End-stage renal disease
Medically reviewed by Drugs.com. Last updated on Jun 9, 2025.
What is end-stage renal disease?
End-stage renal disease is a condition in which the kidneys no longer function normally. Renal describes anything having to do with the kidneys. Nearly everyone is born with two kidneys. They both need to fail for end-stage renal disease to develop.
Kidneys eliminate poisons from the body and keep a normal balance of fluid and certain minerals in the body. When the kidneys can no longer perform this function, a person becomes seriously ill and ultimately dies.
In end-stage renal disease, the kidneys function at a fraction of their normal capacity. When this occurs, there are only two options:
- replace kidney function with dialysis
- kidney transplant. A single transplanted kidney can do the work of the two sick ones.
Diabetes is the leading cause of end-stage renal disease. Kidney disease can result from type 1 or type 2 diabetes. With either type, poor control of blood sugar increases the risk of end-stage renal disease.
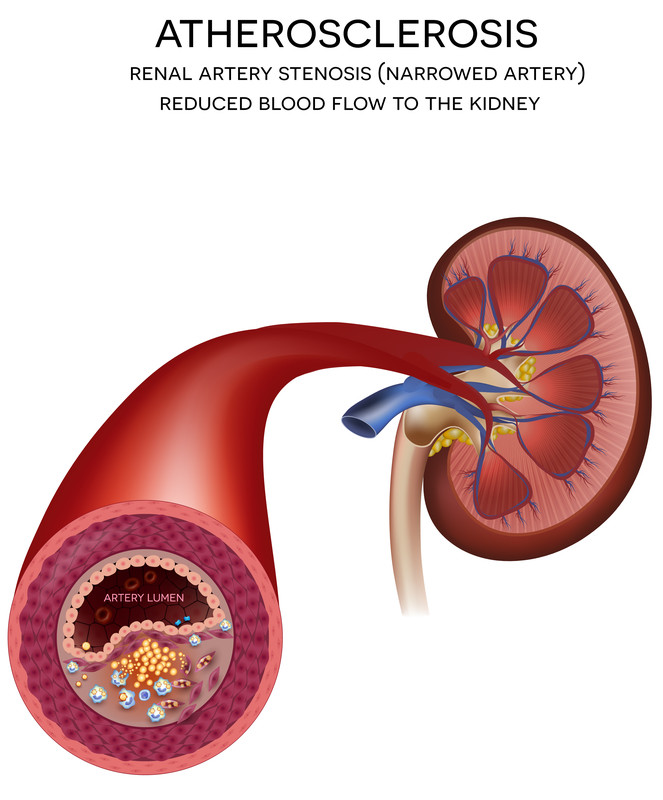
Other common causes of end-stage renal disease are:
|
|
- autoimmune diseases like systemic lupus erythematosus (lupus)
- genetic disorders, such as polycystic kidney disease
- exposure to toxic drugs, including:
- certain antibiotics
- chemotherapy
- contrast dyes
- pain relievers.
Symptoms of end-stage renal disease
Symptoms of end-stage renal disease include:
- weight loss
- nausea, vomiting, loss of appetite
- malaise
- fatigue
- headache
- hiccups
- itching
- decreased urination
- easy bruising or bleeding
- lethargy
- difficulty breathing
- seizures.
Symptoms may remain mild or absent until kidney function drops to less than 20% of normal.
Dialysis is urgent when one or more of the following occurs:
- fluid overload or congestive heart failure (CHF) that cannot be managed with medications. In CHF, fluid backs up into the lungs, legs and other parts of the body.
- dangerous elevations of potassium, sodium or acids in the blood. These substances can affect how other organs function.
- confusion, decreased alertness, or seizures
- bleeding related to kidney failure that cannot be improved through other means
- severe, unrelenting nausea and vomiting
- inflammation of the covering of the heart.
Dialysis may also be necessary if symptoms affect quality of life or nutritional status. This is especially true if they are accompanied by severely abnormal blood tests.
Diagnosing end-stage renal disease
Kidney disease is diagnosed through urine and blood tests. These tests measure levels of creatinine and urea nitrogen in the urine and blood.
Additional tests may be necessary to determine why the kidneys have stopped working. For example, a kidney biopsy may be recommended, in which a tiny sample of kidney tissue is removed and carefully examined under a microscope.
