Ramipril (Monograph)
Brand name: Altace
Drug class: Angiotensin-Converting Enzyme Inhibitors
- ACE Inhibitors
VA class: CV800
Chemical name: [2S-[1[R*(R*)],2α,3aβ,6aβ]]-1-[2-[[1-(Ethoxycarbonyl)-3-phenylpropyl]amino]-1-oxopropy l]octahydrocylopenta[b]pyrrole-2-carboxylic acid
Molecular formula: C21H28N2O5
CAS number: 87333-19-5
Warning
Introduction
Nonsulfhydryl ACE inhibitor.1 2 3
Uses for Ramipril
Hypertension
Management of hypertension (alone or in combination with other classes of antihypertensive agents).1 2 4 1200
ACE inhibitors are recommended as one of several preferred agents for the initial management of hypertension according to current evidence-based hypertension guidelines; other preferred options include angiotensin II receptor antagonists, calcium-channel blockers, and thiazide diuretics.501 502 503 504 1200 While there may be individual differences with respect to recommendations for initial drug selection and use in specific patient populations, current evidence indicates that these antihypertensive drug classes all generally produce comparable effects on overall mortality and cardiovascular, cerebrovascular, and renal outcomes.501 502 504 1200 1213
Individualize choice of therapy; consider patient characteristics (e.g., age, ethnicity/race, comorbidities, cardiovascular risk) as well as drug-related factors (e.g., ease of administration, availability, adverse effects, cost).501 502 503 504 515 1200 1201
A 2017 ACC/AHA multidisciplinary hypertension guideline classifies BP in adults into 4 categories: normal, elevated, stage 1 hypertension, and stage 2 hypertension.1200 (See Table 1.)
Source: Whelton PK, Carey RM, Aronow WS et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13-115.
Individuals with SBP and DBP in 2 different categories (e.g., elevated SBP and normal DBP) should be designated as being in the higher BP category (i.e., elevated BP).
|
Category |
SBP (mm Hg) |
DBP (mm Hg) |
|
|---|---|---|---|
|
Normal |
<120 |
and |
<80 |
|
Elevated |
120–129 |
and |
<80 |
|
Hypertension, Stage 1 |
130–139 |
or |
80–89 |
|
Hypertension, Stage 2 |
≥140 |
or |
≥90 |
The goal of hypertension management and prevention is to achieve and maintain optimal control of BP.1200 However, the BP thresholds used to define hypertension, the optimum BP threshold at which to initiate antihypertensive drug therapy, and the ideal target BP values remain controversial.501 503 504 505 506 507 508 515 523 526 530 1200 1201 1207 1209 1222 1223 1229
The 2017 ACC/AHA hypertension guideline generally recommends a target BP goal (i.e., BP to achieve with drug therapy and/or nonpharmacologic intervention) of <130/80 mm Hg in all adults regardless of comorbidities or level of atherosclerotic cardiovascular disease (ASCVD) risk.1200 In addition, an SBP goal of <130 mm Hg generally is recommended for noninstitutionalized ambulatory patients ≥65 years of age with an average SBP of ≥130 mm Hg.1200 These BP goals are based upon clinical studies demonstrating continuing reduction of cardiovascular risk at progressively lower levels of SBP.1200 1202 1210
Other hypertension guidelines generally have based target BP goals on age and comorbidities.501 504 536 Guidelines such as those issued by the JNC 8 expert panel generally have targeted a BP goal of <140/90 mm Hg regardless of cardiovascular risk and have used higher BP thresholds and target BPs in elderly patients501 504 536 compared with those recommended by the 2017 ACC/AHA hypertension guideline.1200
Some clinicians continue to support previous target BPs recommended by JNC 8 due to concerns about the lack of generalizability of data from some clinical trials (e.g., SPRINT study) used to support the current ACC/AHA hypertension guideline and potential harms (e.g., adverse drug effects, costs of therapy) versus benefits of BP lowering in patients at lower risk of cardiovascular disease.1222 1223 1224 1229
Consider potential benefits of hypertension management and drug cost, adverse effects, and risks associated with the use of multiple antihypertensive drugs when deciding a patient’s BP treatment goal.1200 1220
For decisions regarding when to initiate drug therapy (BP threshold), the current ACC/AHA hypertension guideline incorporates underlying cardiovascular risk factors.1200 1207 ASCVD risk assessment recommended by ACC/AHA for all adults with hypertension.1200
ACC/AHA currently recommend initiation of antihypertensive drug therapy in addition to lifestyle/behavioral modifications at an SBP ≥140 mm Hg or DBP ≥90 mm Hg in adults who have no history of cardiovascular disease (i.e., primary prevention) and a low ASCVD risk (10-year risk <10%).1200
For secondary prevention in adults with known cardiovascular disease or for primary prevention in those at higher risk for ASCVD (10-year risk ≥10%), ACC/AHA recommend initiation of antihypertensive drug therapy at an average SBP ≥130 mm Hg or an average DBP ≥80 mm Hg.1200
Adults with hypertension and diabetes mellitus, chronic kidney disease (CKD), or age ≥65 years are assumed to be at high risk for cardiovascular disease; ACC/AHA state that such patients should have antihypertensive drug therapy initiated at a BP ≥130/80 mm Hg.1200 Individualize drug therapy in patients with hypertension and underlying cardiovascular or other risk factors.502 1200
In stage 1 hypertension, experts state that it is reasonable to initiate drug therapy using the stepped-care approach in which one drug is initiated and titrated and other drugs are added sequentially to achieve the target BP.1200 Initiation of antihypertensive therapy with 2 first-line agents from different pharmacologic classes recommended in patients with stage 2 hypertension and average BP >20/10 mm Hg above BP goal.1200
Black hypertensive patients generally tend to respond better to monotherapy with calcium-channel blockers or thiazide diuretics than to ACE inhibitors.14 67 68 86 87 501 504 1200 However, the combination of an ACE inhibitor or an angiotensin II receptor antagonist with a calcium-channel blocker or thiazide diuretic produces similar BP lowering in black patients as in other racial groups.1200
ACE inhibitors may be preferred in hypertensive patients with heart failure, ischemic heart disease, diabetes mellitus, CKD, or cerebrovascular disease or post-MI.501 502 504 523 524 525 526 527 534 535 536 543 1200 1214 1215
Heart Failure After Acute MI
Reduction of the risk of mortality in hemodynamically stable patients who have demonstrated clinical signs of heart failure within a few days following acute MI.1 2 12 18 21 24 27 28 524 Also may reduce rate of heart failure-associated hospitalization and progression to severe and/or resistant heart failure.1 2 12 18 21 24 27 28 524
