Decitabine and Cedazuridine (Monograph)
Drug class: Antineoplastic Agents
Chemical name: 4-amino-1-[(2R,4S,5R)-4-hydroxy-5-(hydroxymethyl)oxolan-2-yl]-1,3,5-triazin-2(1H)-one
Molecular formula: C8H12N4O4C9H14F2N2O5
CAS number: 22432-95-7
Introduction
Antineoplastic agent; fixed combination containing decitabine (nucleoside metabolic inhibitor) and cedazuridine (cytidine deaminase inhibitor).1 3 4 7
Uses for Decitabine and Cedazuridine
Myelodysplastic Syndrome
Treatment of myelodysplastic syndrome (MDS);1 3 4 6 designated an orphan drug by FDA for this use.2
Used in patients with previously treated or untreated, de novo or secondary MDS with the following French-American-British (FAB) subtypes: refractory anemia, refractory anemia with ringed sideroblasts, refractory anemia with excess blasts, and chronic myelomonocytic leukemia (CMML) and intermediate-1, intermediate-2, and high-risk International Prognostic Scoring System (IPSS) groups.1
Some clinicians offer decitabine/cedazuridine in place of parenteral hypomethylating agents because of convenience of oral administration.8
Decitabine and Cedazuridine Dosage and Administration
General
Pretreatment Screening
-
Obtain complete blood cell (CBC) counts prior to initiation of therapy.1 Patients should have an absolute neutrophil count (ANC) of at least 1000/mm3 and a platelet count of at least 50,000/mm3 (in the absence of active disease).1
-
Verify pregnancy status in females of reproductive potential prior to initiating decitabine/cedazuridine therapy.1
Patient Monitoring
-
Obtain CBC counts prior to initiation of each cycle.1 Patients should have an absolute neutrophil count (ANC) of at least 1000/mm3 and a platelet count of at least 50,000/mm3 (in the absence of active disease) prior to each cycle.1
-
Monitor for hematologic and nonhematologic toxicities.1
-
Closely monitor patients with moderate renal impairment (creatinine clearance 30–59 mL/minute) for adverse reactions.1
Premedication and Prophylaxis
-
Consider premedication with antiemetics prior to each dose.1
-
Females of reproductive potential should be advised to use effective contraception during and for 6 months after discontinuance of decitabine/cedazuridine therapy.1 Male patients receiving decitabine/cedazuridine who have female partners of reproductive potential should be advised to use effective contraception during and for 3 months after discontinuance of therapy.1
Dispensing and Administration Precautions
-
Procedures for proper handling and disposal of antineoplastic agents should be followed.1
-
The fixed combination of decitabine and cedazuridine should not be substituted for IV decitabine within a cycle of therapy.1
Administration
Oral Administration
Administer orally at the same time each day on an empty stomach; do not consume food within 2 hours before or 2 hours after administration.1 Swallow tablets whole; do not cut, crush, or chew.1
If a dose is missed and is remembered within 12 hours of scheduled time, take missed dose as soon as possible, then resume normal daily dosing schedule.1 Extend dosing period 1 day for every missed dose to complete 5 daily doses for each cycle.1
If vomiting occurs after administration, do not take an extra dose; take next dose at regularly scheduled time.1
Dosage
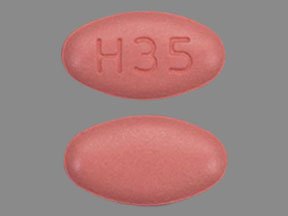
Commercially available as a fixed-combination tablet containing 35 mg of decitabine and 100 mg of cedazuridine.1
Adults
Myelodysplastic Syndrome
Oral
1 tablet (35 mg decitabine and 100 mg cedazuridine) once daily on days 1 through 5 of each 28-day cycle.1
A minimum of 4 treatment cycles is recommended; however, additional cycles may be needed to achieve a complete or partial response.1
Continue therapy until disease progression or unacceptable toxicity occurs.1
Dosage Modification for Toxicity
Hematologic Toxicity
If hematologic recovery (i.e., ANC ≥1000/mm3, platelet count ≥50,000/mm3 in absence of active disease) from previous treatment cycle has not occurred, delay next treatment cycle until hematologic recovery occurs.1
If hematologic recovery occurs within 2 weeks of achieving remission, continue decitabine/cedazuridine at same dosage.1
If hematologic recovery does not occur within 2 weeks of achieving remission, delay next treatment cycle for up to 2 more weeks, then administer next cycle at reduced dosage of 1 tablet (35 mg decitabine and 100 mg cedazuridine) once daily on days 1 through 4 of each 28-day cycle.1
If myelosuppression persists after dosage reduction, consider further decrease in dosage.1 If a second dosage reduction is required, recommended dosage is 1 tablet (35 mg decitabine and 100 mg cedazuridine) once daily on days 1 through 3 of each 28-day cycle.1 If a third dosage reduction is required, recommended dosage is 1 tablet (35 mg decitabine and 100 mg cedazuridine) once daily on days 1, 3, and 5 of each 28-day cycle.1
