fentanyl infusion. In step 1, fentanyl was infused until MV nadir (functional OIRD) was achieved. MV nadir was defined as a 50% reduction in MV from baseline or the MV reduction achieved following the maximum permitted fentanyl titration. Following attainment of MV nadir, the fentanyl infusion rate was decreased (step 2) to maintain the fentanyl concentrations. ZURNAI was administered at 10 minutes following MV nadir. Ten minutes following ZURNAI administration, the fentanyl infusion rate was further decreased (step 3) to maintain constant fentanyl concentrations for the remaining duration of the reversal session.
Following ZURNAI administration the time to onset of effect, that is onset of reversal of respiratory depression, was observed between 2.5 to 5 minutes (Figure 1 and Figure 2). At 5 minutes mean change in MV from nadir was 4.42 L/min (Figure 1). Full recovery of respiratory drive was noted between 5 and 15 minutes after ZURNAI administration (Figure 1 and Figure 2).
Figure 1: Reversal of Fentanyl-Induced Respiratory Depression in adult healthy volunteers treated with ZURNAI (nalmefene)
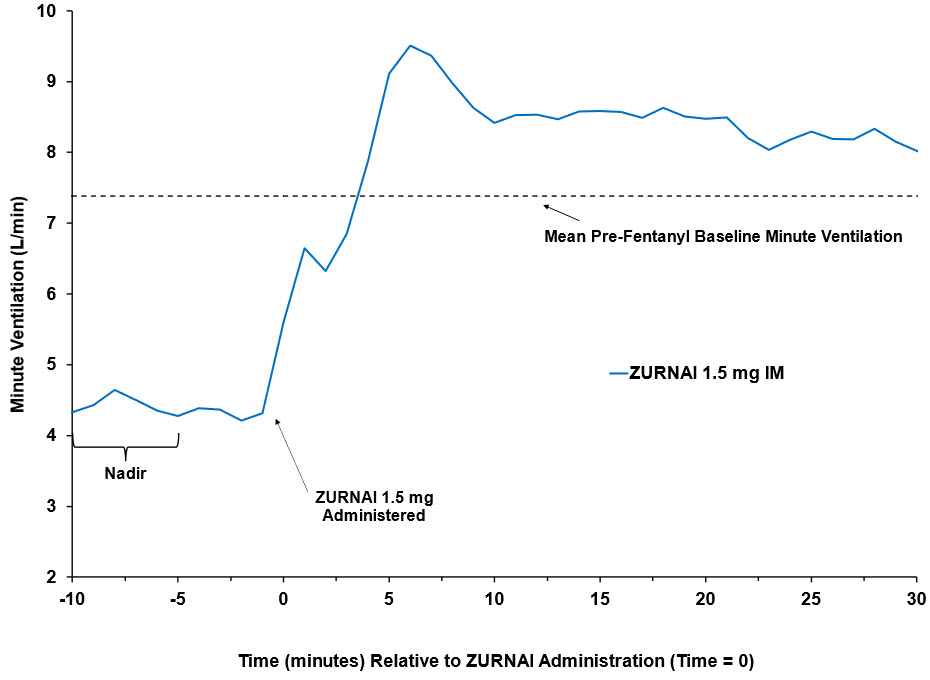
Figure 2: Percent Recovery of Respiratory Drive after Fentanyl Infusion in Minute Ventilation (Mean SD) in Adult Healthy Volunteers with ZURNAI 1.5 mg
Nalmefene is not known to produce respiratory depression, psychotomimetic effects, or pupillary constriction. No pharmacological activity was observed when nalmefene was administered in the absence of opioid agonists.
Nalmefene has not been shown to produce tolerance, physical dependence, or abuse potential.
Nalmefene can produce acute withdrawal symptoms in individuals who are opioid dependent.