Expert guidelines recommend initiation of an oral ACE inhibitor within the first 24 hours of acute MI in patients with an anterior infarct, heart failure, or ejection fraction ≤40% who do not have any contraindications (e.g., hypotension, shock, renal dysfunction).527 Use with caution (and with gradual upward titration) during initial postinfarction period because of the possibility of hypotension or renal dysfunction.527 1100
Continue therapy indefinitely in patients with left ventricular dysfunction or other compelling indications (e.g., hypertension, diabetes mellitus, CKD).525 1100
Prevention of Major Cardiovascular Events
Reduction of the risk of cardiovascular death, MI, and stroke in patients ≥55 years of age who are at high risk for cardiovascular events (e.g., those with a history of CAD, stroke, peripheral vascular disease, or diabetes mellitus in addition to ≥1 other cardiovascular risk factor [e.g., hypertension, elevated total cholesterol and/or decreased HDL-cholesterol concentrations, smoking, documented microalbuminuria]) but who are not known to have low ventricular ejection fraction or heart failure.1 47 48
Reduction in the incidence of diabetic complications and in new diagnosis of diabetes also reported.47 48
Heart Failure
Management of heart failure† [off-label], usually in conjunction with other agents such as cardiac glycosides, diuretics, and β-adrenergic blocking agents (β-blockers).70 71 72 73 74 524 800
Some evidence indicates that therapy with an ACE inhibitor (enalapril) may be less effective than angiotensin receptor-neprilysin inhibitor (ARNI) therapy (e.g., sacubitril/valsartan) in reducing cardiovascular death and heart failure-related hospitalization.702 800
ACCF, AHA, and the Heart Failure Society of America (HFSA) recommend that patients with chronic symptomatic heart failure and reduced left ventricular ejection fraction (LVEF) (NYHA class II or III) who are able to tolerate an ACE inhibitor or angiotensin II receptor antagonist be switched to therapy containing an ARNI to further reduce morbidity and mortality.701 800
Diabetic Nephropathy
A recommended agent in the management of patients with diabetes mellitus and persistent albuminuria† [off-label] who have modestly elevated (30–300 mg/24 hours) or higher (>300 mg/24 hours) levels of urinary albumin excretion; slows rate of progression of renal disease in such patients.81 82 83 84 85 535 536 1232
Ramipril Dosage and Administration
General
BP Monitoring and Treatment Goals
-
Monitor BP regularly (i.e., monthly) during therapy and adjust dosage of the antihypertensive drug until BP controlled.1200
-
If unacceptable adverse effects occur, discontinue drug and initiate another antihypertensive agent from a different pharmacologic class.1216
-
If adequate BP response not achieved with a single antihypertensive agent, either increase dosage of single drug or add a second drug with demonstrated benefit and preferably a complementary mechanism of action (e.g., calcium-channel blocker, thiazide diuretic).1200 1216 Many patients will require at least 2 drugs from different pharmacologic classes to achieve BP goal; if goal BP still not achieved, add a third drug.1200 1216 1220
Administration
Oral Administration
Administer orally once or twice daily.1
Swallow capsules whole.1 Alternatively, open capsules and sprinkle contents on small amount (about 120 mL) of applesauce or mix in 120 mL of water or apple juice.1 Consume entire mixture to ensure that no drug is lost.1 (See Storage under Stability.)
Dosage
In patients currently receiving diuretic therapy, discontinue diuretic, reduce diuretic dosage, or increase salt intake prior to initiating ramipril.600 If such changes are not possible, initiate ramipril in adults at a reduced dosage of 1.25 mg once daily.600 (See Hypotension under Cautions and see the individual dosage sections in Dosage and Administration.)
Adults
Hypertension
Oral
Initially, 2.5 mg once daily in patients not receiving diuretic therapy.600 In patients receiving a diuretic, initiate ramipril at 1.25 mg once daily.600 Adjust subsequent dosage based on BP response.600
Usual maintenance dosage: 2.5–20 mg daily, given in 1 dose or 2 divided doses.600 1200
If effectiveness diminishes toward end of dosing interval in patients treated once daily, consider increasing dosage or administering drug in 2 divided doses.600
Heart Failure After Acute MI
Oral
Initially, 2.5 mg twice daily.1 12 Some clinicians recommend initiation of therapy within the first 24 hours following MI.527 If hypotension occurs, reduce dosage to 1.25 mg twice daily.1 After 1 week at initial dosage, adjust dosage as tolerated at 3-week intervals to target dosage of 5 mg twice daily.1
Following initial dose, monitor closely for ≥2 hours and until BP has stabilized for at least an additional hour.1 To minimize risk of hypotension, reduce diuretic dosage, if possible.1
Prevention of Major Cardiovascular Events
Oral
Initially, 2.5 mg once daily for 1 week, followed by 5 mg once daily for 3 weeks; subsequently increase dosage as tolerated to maintenance dosage of 10 mg once daily.1 In patients with hypertension or those with recent MI, may administer total daily dosage in divided doses.1
Heart Failure† [off-label]
Oral
Initially, 1.25–2.5 mg once daily recommended by ACCF and AHA in patients with prior or current symptoms of chronic heart failure and reduced LVEF (ACCF/AHA stage C heart failure).524
Titrate dosage slowly upward as tolerated to dosages shown to reduce the risk of cardiovascular events in clinical trials; may use intermediate doses if such target dosages cannot be achieved or are poorly tolerated.524
ACCF and AHA recommend maximum ramipril dosage of 10 mg once daily for patients with ACCF/AHA stage C heart failure.524
Special Populations
Renal Impairment
Initial dosage of 1.25 mg once daily recommended in patients with renal artery stenosis.1
In patients with Clcr <40 mL/minute, 25% of the usual doses are expected to induce full therapeutic concentrations of ramiprilat.1
Hypertension
Oral
Initially, 1.25 mg once daily in patients with Clcr <40 mL/minute.1 Titrate until BP is controlled or to maximum dosage of 5 mg daily.1
Heart Failure After Acute MI
Oral
Initially, 1.25 mg once daily in patients with Clcr <40 mL/minute.1 May increase dosage to 1.25 mg twice daily; subsequently titrate according to clinical response and tolerance up to maximum dosage of 2.5 mg twice daily.1
Volume-and/or Salt-Depleted Patients
Correct volume and/or salt depletion prior to initiation of therapy or initiate therapy at dosage of 1.25 mg once daily.1
Cautions for Ramipril
Contraindications
-
Known hypersensitivity (e.g., history of angioedema) to ramipril or another ACE inhibitor.1
-
Concomitant use of ramipril and aliskiren in patients with diabetes mellitus.550 600 (See Specific Drugs under Interactions.)