In each treatment cycle, maintain dosage at a reduced level or increase dosage as clinically indicated.1
Manage persistent severe neutropenia and febrile neutropenia with supportive treatment.1
Nonhematologic Toxicity
If serum creatinine concentration increases to ≥2 mg/dL; serum ALT, AST, or total bilirubin concentration increases to ≥2 times the upper limit of normal; or active or uncontrolled infection occurs, do not restart decitabine/cedazuridine therapy until toxicity has resolved.1 When toxicity has resolved, resume decitabine/cedazuridine therapy at same or reduced dosage as clinically appropriate.1
Special Populations
Hepatic Impairment
Specific dosage recommendations not available.1
Renal Impairment
No dosage modification recommended for patients with mild or moderate renal impairment (ClCr 30–89 mL/minute).1
Geriatric Patients
Specific dosage recommendations not available.1
Cautions for Decitabine and Cedazuridine
Contraindications
-
Manufacturer states none known.1
Warnings/Precautions
Fetal/Neonatal Morbidity and Mortality
May cause fetal harm; teratogenicity and embryolethality demonstrated in animals.1 Verify pregnancy status in women of reproductive potential prior to initiating therapy.1 Women should avoid pregnancy during therapy and for 6 months after therapy.1 Men with female partners of reproductive age should use effective contraception during therapy and for 3 months after therapy.1 If used during pregnancy or if patient becomes pregnant during therapy, apprise of potential fetal hazard.1
Myelosuppression
Risk of dose-limiting and potentially fatal myelosuppression, manifested commonly as severe neutropenia, severe thrombocytopenia, anemia, and serious and fatal infectious complications.1 Myelosuppression may occur more frequently in the first and second treatment cycles and may not indicate progression of underlying MDS.1
Delay or reduce dosage for subsequent cycles based on hematologic recovery.1
Perform CBC at baseline, prior to each cycle, and as clinically indicated.1 Consider use of hematopoietic growth factor and/or anti-infective therapy to prevent or treat complicating infections.1 3
Specific Populations
Pregnancy
No adequate data in humans; based on limited human data, animal studies, and mechanism of action, may cause fetal harm when administered to a pregnant woman.1
Lactation
Not known whether distributed into milk; effects on milk production or breast-fed infant also not known.1 Because of potential for serious adverse reactions in the breast-fed infant, women should not breast-feed during therapy and for ≥2 weeks after the last dose.1
Females and Males of Reproductive Potential
Advise females of reproductive potential to use effective contraception during treatment and for 6 months after last dose.1
Advise male patients with female partners of reproductive potential to use effective contraception during treatment and for 3 months after last dose.1
Based on nonclinical data, may impair male fertility; reversibility of effects unknown.1
Pediatric Use
Safety and efficacy not established.1
Geriatric Use
No overall differences in safety or efficacy observed between geriatric and younger patients.1
Hepatic Impairment
Not studied in patients with moderate or severe hepatic impairment.1
Renal Impairment
Due to potential for increased adverse reactions, frequently monitor patients with moderate renal impairment (ClCr 30–59 mL/minute) for adverse reactions.1
Not studied in patients with severe renal impairment (ClCr 15–29 mL/minute) or end-stage renal disease (ClCr <15 mL/minute).1
Common Adverse Effects
Adverse effects reported in ≥20% of patients: Fatigue,1 6 constipation,1 6 hemorrhage,1 myalgia,1 mucositis,1 arthralgia,1 nausea,1 6 dyspnea,1 6 diarrhea,1 6 rash,1 dizziness,1 6 febrile neutropenia,1 6 edema,1 headache,1 cough,1 decreased appetite,1 upper respiratory tract infection,1 pneumonia,1 increased transaminase concentrations,1 leukopenia,1 6 thrombocytopenia,1 6 neutropenia,1 6 anemia.1 6
Drug Interactions
Decitabine is not a substrate for CYP enzymes and is unlikely to inhibit or induce CYP enzymes.1
No clinically meaningful effect of decitabine on pharmacokinetics of cedazuridine.1 Cedazuridine, an inhibitor of cytidine deaminase, increases systemic exposure of decitabine.1
Cedazuridine is not a substrate of CYP enzymes.1 Cedazuridine does not induce CYP1A, CYP2B6, CYP2C9, or CYP3A, and does not inhibit CYP1A, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6, CYP2E1, or CYP3A.1