12.3 Pharmacokinetics
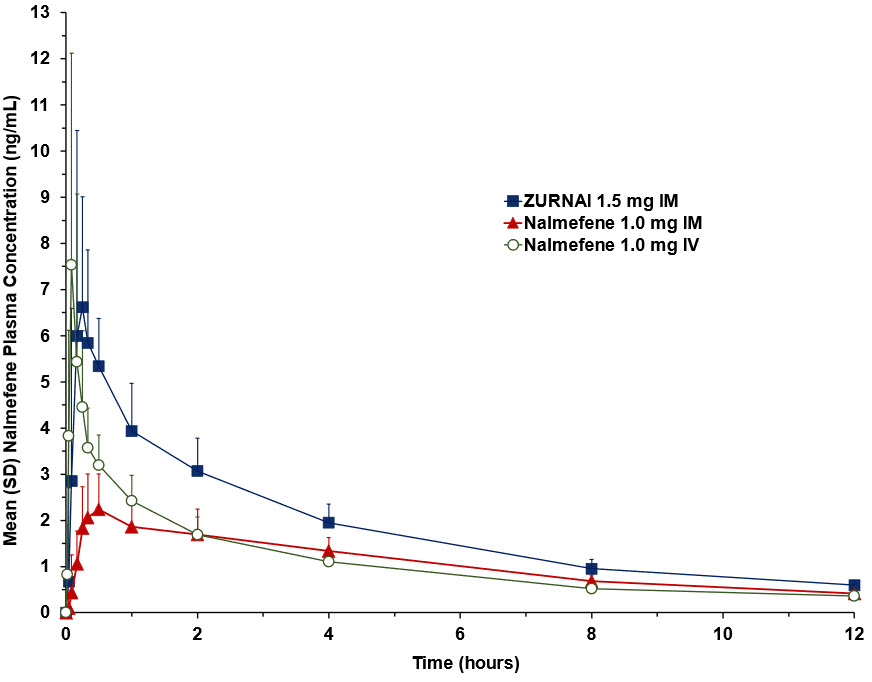
In a pharmacokinetic study (NAL1005) in 24 healthy adult subjects, the relative bioavailability of one dose of ZURNAI administered intramuscularly was compared to a single dose of nalmefene 1.0 mg administered as an intramuscular injection. The pharmacokinetic parameters obtained in this study are shown in Table 3 and the plasma concentration time profiles of nalmefene are presented in Figure 3.
| Parameter | ZURNAI 1.5 mg | Nalmefene IM 1.0 mg | Nalmefene IV 1.0 mg |
|---|---|---|---|
| NA = Not applicable. | |||
| Tmax (h)* | 0.25 (0.083-1.00) | 0.50 (0.083-2.00) | 0.083 (0.083 -0.25) |
| Cmax (ng/mL) | 7.37 (47.5) | 2.39 (32.6) | 6.94 (55.7) |
| AUC0-2.5min (ng-hr/mL) † | 0.011 (288) | 0.001 (241) | 0.062 (56.1) |
| AUC0-5min (ng-hr/mL) † | 0.077 (144) | 0.010 (209) | 0.299 (40.4) |
| AUC0-10min (ng-hr/mL) | 0.320 (85.8) | 0.047 (107) | 0.768 (46.2) |
| AUC0-15min (ng-hr/mL) | 0.831 (62.7) | 0.152 (64.8) | 1.16 (46.1) |
| AUC0-20min (ng-hr/mL) | 1.31 (51.3) | 0.315 (48.3) | 1.50 (41.7) |
| AUC0-30min (ng-hr/mL) | 2.24 (39.3) | 0.647 (40.7) | 2.07 (34.0) |
| AUC0-inf (ng-hr/mL) | 30.53 (16.0) | 17.98 (21.0) | 18.22 (15.3) |
| Frel (%) † | 113 (13.0) | NA | NA |
| T½ (h) † | 9.07 (26.6) | 7.74 (24.3) | 9.12 (16.5) |
Figure 3: Mean Plasma Concentration-Time Profiles of Nalmefene (a) 0-12 hours and (b) 0- 60 minutes Following Administration of 1.5 mg ZURNAI Intramuscular (IM), 1.0 mg Nalmefene IM, and 1.0 mg Nalmefene Intravenous (IV)
(a)
(b)
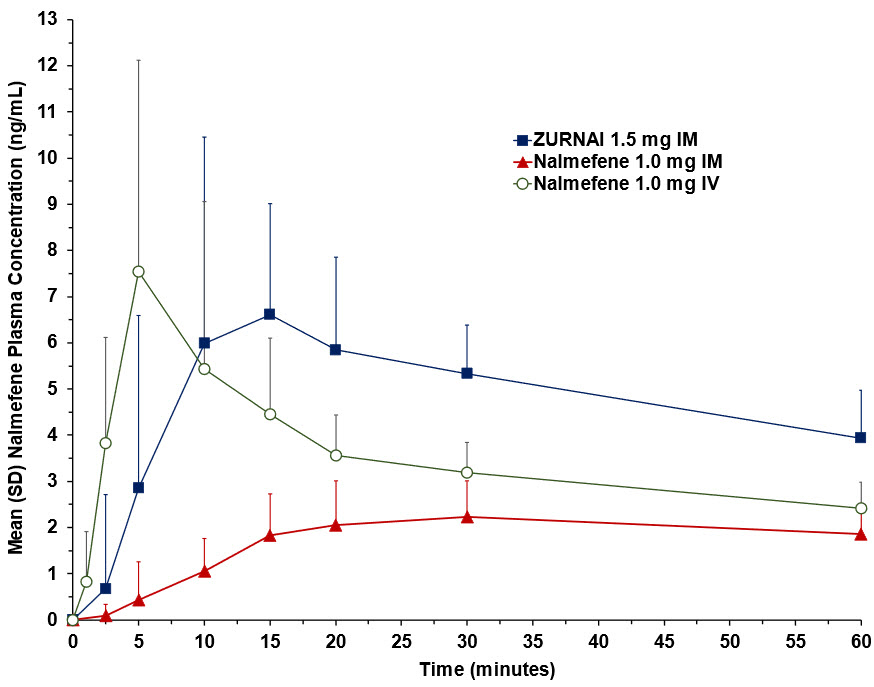
Absorption
After administration of one ZURNAI to healthy adult subjects, the median Tmax for ZURNAI was 0.250 hours, compared to 0.5 hours for the intramuscular nalmefene 1 mg injection.
Based on dose-normalized area under the curve (AUCinf), the mean bioavailability of ZURNAI was 1.13 (Frel) relative to intramuscular administration of nalmefene 1 mg and was 1.15 (Fabs) relative to intravenous administration of nalmefene 1 mg.
Distribution