Warnings/Precautions
Warnings
Hepatic Effects
Clinical syndrome that usually is manifested initially by cholestatic jaundice and may progress to fulminant hepatic necrosis (occasionally fatal) reported rarely with ACE inhibitors.1
If jaundice or marked elevation of liver enzymes occurs, discontinue drug and monitor patient.1
Hypotension
Possible symptomatic hypotension, particularly in volume- and/or salt-depleted patients (e.g., those receiving prolonged diuretic therapy or undergoing dialysis, those with dietary salt restriction, patients with diarrhea or vomiting).1 Risk of excessive hypotension, sometimes associated with oliguria, azotemia, and, rarely, acute renal failure and death in patients with heart failure with or without associated renal insufficiency.1
Hypotension may occur in patients undergoing surgery or during anesthesia with agents that produce hypotension; recommended treatment is fluid volume expansion.1
To minimize potential for hypotension, consider recent antihypertensive therapy, extent of BP elevation, sodium intake, fluid status, and other clinical circumstances.1 Correct volume and/or salt depletion (e.g., by withholding diuretic therapy, reducing diuretic dosage, increasing sodium intake) prior to initiation of ramipril or reduce initial dosage.1 600 (See Dosage and also Special Populations, under Dosage and Administration.)
In patients at risk of excessive hypotension, initiate therapy under close medical supervision; monitor closely for first 2 weeks following initiation of ramipril or any increase in ramipril or diuretic dosage.1
If hypotension occurs, place patient in supine position and, if necessary, administer IV infusion of physiological saline.1 Ramipril therapy usually can be continued following restoration of volume and BP.1
Hematologic Effects
Neutropenia and agranulocytosis reported with captopril; risk appears to depend principally on presence of renal impairment and/or presence of collagen vascular disease (e.g., systemic lupus erythematosus, scleroderma);1 also reported in patients receiving immunosuppressive therapy.5 6 Hematologic effects (e.g., agranulocytosis; pancytopenia; bone marrow depression; reductions in hemoglobin content or leukocyte, erythrocyte, or platelet counts) reported rarely with ramipril.1
Consider monitoring leukocytes in patients with collagen vascular disease, especially if renal impairment exists.1
Fetal/Neonatal Morbidity and Mortality
Possible fetal and neonatal morbidity and mortality when used during pregnancy.1 88 89 (See Boxed Warning.) Such potential risks occur throughout pregnancy, especially during the second and third trimesters.89
Also may increase the risk of major congenital malformations when administered during the first trimester of pregnancy.88 89
Discontinue as soon as possible when pregnancy is detected, unless continued use is considered lifesaving.89 Nearly all women can be transferred successfully to alternative therapy for the remainder of their pregnancy.44 46
Sensitivity Reactions
Anaphylactoid reactions and/or head and neck angioedema possible; if associated with laryngeal edema, may be fatal.1 Immediate medical intervention (e.g., epinephrine) for involvement of tongue, glottis, or larynx.1
Intestinal angioedema possible; consider in differential diagnosis of patients who develop abdominal pain.1
Increased risk for angioedema also reported with concomitant mammalian target of rapamycin (mTOR) inhibitor (e.g., temsirolimus) therapy.600
Anaphylactoid reactions reported in patients receiving ACE inhibitors while undergoing LDL apheresis with dextran sulfate absorption or following initiation of hemodialysis that utilized high-flux membrane.1
Life-threatening anaphylactoid reactions reported in at least 2 patients receiving ACE inhibitors while undergoing desensitization treatment with hymenoptera venom.1
Contraindicated in patients with a history of angioedema associated with ACE inhibitors.1 47 Patients with history of angioedema unrelated to ACE inhibitors may be at increased risk of angioedema associated with ACE inhibitor therapy.1
General Precautions
Renal Effects
Transient increases in BUN and Scr possible, especially in patients with preexisting renal impairment or those receiving concomitant diuretic therapy.1 Possible increases in BUN and Scr in patients with unilateral or bilateral renal artery stenosis; generally reversible following discontinuance of ramipril and/or diuretic therapy.1
Possible oliguria, progressive azotemia, and, rarely, acute renal failure and/or death in patients with severe heart failure.1
Closely monitor renal function for the first few weeks of therapy in hypertensive patients with unilateral or bilateral renal-artery stenosis.1 Some patients may require dosage reduction or discontinuance of ACE inhibitor or diuretic therapy.1
Hyperkalemia
Possible hyperkalemia, especially in patients with renal impairment or diabetes mellitus and those receiving drugs that can increase serum potassium concentration (e.g., potassium-sparing diuretics, potassium supplements, potassium-containing salt substitutes).1 (See Interactions.)
Cough
Persistent and nonproductive cough; resolves after drug discontinuance.1
Specific Populations
Pregnancy
Category C (1st trimester); Category D (2nd and 3rd trimesters).1 (See Fetal/Neonatal Morbidity and Mortality under Cautions and see Boxed Warning.)
Lactation
Undetectable in human milk following single oral dose; not known whether distributed into milk following multiple doses.1 Use not recommended.1
Pediatric Use
Safety and efficacy not established in children <18 years of age.1
Geriatric Use
No substantial differences in safety and efficacy relative to younger adults, but increased sensitivity cannot be ruled out.1
Hepatic Impairment
Use with caution in patients with cirrhosis and/or ascites, due to possible increased activity of renin-angiotensin-aldosterone system.1
Possible marked increase in plasma ramipril concentrations; peak plasma ramiprilat concentrations not appreciably altered. (See Absorption: Special Populations, under Pharmacokinetics.)1
Renal Impairment
Systemic exposure to ramiprilat may be increased.1 (See Pharmacokinetics.) Initial dosage adjustment may be necessary depending on degree of renal impairment.1 (See Renal Impairment under Dosage and Administration.)
Deterioration of renal function may occur.1 (See Renal Effects under Cautions.)
Black Patients
BP reduction may be smaller in black patients compared with nonblack patients.1 14 15 67 68 (See Hypertension under Uses.)