Expected duration of end-stage renal disease
End-stage renal disease is almost always a lifelong condition unless a kidney transplant is done. Even with a successful transplant, a person must take medicine for the rest of his or her life.
Preventing end-stage renal disease
You can take steps to reduce your risk of developing end-stage renal disease:
- If you have diabetes, control your blood sugar.
- Closely monitor and aggressively treat high blood pressure. High blood pressure further damages the kidneys in people with kidney disease.
- If you have kidney disease, avoid over-the-counter arthritis medicines. Nonsteroidal anti-inflammatory drugs (NSAIDs) can cause kidney damage.
- Talk with your doctor about medication that may slow the progression of chronic kidney disease. Your doctor may recommend an SGLT2 inhibitor such as canagliflozin (Invokana), dapagliflozin (Farxiga), or empagliflozin (Jardiance).
- Quitting smoking and lowering cholesterol levels may also help.
Treating end-stage renal disease
The two treatments for end-stage renal disease are dialysis and kidney transplant.
Dialysis
There are two types of dialysis:
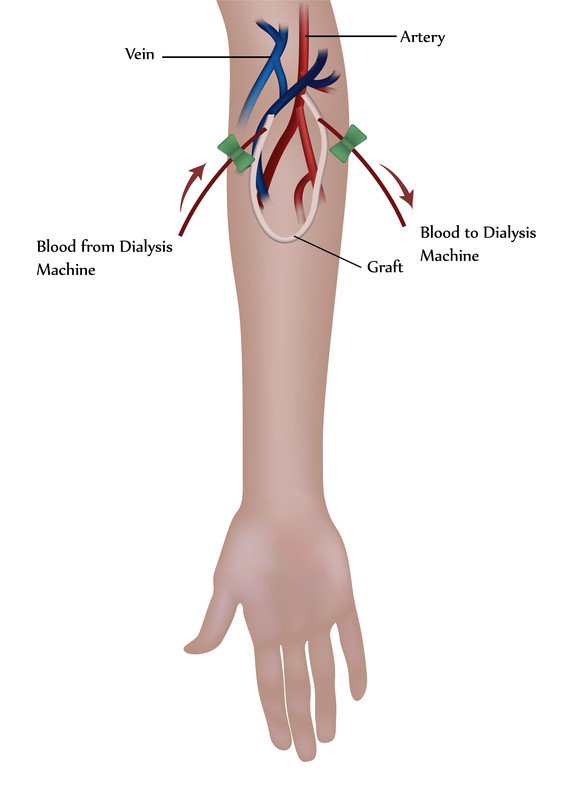
- Hemodialysis: During hemodialysis, blood is removed from a fistula or graft in your arm, run through filters in a hemodialysis machine to remove waste products, and then returned from the machine to your body. A fistula is a connection between a vein and artery created by a surgeon weeks to months before starting hemodialysis. A graft is a soft tube connecting an artery and vein surgically implanted in anticipation of hemodialysis.
- Hemodialysis usually is done at a dialysis center. The treatments are typically performed three times a week, in three-to-four-hour sessions.
|
|
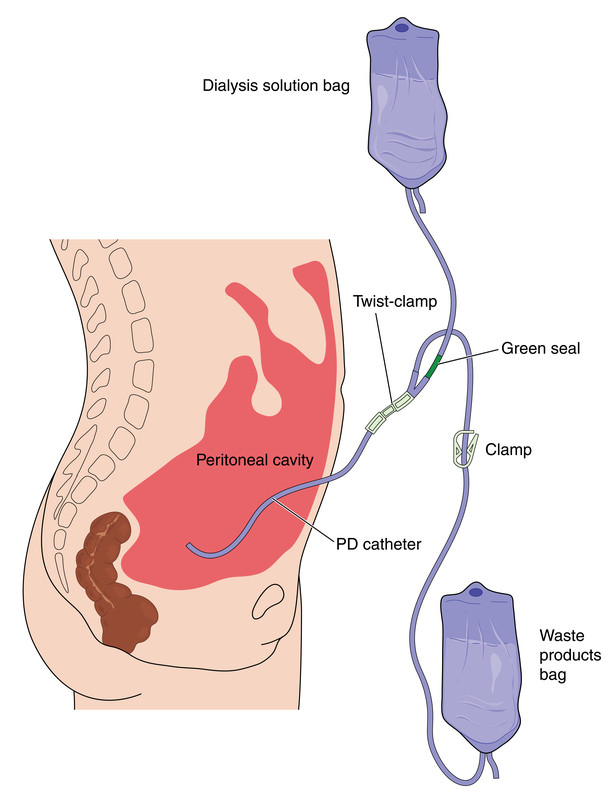
- Peritoneal dialysis: During peritoneal dialysis, sterile fluid is infused into the abdomen. Waste products gradually accumulate in the fluid, which is drained several hours later. Peritoneal dialysis is done at home. It takes longer than hemodialysis and must be done three to five times a day. It can be automated to occur during sleep.