Following a 1 mg parenteral dose, nalmefene was rapidly distributed. In a study of brain receptor occupancy, a 1 mg dose of nalmefene blocked over 80% of brain opioid receptors within 5 minutes after administration. The apparent volumes of distribution centrally (Vc) and at steady state (Vdss) are 3.9 ± 1.1 L/kg and 8.6 ± 1.7 L/kg, respectively. Ultrafiltration studies of nalmefene have demonstrated that 45% (CV 4.1%) is bound to plasma proteins over a concentration range of 0.1 to 2 mcg/mL. An in vitro determination of the distribution of nalmefene in human blood demonstrated that nalmefene distributed 67% (CV 8.7%) into red blood cells and 39% (CV 6.4%) into plasma. The whole blood to plasma ratio was 1.3 (CV 6.6%) over the nominal concentration range in whole blood from 0.376 to 30 ng/mL.
Elimination
After administration of ZURNAI to healthy adult subjects, plasma concentrations have a terminal elimination half-life of 9.07 (%CV 26.2) hours. Following a 1 mg parenteral dose, the apparent clearance of nalmefene is 55.46 (%CV 8.41) L/hr.
Metabolism
Nalmefene is metabolized by the liver, primarily by glucuronide conjugation.
Nalmefene is also metabolized to trace amounts of an N-dealkylated metabolite. Nalmefene glucuronide is inactive and the N-dealkylated metabolite has minimal pharmacological activity.
Excretion
Nalmefene and its metabolites are excreted in the urine. Less than 5% of nalmefene is excreted in the urine unchanged. Seventeen percent (17%) of the nalmefene dose is excreted in the feces. The plasma concentration-time profile in some subjects suggests that nalmefene undergoes enterohepatic recycling.
Specific Populations
Geriatric Population
In previous studies with nalmefene hydrochloride injection, dose proportionality was observed in nalmefene AUC0-inf following 0.5 to 2 mg intravenous administration to elderly male subjects. Following a 1 mg intravenous nalmefene dose, there were no significant differences between young (19 to 32 years) and elderly (62 to 80 years) adult male subjects with respect to plasma clearance, steady-state volume of distribution, or half-life. There was an apparent age-related decrease in the central volume of distribution (young: 3.9 ± 1.1 L/kg, elderly: 2.8 ± 1.1 L/kg) that resulted in a greater initial nalmefene concentration in the elderly group. While initial nalmefene plasma concentrations were transiently higher in the elderly, it would not be anticipated that this population would require dosing adjustment. No clinical adverse events were noted in the elderly following the 1 mg intravenous nalmefene dose.