Higher incidence of angioedema reported with ACE inhibitors in black patients compared with other races.1 68 1200
Common Adverse Effects
Patients with hypertension: Headache, dizziness, fatigue.1
Patients with heart failure: Dizziness, cough, nausea, vomiting, angina pectoris, syncope, postural hypotension, vertigo, hypotension.1
Drug Interactions
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
ACE inhibitors |
Increased risk of renal impairment, hyperkalemia, and hypotensiona |
Generally avoid concomitant use; monitor BP, renal function, and electrolytes if used concomitantlya |
|
Aliskiren |
Increased risk of renal impairment, hyperkalemia, and hypotensiona 550 |
Generally avoid concomitant use; monitor BP, renal function, and electrolytes if used concomitantlya 550 Concomitant use contraindicated in patients with diabetes mellitusa 550 Avoid concomitant use in patients with GFR <60 mL/minutea 550 |
|
Angiotensin II receptor antagonists |
Increased risk of renal impairment, hyperkalemia, and hypotensiona |
Generally avoid concomitant use; monitor BP, renal function, and electrolytes if used concomitantlya |
|
Antacid |
Pharmacokinetic interaction unlikely1 |
|
|
Antidiabetic agents (insulin, oral agents) |
Possible hypoglycemia in diabetic patients1 |
Monitor closely for symptoms of hypoglycemia following initiation or dosage adjustment of ramipril; adjust dosage of antidiabetic agent as necessary1 |
|
Cimetidine |
Pharmacokinetic interaction unlikely1 |
|
|
Digoxin |
Pharmacokinetic interaction unlikely1 |
|
|
Diuretics |
Increased hypotensive effect1 |
If possible, discontinue or decrease dosage of diuretic before initiating ramipril600 (see Dosage and also Special Populations, under Dosage and Administration) |
|
Diuretics, potassium-sparing (amiloride, spironolactone, triamterene) |
Enhanced hyperkalemic effect1 |
Use with caution; monitor serum potassium concentrations frequently1 |
|
Lithium |
Increased serum lithium concentrations; possible toxicity1 |
Use with caution; monitor serum lithium concentrations frequently1 |
|
Mammalian target of rapamycin (mTOR) inhibitors (e.g., temsirolimus) |
Increased risk for angioedema600 |
|
|
NSAIAs |
Potential for reduction of renal function and increase in serum potassium1 No interaction observed with indomethacin1 |
|
|
Potassium supplements or potassium-containing salt substitutes |
Enhanced hyperkalemic effect1 |
Use with caution; monitor serum potassium concentrations frequently1 |
|
Simvastatin |
Pharmacokinetic interaction unlikely1 |
|
|
Warfarin |
Pharmacologic interaction unlikely1 |
Ramipril Pharmacokinetics
Absorption
Bioavailability
Following oral administration, peak plasma concentrations of ramipril usually attained within 1 hour.1 Peak plasma concentrations of ramiprilat attained within 2–4 hours after oral dose.1 About ≥50–60% of an oral dose is absorbed.1
Onset
Following multiple oral doses (≥2 mg), >90% inhibition of plasma ACE activity achieved 4 hours after dosing.1
Duration
Following multiple oral doses (≥2 mg), inhibition of >80% of plasma ACE activity persists for about 24 hours.1
Food
Food decreases rate but not extent of absorption.1 Opening the capsules and sprinkling the contents on applesauce or mixing the contents in apple juice does not alter serum concentrations of ramiprilat.1 (See Oral Administration under Dosage and Administration.)
Special Populations
In patients with hepatic impairment, plasma concentrations of ramipril are increased; peak plasma ramiprilat concentrations are similar to those in individuals with normal hepatic function.1
In patients with renal impairment (Clcr <40 mL/minute per 1.73 m2), plasma concentrations and AUC of ramiprilat are increased, and time to peak plasma ramiprilat concentrations is slightly prolonged.1
Distribution
Extent
Distributes into a large peripheral compartment.1 Crosses the placenta.1 Undetectable in human milk following single oral dose; not known whether distributed into milk following multiple doses.1
Plasma Protein Binding
Ramipril: About 73%.1
Ramiprilat: About 56%.1
Elimination
Metabolism
Metabolized mainly in the liver, principally to an active metabolite, ramiprilat.1
Elimination Route
Excreted in urine (60%) as unchanged drug and ramiprilat and in feces (approximately 40%).1
Half-life
Triphasic; apparent elimination half-life of ramiprilat: Approximately 13–17 hours.1
Special Populations
In patients with Clcr <40 mL/minute per 1.73m2, urinary excretion of ramipril, ramiprilat, and their metabolites is decreased.1
Stability
Storage
Oral
Capsules
15–30 ºC.1
Mixtures of ramipril with applesauce, water, or apple juice (see Oral Administration under Dosage and Administration) are stable for 24 hours at room temperature and 48 hours when refrigerated.1
Actions
-
Prodrug; has little pharmacologic activity until metabolized to ramiprilat.1
-
Suppresses the renin-angiotensin-aldosterone system.1
Advice to Patients
-
Risk of angioedema, anaphylactoid reactions, or other sensitivity reactions.1 47 Importance of reporting sensitivity reactions (e.g., edema of face, eyes, lips, tongue, larynx, or extremities; hoarseness; swallowing or breathing with difficulty) immediately to clinician and of discontinuing the drug.1
-
Importance of reporting signs of infection (e.g., sore throat, fever).1
-
Risk of hypotension.1 Importance of informing clinicians promptly if lightheadedness or fainting occurs.1
-
Importance of adequate fluid intake; risk of volume depletion with excessive perspiration, dehydration, vomiting, or diarrhea.1
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs (including salt substitutes containing potassium).1
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.1
-
Importance of advising patients of other important precautionary information.1 (See Cautions.)
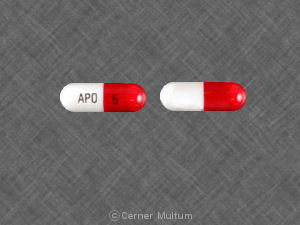
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules |
1.25 mg* |
Altace |
Pfizer |
|
Ramipril Capsules |
||||
|
2.5 mg* |
Altace |
Pfizer |
||
|
Ramipril Capsules |
||||
|
5 mg* |
Altace |
Pfizer |
||
|
Ramipril Capsules |
||||
|
10 mg* |
Altace |
Pfizer |
||
|
Ramipril Capsules |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions November 5, 2018. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
References
1. Monarch. Altace (ramipril) capsules prescribing information. Kansas City, MO; 2005 Sep.
2. Frampton JE, Peters DH. Ramipril: an updated review of its therapeutic use in essential hypertension and heart failure. Drugs. 1995;49:440-466.
3. Anon. Three new ACE inhibitors for hypertension. Med Lett Drugs Ther. 1991; 33:83-4. https://pubmed.ncbi.nlm.nih.gov/1831531
4. McAreavey D, Robertson JI. Angiotensin converting enzyme inhibitors and moderate hypertension. Drugs. 1990; 40:326-45. https://pubmed.ncbi.nlm.nih.gov/2226219
5. Squibb. Capoten (captopril) tablets prescribing information. In: Physician’s desk reference. 47th ed. Montvale, NJ: Medical Economics Company Inc; 1993:2356-62.
6. Reviewers’ comments on Enalaprilat/Enalapril 24:32.04 (personal observations).
8. Anon. Drugs for hypertension. Med Lett Drugs Ther. 1984; 26:107-12. https://pubmed.ncbi.nlm.nih.gov/6150424
10. US Food and Drug Administration. Dangers of ACE inhibitors during second and third trimesters of pregnancy. FDA Med Bull. 1992; 22:2.
