Hypertrophic Cardiomyopathy
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What is hypertrophic cardiomyopathy (HCM)?
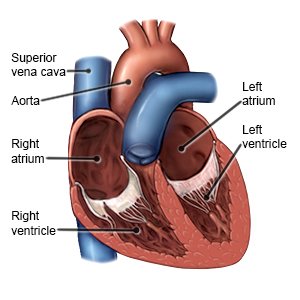
HCM is a disease that causes heart muscle cells to become large. As the cells get larger, they cause the walls of your ventricles to become thick and stiff. The ventricles are the 2 lower chambers of your heart. They pump blood to your lungs and the rest of your body. When the ventricles are thick or stiff, your heart cannot fill with enough blood. This decreases the blood and oxygen supply to the rest of your body. HCM is usually inherited, but it may develop over time. High blood pressure, thyroid disease, or diabetes increase your risk for HCM.
 |
What are the signs and symptoms of HCM?
You may have no signs or symptoms, or you may have any of the following:
- Chest pain
- Shortness of breath especially during exercise
- Feeling dizzy or faint
How is HCM diagnosed?
Your healthcare provider will listen to your heart and lungs. Your provider may check your abdomen, ankles, and feet for swelling. Tell your provider if you have other health conditions or family members with heart disease. You may need the following tests:
- An EKG or ECG records the electrical activity of your heart. It may show abnormal heartbeats or signals from changes to the heart muscle.
- A chest x-ray will show enlarged ventricles or a large left atrium.
- An echocardiogram is a type of ultrasound. Sound waves are used to show the structure and function of your heart.
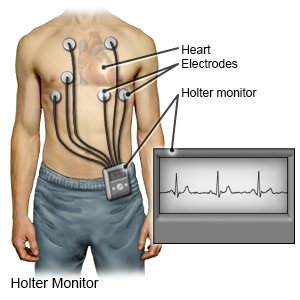
- A Holter monitor will record your heart's activity for a length of time prescribed by your doctor. The results may show changes in your heart's rhythm.
- A cardiac MRI may show the size of your heart and the thickness of your ventricles. It can also show if you have iron buildup in your heart. You may be given contrast liquid to help the pictures show up better. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid. Do not enter the MRI room with anything metal. The MRI machine uses a powerful magnet. Metal can cause serious injury from the magnet. Tell the healthcare provider if you have any metal in or on your body.
- Cardiac catheterization is a procedure used to look for or treat a heart condition. A catheter is inserted in your arm, neck, or groin and moved into your heart. Contrast liquid is injected into an artery and x-rays of your blood flow are taken. Tell a healthcare provider if you have ever had an allergic reaction to contrast liquid.
- A stress test will show your heart's response to exercise.
- A genetic test will show if HCM was passed to you from your parents. The test can also show the risk to any children you have or plan to have. Your provider can give you more information about genetic testing.
How is HCM treated?
Treatment depends on how much HCM has affected your health. The goal of treatment is to stop the problems caused by HCM and keep the disease from getting worse. You may need any of the following:
- Blood thinners help prevent blood clots. These include aspirin and warfarin. Take your medicine exactly as directed. Tell your healthcare provider if you forgot to take it or if you took too much. Blood thinners may cause you to bleed or bruise more easily. Use a soft toothbrush and an electric shaver. Wear medical alert jewelry or carry a card that says you take a blood thinner. Tell all healthcare providers, including your dentist, that you take this medicine.
- Heart medicine helps strengthen or regulate your heartbeat.
- Antihypertensive medicine helps lower your blood pressure. A controlled blood pressure helps protect your organs, such as your heart, lungs, brain, and kidneys. Take the medicine exactly as directed.
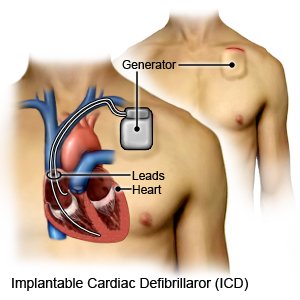
- An implantable cardioverter defibrillator (ICD) is a small device that monitors your heart rate and rhythm. It is placed inside your chest or abdomen. An ICD can give a shock to your heart to make it start beating again. It can also make your heart beat faster or slower.
- Open heart surgery may be needed to remove part of the thickened muscle that separates the left from right ventricle. You may also need to have a heart valve repaired or replaced so your heart can pump enough blood to your body. Heart valves allow blood flow between the chambers of your heart.
- Septal ablation is a procedure to shrink part of the muscle and increase the amount of blood the heart can pump. A cardiac catheter is used to inject a solution of alcohol into the thickened part of the heart wall (septum).
Treatment options
The following list of medications are related to or used in the treatment of this condition.
Related medications
How can I manage HCM?
- Manage any other health conditions. Diabetes and high blood pressure that are not controlled will increase your risk for heart problems.
- Limit liquids. Talk to your healthcare provider about how much liquid to drink in a day. Your risk for fluid buildup and swelling increases if you drink too much. Your risk for dehydration increases if you do not drink enough liquid. Your heart has to work harder with too much or too little liquid.
- Eat heart-healthy foods. Heart-healthy foods help lower your risk for heart disease. Your provider may recommend the DASH eating plan. The DASH plan is low in sodium, processed sugar, unhealthy fats, and total fat. It is high in potassium, calcium, and fiber. These can be found in vegetables, fruit, and whole-grain foods. Eat a variety of fresh, frozen, or canned vegetables and fruits. Eat vegetables and fruits without creamy sauces or added salt and sugars. You can get more fiber by eating brown rice instead of white rice. Oatmeal and beans are also good sources of fiber. Eat healthy fats, such as peanut butter, nuts, tuna, and avocados.

- Avoid alcohol. Alcohol can increase your symptoms by increasing your risk for dehydration or weight gain.
- Talk to your provider about physical activity. Your provider will help you make a plan. The plan may include certain exercises or activities to avoid. Tell your provider about any sports or vigorous activities you do. Your provider may help you decide if the benefits of continuing outweigh the possible risks.
- Do not smoke. Smoking weakens your heart and makes shortness of breath and other symptoms worse. If you smoke, it is never too late to quit. Ask your provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your provider before you use these products.
Call your local emergency number (911 in the US) or have someone call if:
- You have chest pain that may be worse when you take a deep breath or cough. You may cough up blood.
- You have a sudden cold sweat, especially with chest discomfort or trouble breathing.
- You feel very lightheaded or dizzy, especially with chest discomfort or trouble breathing.
- You have pain or discomfort in your back, neck, jaw, abdomen, or one or both of your arms.
- You have a severe headache or vision loss.
- You have weakness in an arm or leg.
- You are confused or have trouble speaking.
- You suddenly have trouble breathing.
When should I seek immediate care?
- You gain weight for no known reason.
- You feel weak or more tired than usual.
- You have increased swelling in your legs, ankles, feet, or abdomen.
- Your symptoms return or get worse.
- You feel like your heart is beating faster than normal, fluttering, or jumping in your chest.
When should I call my doctor?
- You urinate less than usual or not at all.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Hypertrophic Cardiomyopathy
Treatment options
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