Pediatric Patients
No pharmacokinetic studies were conducted with ZURNAI in pediatric patients. Based on population PK simulations, compared to an adult population (mean weight 76 kg), 12-year-old subjects with a median weight 49 kg, range 33 to 71 kg are expected to have 27% higher mean Cmax and 15% higher mean AUC0-∞ [See Use in Specific Populations (8.4)].
Male and Female Patients
There is insufficient experience with the use of nalmefene hydrochloride injection to detect sex variations in pharmacokinetics.
Patients with Renal Impairment
The pharmacokinetics of ZURNAI have not been studied in renally impaired subjects. In previous studies with nalmefene hydrochloride injection, there was a statistically significant 27% decrease in plasma clearance of nalmefene in the end-stage renal disease (ESRD) population during interdialysis (0.57 ± 0.20 L/hr/kg) and a 25% decreased plasma clearance in the ESRD population during intradialysis (0.59 ± 0.18 L/hr/kg) compared to normal patients (0.79 ± 0.24 L/hr/kg). The elimination half-life was prolonged in ESRD patients from 10.2 ± 2.2 hours in normal patients to 26.1 ± 9.9 hours.
Patients with Hepatic Impairment
The pharmacokinetics of ZURNAI have not been studied in hepatically impaired subjects. In previous studies with nalmefene hydrochloride injection, in subjects with hepatic disease, when compared to matched normal controls, had a 28.3% decrease in plasma clearance of nalmefene (0.56 ± 0.21 L/hr/kg versus 0.78 ± 0.24 L/hr/kg, respectively). Elimination half-life increased from 10.2 ± 2.2 hours to 11.9 ± 2.0 hours in the hepatically impaired. No dosage adjustment is recommended since nalmefene will be administered as an acute course of therapy.
Low Body Weight Patients and High Body Weight Patients
The effect of weight on nalmefene PK following a single dose of 1.5 mg ZURNAI administration was assessed using population pharmacokinetic simulations. Compared to the mean PK values across the full population in the PK dataset (median weight 76 kg), the 1st quartile of body weight (54.0 to 67.3 kg) had + 17.6% higher Cmax and + 13.4% higher AUC0-∞ whereas the 4th quartile of body weight (86.8 to 117.1 kg) had – 15.3% lower Cmax and – 11.8% lower AUC0-∞.
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Long-term animal studies to evaluate the carcinogenic potential of nalmefene have not been completed.
Mutagenesis
Nalmefene did not have mutagenic activity in the Ames test with five bacterial strains or the mouse lymphoma assay. Clastogenic activity was not observed in the mouse micronucleus test or in the cytogenic bone marrow assay in rats. However, nalmefene did exhibit a weak but significant clastogenic activity in the human lymphocyte metaphase assay in the absence but not in the presence of exogenous metabolic activation.
16. How is Zurnai supplied
16.1 How Supplied
Each single-dose auto-injector delivers 1.5 mg of nalmefene in 0.5 mL. Each carton contains one single-dose ZURNAI (nalmefene injection).
NDC 59011-962-01: One carton containing one single-dose auto-injector.
ZURNAI is not made with natural rubber latex.
16.2 Storage and Handling
Store at controlled room temperature 20°C to 25°C (68°F to 77°F), with excursions permitted between 15°C and 30°C (59°F and 86°F).
During storage, check ZURNAI through the viewing window of the auto-injector every 30 days. The liquid should be clear, colorless to light yellow. If the ZURNAI liquid is discolored, cloudy, or contains solid particles, replace it with a new ZURNAI.
DO NOT FREEZE OR REFRIGERATE. Store in a clean dry place. Protect from light.
Keep ZURNAI in the carton until use.
Store ZURNAI securely and dispose of properly in a sharps container. For detailed disposal instructions, see the Instructions for Use.
KEEP ZURNAI AND ALL MEDICINES OUT OF THE REACH OF CHILDREN.
Before using, check to make sure the solution in the auto-injector is not discolored. Replace ZURNAI if the solution is discolored or contains a precipitate.
Each ZURNAI can only be used one time and cannot be re-used.
17. Patient Counseling Information
Advise the patient and family members or caregivers to read the FDA-approved patient labeling (Patient Information and Instructions for Use).
Instruct patients and their family members or caregivers to become familiar with all information contained in the carton as soon as they receive ZURNAI.