12. The Acute Infarction Ramipril Efficacy (AIRE) Study Investigators. Effect of ramipril on mortality and morbidity of survivors of acute myocardial infarction with clinical evidence of heart failure. Lancet. 1993; 342:821-8. https://pubmed.ncbi.nlm.nih.gov/8104270
14. Saunders E. Tailoring treatment to minority patients. Am J Med. 1990; 88(Suppl 3B):21-23S. https://pubmed.ncbi.nlm.nih.gov/2294761
15. Chrysant SG, Danisa K, Kem DC et al. Racial differances in pressure, volume and renin interrelationships in essential hypertension. Hypertension. 1979; 1:136-41. https://pubmed.ncbi.nlm.nih.gov/399939
16. Holland OB, Kuhnert L, Campbell WB et al. Synergistic effect of captopril with hydrochlorothiazide for the treatment of low-renin hypertensive black patients. Hypertension. 1983; 5:235-9. https://pubmed.ncbi.nlm.nih.gov/6337951
17. Ferguson RK, Vlasses PH, Rotmesch HH. Clinical applications of angiotensin-enzyme inhibitors. Am J Med. 1984; 77:690-8. https://pubmed.ncbi.nlm.nih.gov/6091446
18. LeJemtel TH, Hochman JS, Sonnenblick EH. Indications for immedicate angiotensin-converting enzyme inhibition in patients with acute myocardial infarction. J Am Coll Cardiol. 1995; 25(Suppl):47-51S. https://pubmed.ncbi.nlm.nih.gov/7798525
19. Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto Miocardico. GISSI-3: effects of lisinopril and transdermal glyceryl trinitrate single and together on 6-week mortality and ventricular function after acute myocardial infarction. Lancet. 1994; 343:1115-22. https://pubmed.ncbi.nlm.nih.gov/7910229
20. Ambrosioni E, Borghi C, Magnani B for the Survival of Myocardial Infarction Long-Term Evaluation (SMILE) Study Investigators. The effect of the angiotensin-converting-enzyme inhibitor zofenopril on mortality and morbidity after anterior myocardial infarction. N Engl J Med. 1995; 332:80-5. https://pubmed.ncbi.nlm.nih.gov/7990904
21. Ball SG, Hall AS, Murray GD. Angiotensin-converting enzyme inhibitors after myocardial infarction: indications and timing. J Am Coll Cardiol. 1995; 25(Suppl):42-6S.
22. ISIS-4 Collaborative Group. Fourth international study of infarct survival: protocol for a large simple study of the effects of oral mononitrate, of oral captopril, and of intravenous magnesium. Am J Cardiol. 1991; 68:87-100D.
23. Simoons ML. Myocardial infarction: ACE inhibitors for all? for ever? Lancet. 1994; 344:279-81. Editorial.
24. Anon. An ACE inhibitor after a myocardial infarction. Med Lett Drugs Ther. 1994; 36:69-70. https://pubmed.ncbi.nlm.nih.gov/8035753
25. Ertl G, Jugdutt B. ACE inhibition after myocardial infarction: can megatrials provide answers? Lancet. 1994; 344:1068-9.
26. Ertl G. Angiotensin converting enzyme inhibitors in angina and myocardial infarction: what role will they play in the 1990s? Drugs. 1993; 46:209-18.
27. Purcell H, Coats A, Fox K et al. Improving outcome after acute myocardial infarction: what is the role of ACE inhibitors? Br J Clin Pract. 1995; 49:195-9. (IDIS 349780)
28. Ball SG, Hass AS. What to expect from ACE inhibitors after myocardial infarction. Br Heart J. 1994; 72(Suppl):S70-4.
29. ISIS-4 (Fourth International Study of Infarct Survival) Collaborative Group. ISIS-4: a randomised factorial trial assesssing early oral captopril, oral mononitrate, and intravenous magnesium sulphate in 58 050 patients with suspected acute myocardial infarction. Lancet. 1995; 345:669-85. https://pubmed.ncbi.nlm.nih.gov/7661937
30. Chinese Cardiac Study Collaborative Group. Oral captopril versus placebo among 13 634 patients with suspected acute myocardial infarction: interim report from the Chinese Cardiac Study (CCS-1). Lancet. 1995; 345:686-7. https://pubmed.ncbi.nlm.nih.gov/7885123
31. Cohn JN. The prevention of heart failure—a new agenda. N Engl J Med. 1992; 327:725-7. https://pubmed.ncbi.nlm.nih.gov/1495526
32. Pfeffer MA, Braunwald E, Moyé LA et al. Effect of captopril on mortality and morbidity in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med. 1992; 327:669-77. https://pubmed.ncbi.nlm.nih.gov/1386652
33. Swedberg K, Held P, Kjekshus J et al. Effects of the early administration of enalapril on mortality in patients with acute myocardial infarction: results of the Cooperative New Scandinavian enalapril survival study II (Consensus II). N Engl J Med. 1992; 327:678-84. https://pubmed.ncbi.nlm.nih.gov/1495520
34. Sharpe N, Smith H, Murphy J et al. Early prevention of left ventricular dysfunction after myocardial infarction with angiotensin-converting-enzyme inhibition. Lancet. 1991; 337:872-6. https://pubmed.ncbi.nlm.nih.gov/1672967
35. Oldroyd KG, Pye MP, Ray SG et al. Effects of early captopril administration on infarct expansion, left ventricular remodeling and exercise capacity after acute myocardial infarction. Am J Cardiol. 1991; 68:713-8. https://pubmed.ncbi.nlm.nih.gov/1892076
36. Sharpe N, Murphy J, Smith H et al. Treatment of patients with symptomless left ventricular dysfunction after myocardial infarction. Lancet. 1988; 1:255-9. https://pubmed.ncbi.nlm.nih.gov/2893080
37. Pfeffer MA, Lamas GA, Vaughan DE et al. Effect of captopril on progressive ventricular dilatation after anterior myocardial infarction. N Engl J Med. 1988; 319:80-6. https://pubmed.ncbi.nlm.nih.gov/2967917
38. National Heart, Lung, and Blood Institute National High Blood Pressure Education Program. The sixth report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC VI). Bethesda, MD: National Institutes of Health; 1997 Nov. (NIH publication No. 98-4080.)
39. Rey E, LeLorier J, Burgess E et al. Report of the Canadian Hypertension Society consensus conference: 3. pharmacologic treatment of hypertensive disorders in pregnancy. CMAJ. 1997; 157:1245-54. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1228354/ https://pubmed.ncbi.nlm.nih.gov/9361646
40. American College of Obstetricians and Gynecologists. ACOG technical bulletin No. 219: hypertension in pregnancy. 1996 Jan.