Cedazuridine is not a substrate of P-glycoprotein (P-gp), multidrug and toxin extrusion transporters (MATE) 1 or MATE2K, organic anion transporters (OAT) 1 or OAT3, organic anion transport proteins (OATP) 1B1, OATP1B3, or OATP2B1, or organic cation transporters (OCT) 1 or OCT2, and does not inhibit P-gp, breast cancer resistance protein (BCRP), MATE1, MATE2K, OAT1, OAT3, OATP1B1, OATP1B3, or OCT2.1
Drugs Metabolized by Cytidine Deaminase
Coadministration of decitabine and cedazuridine with drugs that are metabolized by cytidine deaminase may increase systemic exposure and toxicity of the substrate drug.1 Avoid coadministration of decitabine/cedazuridine with drugs that are metabolized by cytidine deaminase.1 3
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Gemcitabine |
Possible increased exposure and toxicity of gemcitabine (cytidine deaminase substrate)1 3 |
Avoid concomitant administration with decitabine/cedazuridine1 3 |
|
Proton-pump inhibitors |
No clinically important effect on decitabine/cedazuridine exposure1 |
Decitabine and Cedazuridine Pharmacokinetics
Absorption
Bioavailability
Decitabine peak concentrations and AUC increase in an approximately dose-proportional manner over the dosing interval following oral administration of decitabine 20–40 mg once daily (0.6–1.1 times the recommended dose) in combination with 100 mg oral cedazuridine.1
Cedazuridine peak concentrations and AUC increase in an approximately dose-proportional manner over the dosing interval following oral administration of cedazuridine 40–100 mg once daily (0.4–1 times the recommended dose) in combination with 20 mg of oral decitabine.1
The geometric mean ratio (GMR) of decitabine AUC following the first dose of oral decitabine/cedazuridine compared to that of IV decitabine on day 1 was 60% in patients with MDS or CMML.1
GMR of decitabine AUC following 5 consecutive once-daily doses of decitabine/cedazuridine compared to that of IV decitabine on day 5 was 106% and GMR of the 5-day cumulative decitabine AUC following 5 consecutive once-daily doses of decitabine/cedazuridine compared to that of IV decitabine was 99%.1 5
Following oral administration of decitabine/cedazuridine at the recommended dose in patients with MDS or CMML, mean oral bioavailability of cedazuridine is approximately 20%.1
Median time to peak plasma concentrations is approximately 1 or 3 hours for decitabine or cedazuridine, respectively.1
Food
Administration of decitabine/cedazuridine with food (high-fat, high-calorie meal) has little effect on cedazuridine exposure; however, decitabine exposure parameters are approximately 40% (AUC) to 53.5% (peak concentration) lower compared to those following administration under fasted conditions.3
Distribution
Plasma Protein Binding
In vitro, decitabine is 94–96% unbound to plasma proteins at a concentration of 17–342 ng/mL, and cedazuridine is 62–66% unbound to plasma proteins at a concentration of 1000–50,000 ng/mL.1
Elimination
Metabolism
Decitabine is metabolized primarily by cytidine deaminase and by physicochemical degradation.1 Cedazuridine is metabolized primarily via conversion to epimer by physicochemical degradation.1
Elimination Route
Cedazuridine eliminated in urine (46%; 21% as unchanged drug) and in feces (51%; 27% as unchanged drug).1
Half-life
Mean terminal elimination half-life at steady state is 1.5 or 6.7 hours for decitabine or cedazuridine, respectively.1
Special Populations
Age (32–90 years), sex, and mild hepatic impairment do not substantially affect the pharmacokinetics of decitabine or cedazuridine when administered as the fixed combination.1
Decitabine exposure (AUC) increases with decreasing body surface area or body weight, and cedazuridine exposure increases with decreasing ClCr; however, body surface area (1.3–2.9 m2), body weight (41–158 kg), and mild to moderate renal impairment (ClCr 30–89 mL/minute) do not have a clinically important effect on pharmacokinetics of decitabine and cedazuridine after administration of fixed combination.1
Stability
Storage
Oral
Tablets
20–25°C (excursions permitted between 15–30°C).1
Dispense in original packaging; follow procedures for proper handling and disposal of antineoplastic agents.1
Actions
-
Decitabine exerts its antineoplastic effect by incorporating into DNA and inhibiting DNA methyltransferase, thereby causing hypomethylation of DNA and cellular differentiation and/or apoptosis.1 4 7 Does not appear to cause major suppression of DNA synthesis.1 7
-
Decitabine-induced hypomethylation in cancer cells may restore normal function to genes that are critical for cellular differentiation and proliferation.1
-
Decitabine may exert a direct cytotoxic effect by forming covalent adducts with DNA methyltransferase in rapidly dividing cells.1 Nonproliferating cells are relatively insensitive to decitabine.1