|
|
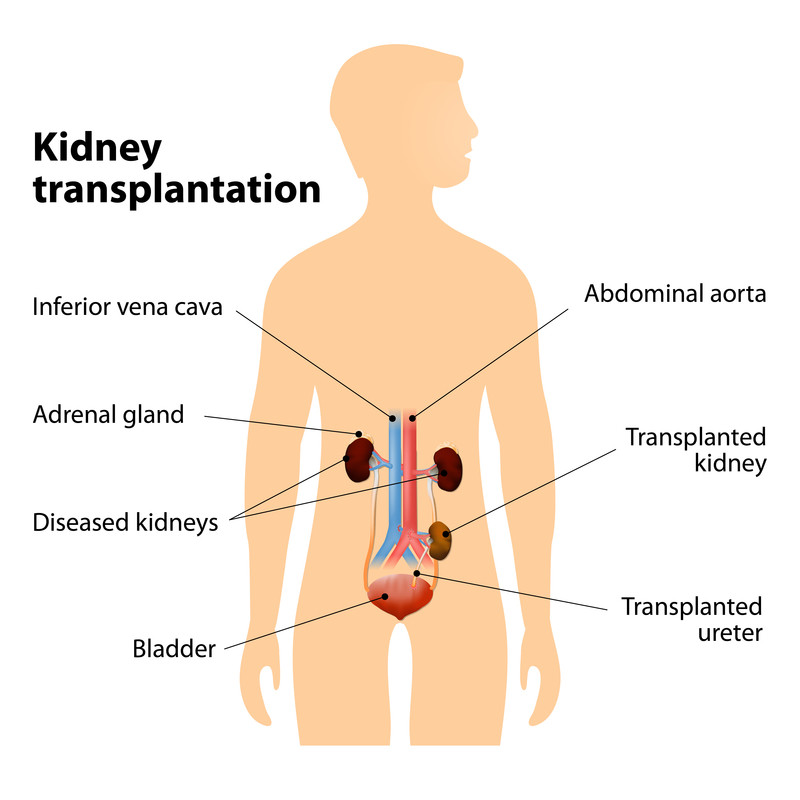
Kidney transplants
Kidney transplants allow people with severe kidney disease to avoid or discontinue dialysis.
Anyone who receives a kidney transplant must take immunosuppressive drugs for life, unless they received a kidney donated by their identical twin. These are drugs that prevent the body from rejecting the donated organ. In addition, a good genetic match is needed for a successful transplant. Most transplant candidates wait one to three to five years before a good genetic match can be found from an unrelated donor.
|
|
When to call a professional
You should have regular checkups if you have:
- diabetes
- high blood pressure
- other diseases that put you at risk of end-stage renal disease.
These checkups should include urine and blood tests to measure your kidney function.
When blood tests indicate kidney disease, your doctor should refer you to a kidney specialist. This specialist is called a nephrologist.
Call your doctor if you notice any decrease in urination or other symptoms of end-stage renal disease. Be particularly vigilant if you have kidney disease or its risk factors.
Prognosis
Treatments for end-stage renal disease offer hope for good recovery and quality of life. Although people requiring dialysis or who have had a kidney transplant have a somewhat shorter average lifespan than the general population, they can lead near normal lives for many years.
Additional info
National Institute of Diabetes & Digestive & Kidney Disorders
https://www.niddk.nih.gov/
National Kidney Foundation
https://www.kidney.org/
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.