41. Hanssens M, Keirse MJ, Van Assche FA. Fetal and neonatal effects of treatment with angiotensin-converting enzyme inhibitors in pregnancy. Obstet Gynecol. 1991; 78:128-35. https://pubmed.ncbi.nlm.nih.gov/2047053
42. Brent RL, Beckman D. Angiotensin-converting enzyme inhibitors, an embryopathic class of drugs with unique properties: information for clinical teratology counselors. Teratology. 1991; 43:543-6. https://pubmed.ncbi.nlm.nih.gov/1882342
43. Piper JM, Ray WA, Rosa FW. Pregnancy outcome following exposure to angiotensin-converting enzyme inhibitors. Obstet Gynecol. 1992; 80:429-32. https://pubmed.ncbi.nlm.nih.gov/1495700
44. Sibai BM. Treatment of hypertension in pregnant women. N Engl J Med. 1996; 335:257-65. https://pubmed.ncbi.nlm.nih.gov/8657243
45. Barr M, Cohen MM. ACE inhibitor fetopathy and hypocalvaria: the kidney-skull connection. Teratology. 1991; 44:485-95. https://pubmed.ncbi.nlm.nih.gov/1771591
46. US Food and Drug Administration. Dangers of ACE inhibitors during pregnancy. FDA Med Bull. 1992; 22:2.
47. Yusuf S, Sleight P, Pogue J et al for the Heart Outcomes Prevention Evaluation Study Investigators. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on death from cardiovascular causes, myocardial infarction, and stroke in high-risk patients. N Engl J Med. (in press)
48. Kleinert S. HOPE cardiovascular disease prevention with ACE inhibitor ramipril. Lancet. 1999; 354:841. https://pubmed.ncbi.nlm.nih.gov/10485736
49. Hansson L, Lindholm LH, Niskanen L et al. Effects of angiotensin-converting enzyme inhibition compared with conventional therapy on cardiovascular morbidity and mortality in hypertension: the Captopril Prevention Project (CAPPP) randomised trial. Lancet. 1999; 353:611-616. https://pubmed.ncbi.nlm.nih.gov/10030325
50. Lonn EM, Yusuf S, Jha P et al. Emerging role of angiotensin-converting enzyme inhibitors in cardiac and vascular protection. Circulation. 1994; 90:2056-69. https://pubmed.ncbi.nlm.nih.gov/7923694
52. Genuth S. United Kingdom prospective diabetes study results are in. J Farm Pract. 1998; 47(Suppl 5):S27.
53. Watkins PJ. UKPDS: a message of hope and a need for change. Diabetic Med. 1998; 15:895-6. https://pubmed.ncbi.nlm.nih.gov/9827842
54. UK Prospective Diatetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ. 1998; 317:703-13. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC28659/ https://pubmed.ncbi.nlm.nih.gov/9732337
55. Bretzel RG, Voit K, Schatz H et al. The United Kingdom Prospective Diabetes Study (UKPDS): implications for the pharmacotherapy of type 2 diabetes mellitus. Exp Clin Endocrinol Diabetes. 1998; 106:369-72. https://pubmed.ncbi.nlm.nih.gov/9831300
57. Tatti P, Pahor M, Byington RP et al. Outcome results of the fosinopril versus amlodipine cardiovascular events randomized trial (FACET) in patients with hypertension and NIDDM. Diabetes Care. 1998; 21:597-603. https://pubmed.ncbi.nlm.nih.gov/9571349
58. American Diabetes Association. The United Kingdom Prospective Diabetes Study (UKPDS) for type 2 diabetes: what you need to know about the results of a long-term study. Washington, DC; 1998 Sep 15 from American Diabetes Association web site. http://www.dtu.ox.ac.uk/ukpds
59. UK Prospective Diabetes Study Group. Efficacy of atenolol and captopril in reducing risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 39. BMJ. 1998; 317:713-20. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC28660/ https://pubmed.ncbi.nlm.nih.gov/9732338
60. Davis TM. United Kingdom Prospective Diabetes Study: the end of the beginning? Med J Aust. 1998; 169:511-2.
63. Izzo JL, Levy D, Black HR. Importance of systolic blood pressure in older Americans. Hypertension. 2000; 35:1021-4. https://pubmed.ncbi.nlm.nih.gov/10818056
64. Frohlich ED. Recognition of systolic hypertension for hypertension. Hypertension. 2000; 35:1019-20. https://pubmed.ncbi.nlm.nih.gov/10818055
65. Bakris GL, Williams M, Dworkin L et al. Preserving renal function in adults with hypertension and diabetes: a consensus approach. Am J Kidney Dis. 2000; 36:646-61. https://pubmed.ncbi.nlm.nih.gov/10977801
66. Associated Press (American Diabetes Association). Diabetics urged: drop blood pressure. Chicago, IL; 2000 Aug 29. Press Release from web site. http://www.diabetes.org/newsroom/
67. Appel LJ. The verdict from ALLHAT—thiazide diuretics are the preferred initial therapy for hypertension. JAMA. 2002; 288:3039-60. https://pubmed.ncbi.nlm.nih.gov/12479770
68. The ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA. 2002; 288:2981-97. https://pubmed.ncbi.nlm.nih.gov/12479763