Recognition of Opioid Overdose
Instruct patients and their family members or caregivers about how to recognize the signs and symptoms of an opioid overdose, such as the following:
- Extreme somnolence – inability to awaken a patient verbally or upon a firm sternal rub
- Respiratory depression – this can range from slow or shallow respiration to no respiration in a patient who is unarousable
- Other signs and symptoms that may accompany somnolence and respiratory depression include the following:
- Miosis
- Bradycardia and/or hypotension
Risk of Recurrent Respiratory and Central Nervous System Depression
While the duration of action of nalmefene is as long as most opioids, instruct patients and their family members or caregivers that they must seek immediate emergency medical assistance after administration of the first dose of ZURNAI, and keep the patient under continued surveillance even after an apparently adequate initial response to ZURNAI. A second dose may be necessary if there is recurrence of symptoms of opioid overdose [see Dosage and Administration (2.2), Warnings and Precautions (5.1)].
Limited Efficacy for/with Partial Agonists or Mixed Agonist/Antagonists
Instruct patients and their family members or caregivers that the reversal of respiratory depression caused by partial agonists or mixed agonist/antagonists, such as buprenorphine and pentazocine, may be incomplete and may require repeated administration of ZURNAI, using a new ZURNAI auto-injector each time [see Dosage and Administration (2.2), Warnings and Precautions (5.2)].
Precipitation of Severe Opioid Withdrawal
Instruct patients and their family members or caregivers that the use of ZURNAI in patients who are opioid dependent may precipitate opioid withdrawal [see Warnings and Precautions (5.3), Adverse Reactions (6)].
Administration Instructions
Instruct patients and their family member or caregivers to:
- Ensure ZURNAI is readily available in locations where persons may be intentionally or accidentally exposed to an opioid overdose (i.e., opioid emergencies).
- Use ZURNAI one time only. DO NOT test or prime prior to use [see Dosage and Administration (2.1)].
- Carefully read the Instructions for Use that comes with ZURNAI.
- Administer ZURNAI as quickly as possible if a person is unresponsive and an opioid overdose is suspected, even when in doubt, because prolonged respiratory depression may result in damage to the central nervous system or death. ZURNAI is not a substitute for emergency medical care [see Dosage and Administration (2.1)].
- Administer ZURNAI directly into the outer thigh. Press the needle end firmly into the injection site (through clothing, if necessary) and hold for 3 seconds [see Dosage and Administration (2.1)]. After 3 seconds, the viewing window should turn completely orange, signaling that ZURNAI has delivered the intended dose of nalmefene.
- Remove ZURNAI from the outer thigh.
- Call 911 immediately after injecting the first dose of ZURNAI.
- Move the person to the recovery position by turning them to their side. Additional supportive and/or resuscitative measures may be helpful while awaiting emergency medical assistance [see Dosage and Administration (2.1)].
- Watch the person carefully. Wait 2 to 5 minutes to see if the person wakes up.
- If the person is not responding or responds and then relapses back into respiratory depression, administer additional doses of ZURNAI every 2 to 5 minutes using a new ZURNAI auto-injector [see Dosage and Administration (2.1)].
- Remain with the person until emergency medical help arrives, even if they wake up.
- Visually inspect the nalmefene solution through the viewing window every 30 days. If the solution is discolored, cloudy, or contains solid particles, replace it with a new ZURNAI.
- Replace ZURNAI before its expiration date.
| PATIENT INFORMATION ZURNAI™ (zur nye) (nalmefene injection) |
||||
|---|---|---|---|---|
| This Patient Information has been approved by the U.S. Food and Drug Administration. | Issued: 08/2024 | |||
| You and your family members or caregivers should read this Patient Information leaflet before an opioid emergency happens. This information does not take the place of talking with your healthcare provider about your medical condition or your treatment. | ||||
| What is the most important information I should know about ZURNAI?