-
Cedazuridine increases systemic exposure of decitabine by inhibiting cytidine deaminase, an enzyme present in high levels in the GI tract and liver that catalyzes the degradation of cytidine, including the cytidine analog decitabine.1 4
Advice to Patients
-
Importance of advising patients to read the FDA-approved patient labeling (patient information).1
-
Importance of advising patients to take decitabine/cedazuridine at approximately the same time each day on an empty stomach.1 Instruct patients to avoid eating for at least 2 hours before and 2 hours after taking the fixed-combination tablets.1
-
Advise patients to take a missed dose as soon as possible if it is remembered within 12 hours of the scheduled dose and to then resume the regular dosing schedule.1 Importance of advising patients to extend the dosing period by 1 day for every missed dose to complete 5 daily doses for each cycle.1
-
Advise patients not to take an extra dose in case of vomiting after taking the drug; the next dose should be taken at the regularly scheduled time.1
-
Importance of advising patients of the risk of myelosuppression and to report any symptoms of fever, infection, anemia, or bleeding to their clinician as soon as possible.1 Advise patients of the need for laboratory monitoring.1
-
Importance of women informing clinicians immediately if they are or plan to become pregnant or plan to breast-feed.1 Advise women to avoid pregnancy during and for 6 months following discontinuance of therapy.1 Advise men with female partners of reproductive age to use effective contraception during therapy and for 3 months following discontinuance of therapy.1 Necessity of advising pregnant women of the risk to the fetus.1
-
Importance of advising women not to breast-feed during treatment with decitabine/cedazuridine and for 2 weeks after the last dose.1
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses.1
-
Importance of informing patients of other important precautionary information.1 (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
35 mg decitabine, 100 mg cedazuridine |
Inqovi |
Taiho Oncology |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions July 22, 2022. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
References
1. Taiho Pharmaceutical Co., Ltd.. Inqovi (decitabine and cedazuridine) oral prescribing information. Princeton, NJ; 2020 Jul. http://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=91a0f80b-f865-4d06-a40d-4d148d99ee71
2. Food and Drug Administration. Orphan designation pursuant to Section 526 of the Federal Food and Cosmetic Act as amended by the Orphan Drug Act. (P.L. 97-414). Rockville, MD; From FDA website. http://www.fda.gov/ForIndustry/DevelopingProductsforRareDiseasesConditions/HowtoapplyforOrphanProductDesignation/default.htm
3. Food and Drug Administration. Center for Drug Evaluation and Research: Application number 212576Orig1s000: Multi-discipline Review. From FDA website. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2020/212576Orig1s000MultidisciplineR.pdf
4. Dhillon S. Decitabine/Cedazuridine: First Approval. Drugs. 2020; 80:1373-1378. https://pubmed.ncbi.nlm.nih.gov/32860582
5. Garcia-Manero G, McCloskey J, Griffiths EA et al. Pharmacokinetic Exposure Equivalence and Preliminary Efficacy and Safety from a Randomized Cross over Phase 3 Study (ASCERTAIN study) of an Oral Hypomethylating Agent ASTX727 (cedazuridine/decitabine) Compared to IV Decitabine. Blood. 2019; 134 (Suppl 1): 846. https://ashpublications.org/blood/article/134/Supplement_1/846/426917/Pharmacokinetic-Exposure-Equivalence-and
6. Garcia-Manero G, Griffiths EA, Steensma DP et al. Oral cedazuridine/decitabine for MDS and CMML: a phase 2 pharmacokinetic/pharmacodynamic randomized crossover study. Blood. 2020; 136:674-683. https://pubmed.ncbi.nlm.nih.gov/32285126
7. Patel AA, Cahill K, Saygin C et al. Cedazuridine/decitabine: from preclinical to clinical development in myeloid malignancies. Blood Adv. 2021; 5:2264-2271. https://pubmed.ncbi.nlm.nih.gov/33904891
8. Tremblay D, Rippel N, Feld J et al. Contemporary Risk Stratification and Treatment of Chronic Myelomonocytic Leukemia. Oncologist. 2021; 26:406-421. https://pubmed.ncbi.nlm.nih.gov/33792103
9. Cheson BD, Greenberg PL, Bennett JM et al. Clinical application and proposal for modification of the International Working Group (IWG) response criteria in myelodysplasia. Blood. 2006; 108:419-25. https://pubmed.ncbi.nlm.nih.gov/16609072
Related/similar drugs
More about cedazuridine / decitabine
- Check interactions
- Compare alternatives
- Reviews (5)
- Side effects
- Dosage information
- During pregnancy
- Drug class: antineoplastic combinations
- En español