70. Merck & Co. Vasotec tablets (enalapril maleate) prescribing information. Whitehouse Station, NJ; 2002 Jan.
71. Bristol-Myers Squibb. Monopril (fosinopril sodium) tablets prescribing information. Princeton, NJ; 2002 Feb.
72. Merck. Prinivil (lisinopril) tablets prescribing information. Whitehouse Station, NJ; 2002 Jan.
73. AstraZeneca. Zestril (lisinopril) tablets prescribing information. Wilmington, DE: 2002 Jan.
74. Parke Davis. Accupril (quinapril hydrochloride) tablets prescribing information. Morris Plains, NJ; 2001 Mar.
77. Novartis. Diovan (valsartan) tablets prescribing information. East Hanover, NJ; 2002 Aug.
81. Lewis EJ, Hunsicker LG, Bain RP et al. The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy. N Engl J Med. 1993; 329:1456-62. https://pubmed.ncbi.nlm.nih.gov/8413456
82. Remuzzi G. Slowing the progression of diabetic nephropathy. N Engl J Med. 1993; 329:1496-7. https://pubmed.ncbi.nlm.nih.gov/8413463
83. Kaplan NM. Choice of initial therapy for hypertension. JAMA. 1996; 275:1577-80. https://pubmed.ncbi.nlm.nih.gov/8622249
84. Viberti G, Mogensen CE, Groop LC et al. Effect of captopril on progression to clinical proteinuria in patients with insulin-dependent diabetes mellitus and microalbuminuria. JAMA. 1994; 271:275-9. https://pubmed.ncbi.nlm.nih.gov/8295285
85. Fournier A. The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy. N Engl J Med. 1994; 330:937. https://pubmed.ncbi.nlm.nih.gov/8114873
86. Wright JT, Dunn JK, Cutler JA et al. Outcomes in hypertensive black and nonblack patients treated with chlorthalidone, amlodipine, and lisinopril. JAMA. 2005; 293:1595-607. https://pubmed.ncbi.nlm.nih.gov/15811979
87. Neaton JD, Kuller LH. Diuretics are color blind. JAMA. 2005; 293:1663-6. Editorial. https://pubmed.ncbi.nlm.nih.gov/15811986
88. Cooper WO, Hernandez-Diaz S, Arbogast PG et al. Major congenital malformations after first-trimester exposure to ACE inhibitors. N Engl J Med. 2006; 354:2443-51. https://pubmed.ncbi.nlm.nih.gov/16760444
89. Food and Drug Administration. FDA public health advisory: angiotensin-converting enzyme inhibitor (ACE inhibitor) drugs and pregnancy. From FDA website. http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/DrugSafetyInformationforHeathcareProfessionals/PublicHealthAdvisories/ucm053113.htm
90. Bristol-Myers Squibb Co. Capoten tablets (captopril tablets) prescribing information. In: Physicians’ desk reference. 49th ed. Montvale, NJ: Medical Economics Company Inc; 1995:710-4.
91. Bristol-Myers Squibb. Monopril (fosinopril sodium) tablets prescribing information. Princeton, NJ; 2002 Feb.
92. Parke Davis. Accupril (quinapril hydrochloride) tablets prescribing information. Morris Plains, NJ; 2001 Mar.
93. Merck. Prinivil (lisinopril) tablets prescribing information. Whitehouse Station, NJ; 2002 Jan.
94. Merck & Co. Vasotec tablets (enalapril maleate) prescribing information. Whitehouse Station, NJ; 2002 Jan.
95. Ciba Pharmaceutical Company. Lotensin (benazepril hydrochloride) tablets prescribing information. In: Physicians’ desk reference. 49th ed. Montvale, NJ: Medical Economics Company Inc; 1995:887-90.
96. Schwarz Pharma. Univasc™ (moexipril hydrochloride) tablets prescribing information. Milwaukee, WI; 2003 May.
97. Cobalt Pharmaceuticals, Bristol, TN: Personal communication.
501. James PA, Oparil S, Carter BL et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014; 311:507-20. https://pubmed.ncbi.nlm.nih.gov/24352797
502. Mancia G, Fagard R, Narkiewicz K et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013; 31:1281-357. https://pubmed.ncbi.nlm.nih.gov/23817082
503. Go AS, Bauman MA, Coleman King SM et al. An effective approach to high blood pressure control: a science advisory from the American Heart Association, the American College of Cardiology, and the Centers for Disease Control and Prevention. Hypertension. 2014; 63:878-85. https://pubmed.ncbi.nlm.nih.gov/24243703
504. Weber MA, Schiffrin EL, White WB et al. Clinical practice guidelines for the management of hypertension in the community: a statement by the American Society of Hypertension and the International Society of Hypertension. J Clin Hypertens (Greenwich). 2014; 16:14-26. https://pubmed.ncbi.nlm.nih.gov/24341872
505. Wright JT, Fine LJ, Lackland DT et al. Evidence supporting a systolic blood pressure goal of less than 150 mm Hg in patients aged 60 years or older: the minority view. Ann Intern Med. 2014; 160:499-503. https://pubmed.ncbi.nlm.nih.gov/24424788
506. Mitka M. Groups spar over new hypertension guidelines. JAMA. 2014; 311:663-4. https://pubmed.ncbi.nlm.nih.gov/24549531
507. Peterson ED, Gaziano JM, Greenland P. Recommendations for treating hypertension: what are the right goals and purposes?. JAMA. 2014; 311:474-6. https://pubmed.ncbi.nlm.nih.gov/24352710
508. Bauchner H, Fontanarosa PB, Golub RM. Updated guidelines for management of high blood pressure: recommendations, review, and responsibility. JAMA. 2014; 311:477-8. https://pubmed.ncbi.nlm.nih.gov/24352759
511. JATOS Study Group. Principal results of the Japanese trial to assess optimal systolic blood pressure in elderly hypertensive patients (JATOS). Hypertens Res. 2008; 31:2115-27. https://pubmed.ncbi.nlm.nih.gov/19139601
515. Thomas G, Shishehbor M, Brill D et al. New hypertension guidelines: one size fits most?. Cleve Clin J Med. 2014; 81:178-88. https://pubmed.ncbi.nlm.nih.gov/24591473
523. Fihn SD, Gardin JM, Abrams J et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation. 2012; 126:e354-471.
524. WRITING COMMITTEE MEMBERS, Yancy CW, Jessup M et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013; 128:e240-327.
525. Smith SC, Benjamin EJ, Bonow RO et al. AHA/ACCF Secondary Prevention and Risk Reduction Therapy for Patients with Coronary and other Atherosclerotic Vascular Disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation. Circulation. 2011; 124:2458-73. https://pubmed.ncbi.nlm.nih.gov/22052934
526. Kernan WN, Ovbiagele B, Black HR et al. Guidelines for the Prevention of Stroke in Patients With Stroke and Transient Ischemic Attack: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2014; :. https://pubmed.ncbi.nlm.nih.gov/24788967
527. O'Gara PT, Kushner FG, Ascheim DD et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013; 127:e362-425. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3695607/
530. Myers MG, Tobe SW. A Canadian perspective on the Eighth Joint National Committee (JNC 8) hypertension guidelines. J Clin Hypertens (Greenwich). 2014; 16:246-8. https://pubmed.ncbi.nlm.nih.gov/24641124
534. Qaseem A, Hopkins RH, Sweet DE et al. Screening, monitoring, and treatment of stage 1 to 3 chronic kidney disease: A clinical practice guideline from the American College of Physicians. Ann Intern Med. 2013; 159:835-47. https://pubmed.ncbi.nlm.nih.gov/24145991
535. Taler SJ, Agarwal R, Bakris GL et al. KDOQI US commentary on the 2012 KDIGO clinical practice guideline for management of blood pressure in CKD. Am J Kidney Dis. 2013; 62:201-13. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3929429/ https://pubmed.ncbi.nlm.nih.gov/23684145
536. Kidney Disease: Improving Global Outcomes (KDIGO) Blood Pressure Work Group. KDIGO clinical practice guideline for the management of blood pressure in chronic kidney disease. Kidney Int Suppl. 2012: 2: 337-414.