ZURNAI is used to temporarily reverse the effects of opioid medicines. The medicine in ZURNAI is not expected to have an effect in people who are not taking opioid medicines. Always carry ZURNAI with you in case of an opioid emergency.
|
||||
What is ZURNAI?
|
||||
| Do not use ZURNAI if you are allergic to nalmefene hydrochloride or any of the ingredients in ZURNAI. See the end of this Patient Information leaflet for a complete list of ingredients in ZURNAI. | ||||
Before using ZURNAI, tell your healthcare provider about all of your medical conditions, including if you:
|
||||
| How should I use ZURNAI? Read the "Instructions for Use" at the end of this Patient Information leaflet for detailed information about the right way to use ZURNAI.
|
||||
| What are the possible side effects of ZURNAI? ZURNAI may cause serious side effects, including: |
||||
|
||||
|
|
|
||
|
||||
| The most common side effects of ZURNAI include: | ||||
|
|
|
||
| These are not all of the possible side effects of ZURNAI. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. |
||||
How should I store ZURNAI?
|
||||
| General information about the safe and effective use of ZURNAI.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use ZURNAI for a condition for which it was not prescribed. You can ask your pharmacist or healthcare provider for information about ZURNAI that is written for health professionals. |
||||
| What are the ingredients in ZURNAI?
Active ingredient: nalmefene Inactive ingredients: hydrochloric acid to adjust pH, magnesium chloride, and water for injection. ZURNAI is not made with natural rubber latex. |
||||
| Manufactured for: Purdue Pharma L.P., Stamford, CT 06901-3431. For more information, go to www.ZURNAI.com or call 1-888-726-7535. |
||||
INSTRUCTIONS FOR USE
ZURNAI™ (zur nye)
(nalmefene injection)
The Instructions for Use contains information on how to give ZURNAI in response to a known or suspected opioid overdose in adults and children 12 years of age and older. You and your family members or caregivers should read the Instructions for Use that comes with ZURNAI before using it. Talk to your healthcare provider if you and your family members or caregivers have any questions about the use of ZURNAI.
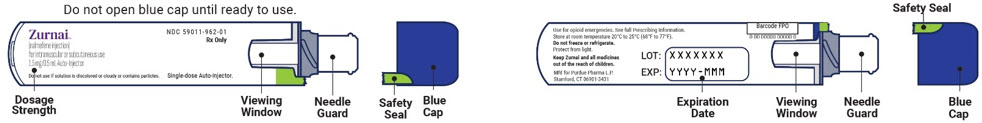
ZURNAI auto-injector parts:
 |
Important information you need to know before injecting ZURNAI
- The ZURNAI auto-injector is ready to use. Do not test or prime ZURNAI before use.
- Each ZURNAI auto-injector contains 1 dose of medicine and cannot be reused.
- Inject ZURNAI into the muscle (intramuscular) or underneath the skin (subcutaneous) of the outer thigh. Do not inject into any other area of the body.
Preparing to inject ZURNAI
-
Check person for signs of a suspected overdose:
- will not wake to voice or touch
- very sleepy
- not breathing well
- Check the auto-injector label to make sure you are injecting ZURNAI.
- Check for any visible damage to the auto-injector before using.
- Check the auto-injector to make sure the safety seal is not broken and the blue cap is secure and not missing.
- Check the liquid through the viewing window before using. It should be clear, colorless to light-yellow and free of particles. You may see air bubbles. This is normal.
Injecting ZURNAI
| 1. Remove the blue cap | |
| 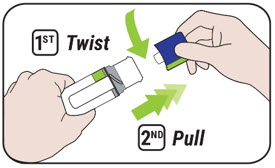 |
| 2. Position and inject | |
|  |
| 3. Inspect the viewing window | |
| 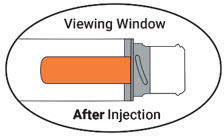 |
| 4. Call 911 and watch the person | |
|
|
  |
|
| 5. Throw away (dispose of) the used ZURNAI auto-injector | |
Disposing of (throwing away) ZURNAI
|  |
| Important: Always keep the sharps disposal container out of the reach of children. | |
| Storing ZURNAI |
|
| Manufactured for Purdue Pharma L.P., Stamford CT, 06901-3431. ©2024, Purdue Pharma L.P., Stamford CT 06901-3431 For more information go to www.ZURNAI.com or call 1-888-726-7535. This Instructions for Use has been approved by the U.S. Food and Drug Administration. | Issued: 08/2024 |
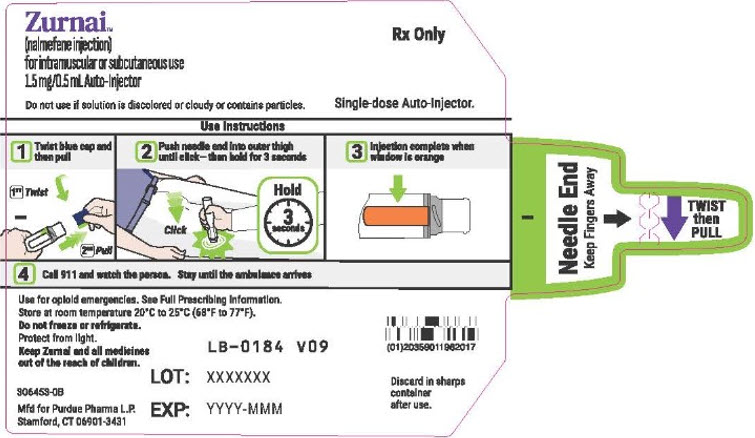
PRINCIPAL DISPLAY PANEL - 1.5 mg/0.5 mL Auto-Injector Label
Zurnai™
(nalmefene injection)
for intramuscular or subcutaneous use
1.5 mg/0.5 mL Auto-Injector
Do not use if solution is discolored or cloudy or contains particles.