541. Perk J, De Backer G, Gohlke H et al. European Guidelines on cardiovascular disease prevention in clinical practice (version 2012). The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts). Eur Heart J. 2012; 33:1635-701. https://pubmed.ncbi.nlm.nih.gov/22555213
543. National Kidney Foundation Kidney Disease Outcomes Quality Initiative. K/DOQI Clinical practice guidelines on hypertension and antihypertensive agents in chronic kidney disease (2002). From National Kidney Foundation website. http://www.kidney.org/professionals/kdoqi/guidelines_commentaries.cfm
550. US Food and Drug Administration. FDA Drug Safety Communication: new warning and contraindication for blood pressure medicines containing aliskiren (Tekturna). Rockville, MD; 2012 April 4. From FDA website. http://www.fda.gov/Drugs/DrugSafety/ucm300889.htm
600. Pfizer. Altace (ramipril) capsules prescribing information. New York, NY; 2015 Sep.
701. Ponikowski P, Voors AA, Anker SD et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016; 37:2129-200. https://pubmed.ncbi.nlm.nih.gov/27206819
702. McMurray JJ, Packer M, Desai AS et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014; 371:993-1004. https://pubmed.ncbi.nlm.nih.gov/25176015
703. Ansara AJ, Kolanczyk DM, Koehler JM. Neprilysin inhibition with sacubitril/valsartan in the treatment of heart failure: mortality bang for your buck. J Clin Pharm Ther. 2016; 41:119-27. https://pubmed.ncbi.nlm.nih.gov/26992459
800. Yancy CW, Jessup M, Bozkurt B et al. 2016 ACC/AHA/HFSA Focused Update on New Pharmacological Therapy for Heart Failure: An Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation. 2016; 134:e282-93.
803. Lamas GA, Escolar E, Faxon DP. Examining treatment of ST-elevation myocardial infarction: the importance of early intervention. J Cardiovasc Pharmacol Ther. 2010; 15:6-16. https://pubmed.ncbi.nlm.nih.gov/20061507
805. Reed GW, Rossi JE, Cannon CP. Acute myocardial infarction. Lancet. 2017; 389:197-210. https://pubmed.ncbi.nlm.nih.gov/27502078
1100. Amsterdam EA, Wenger NK, Brindis RG et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014; 130:e344-426. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4676081/
1150. Flynn JT, Kaelber DC, Baker-Smith CM et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017; 140 https://pubmed.ncbi.nlm.nih.gov/28827377
1200. Whelton PK, Carey RM, Aronow WS et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018; 71:el13-e115. https://pubmed.ncbi.nlm.nih.gov/29133356
1201. Bakris G, Sorrentino M. Redefining hypertension - assessing the new blood-pressure guidelines. N Engl J Med. 2018; 378:497-499. https://pubmed.ncbi.nlm.nih.gov/29341841
1202. Carey RM, Whelton PK, 2017 ACC/AHA Hypertension Guideline Writing Committee. Prevention, detection, evaluation, and management of high blood pressure in adults: synopsis of the 2017 American College of Cardiology/American Heart Association hypertension guideline. Ann Intern Med. 2018; 168:351-358. https://pubmed.ncbi.nlm.nih.gov/29357392
1207. Burnier M, Oparil S, Narkiewicz K et al. New 2017 American Heart Association and American College of Cardiology guideline for hypertension in the adults: major paradigm shifts, but will they help to fight against the hypertension disease burden?. Blood Press. 2018; 27:62-65. https://pubmed.ncbi.nlm.nih.gov/29447001
1209. Qaseem A, Wilt TJ, Rich R et al. Pharmacologic treatment of hypertension in adults aged 60 years or older to higher versus lower blood pressure targets: a clinical practice guideline from the American College of Physicians and the American Academy of Family Physicians. Ann Intern Med. 2017; 166:430-437. https://pubmed.ncbi.nlm.nih.gov/28135725
1210. SPRINT Research Group, Wright JT, Williamson JD et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015; 373:2103-16. https://pubmed.ncbi.nlm.nih.gov/26551272
1213. Reboussin DM, Allen NB, Griswold ME et al. Systematic review for the 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018; 71:2176-2198. https://pubmed.ncbi.nlm.nih.gov/29146534
1214. American Diabetes Association. 9. Cardiovascular disease and risk management: standards of medical care in diabetes 2018. Diabetes Care. 2018; 41:S86-S104. https://pubmed.ncbi.nlm.nih.gov/29222380
1215. de Boer IH, Bangalore S, Benetos A et al. Diabetes and hypertension: a position statement by the American Diabetes Association. Diabetes Care. 2017; 40:1273-1284. https://pubmed.ncbi.nlm.nih.gov/28830958
1216. Taler SJ. Initial treatment of hypertension. N Engl J Med. 2018; 378:636-644. https://pubmed.ncbi.nlm.nih.gov/29443671
1218. Messerli FH, Bangalore S, Bavishi C et al. Angiotensin-converting enzyme inhibitors in hypertension: to use or not to use?. J Am Coll Cardiol. 2018; 71:1474-1482. https://pubmed.ncbi.nlm.nih.gov/29598869
1220. Cifu AS, Davis AM. Prevention, detection, evaluation, and management of high blood pressure in adults. JAMA. 2017; 318:2132-2134. https://pubmed.ncbi.nlm.nih.gov/29159416
1222. Bell KJL, Doust J, Glasziou P. Incremental benefits and harms of the 2017 American College of Cardiology/American Heart Association high blood pressure guideline. JAMA Intern Med. 2018; 178:755-7. https://pubmed.ncbi.nlm.nih.gov/29710197
1223. LeFevre M. ACC/AHA hypertension guideline: what is new? what do we do?. Am Fam Physician. 2018; 97(6):372-3. https://pubmed.ncbi.nlm.nih.gov/29671534
1224. Brett AS. New hypertension guideline is released. From NEJM Journal Watch website. Accessed 2018 Jun 18. https://www.jwatch.org/na45778/2017/12/28/nejm-journal-watch-general-medicine-year-review-2017
1229. Ioannidis JPA. Diagnosis and treatment of hypertension in the 2017 ACC/AHA guidelines and in the real world. JAMA. 2018; 319(2):115-6. https://pubmed.ncbi.nlm.nih.gov/29242891
1232. American Diabetes Association. 10. Microvascular complications and foot care: standards of medical care in diabetes 2018. Diabetes Care. 2018; 41:S86-S104. https://pubmed.ncbi.nlm.nih.gov/29222381
a. Pfizer. Altace (ramipril) capsules for oral use prescribing information. New York, NY; 2015 Sep.
Related/similar drugs
Frequently asked questions
More about ramipril
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (136)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: Angiotensin Converting Enzyme Inhibitors
- Breastfeeding
- En español