Rx Only
Single-dose Auto-Injector.
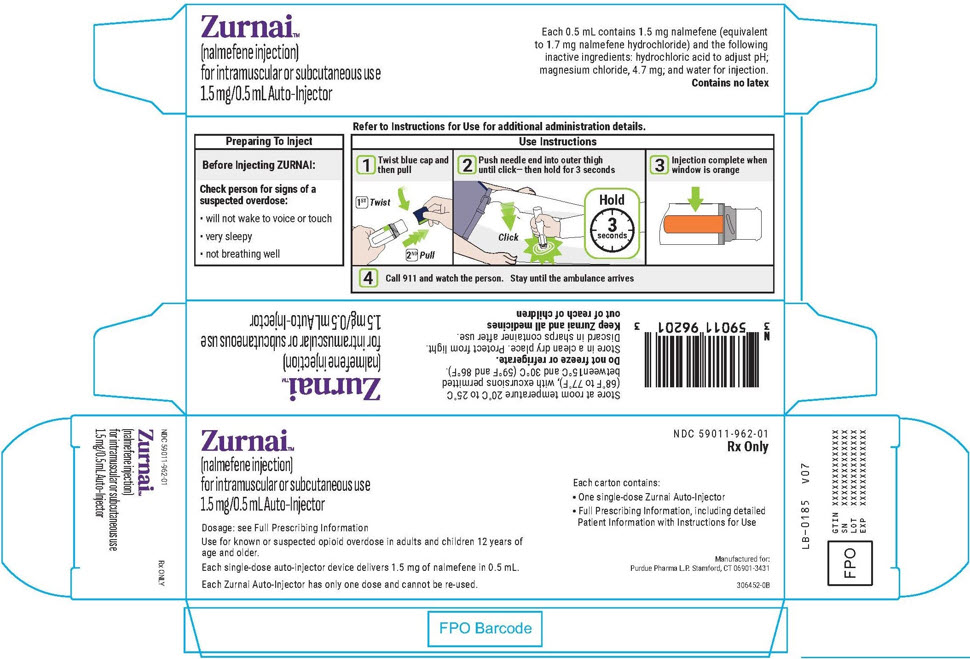
PRINCIPAL DISPLAY PANEL - 1.5 mg/0.5 mL Auto-Injector Carton
Zurnai™
(nalmefene injection)
for intramuscular or subcutaneous use
1.5 mg/0.5 mL Auto-Injector
Dosage: see Full Prescribing Information
Use for known or suspected opioid overdose in adults and children 12 years of
age and older.
Each single-dose auto-injector device delivers 1.5 mg of nalmefene in 0.5 mL.
Each Zurnai Auto-Injector has only one dose and cannot be re-used.
NDC 59011-962-01
Rx Only
Each carton contains:
- One single-dose Zurnai Auto-Injector
- Full Prescribing Information, including detailed
Patient Information with Instructions for Use
Manufactured for:
Purdue Pharma L.P. Stamford, CT 06901-3431
306452-0B
| ZURNAI
nalmefene hydrochloride injection, solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Purdue Pharma L.P. (932323652) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| ANTARES PHARMA, INC. | 118083911 | MANUFACTURE(59011-962) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Pharmascience Inc | 202657094 | MANUFACTURE(59011-962) | |
More about Zurnai (nalmefene)
- Check interactions
- Compare alternatives
- Side effects
- Dosage information
- During pregnancy
- FDA approval history
- Drug class: antidotes
- Breastfeeding

