Exjade Dosage
Generic name: DEFERASIROX 125mg
Dosage form: tablet, for suspension
Drug class: Chelating agents
Medically reviewed by Drugs.com. Last updated on Aug 12, 2025.
2.1 Transfusional Iron Overload
Exjade therapy should only be considered when a patient has evidence of chronic transfusional iron overload. The evidence should include the transfusion of at least 100 mL/kg of packed red blood cells (e.g., at least 20 units of packed red blood cells for a 40 kg person or more in individuals weighing more than 40 kg), and a serum ferritin consistently greater than 1,000 mcg/L.
Prior to starting therapy or increasing dose, evaluate:
- Serum ferritin level
- Baseline renal function:
- Obtain serum creatinine in duplicate (due to variations in measurements) to establish accurate baseline
- Calculate the estimated glomerular filtration rate (eGFR). Use a prediction equation appropriate for adult patients (e.g., CKD-EPI, MDRD method) and in pediatric patients (e.g., Schwartz equations).
- Obtain urinalyses and serum electrolytes to evaluate renal tubular function.
- Serum transaminases and bilirubin
- Baseline auditory and ophthalmic examinations
Initiating Therapy:
The recommended initial dose of Exjade for patients 2 years of age and older with eGFR greater than 60 mL/min/1.73 m2 is 20 mg per kg body weight orally, once daily. Calculate doses (mg per kg per day) to the nearest whole tablet.
During Therapy:
- Monitor serum ferritin monthly and adjust the dose of Exjade, if necessary, every 3-6 months based on serum ferritin trends.
- Use the minimum effective dose to achieve a trend of decreasing ferritin.
- Make dose adjustments in steps of 5 or 10 mg per kg and tailor adjustments to the individual patient’s response and therapeutic goals.
- In patients not adequately controlled with doses of 30 mg per kg (e.g., serum ferritin levels persistently above 2,500 mcg/L and not showing a decreasing trend over time), doses of up to 40 mg per kg may be considered. Doses above 40 mg per kg are not recommended.
- Adjust dose based on serum ferritin levels
- If the serum ferritin falls below 1,000 mcg/L at 2 consecutive visits, consider dose reduction, especially if the dose is greater than 25 mg/kg/day.
- If the serum ferritin falls below 500 mcg/L, interrupt Exjade to minimize the risk of overchelation, and continue monthly monitoring.
- Evaluate the need for ongoing chelation therapy for patients whose conditions no longer require regular blood transfusions.
- Use the minimum effective dose to maintain iron burden in the target range.
- Monitor blood counts, liver function, renal function and ferritin monthly.
- Interrupt Exjade for pediatric patients who have acute illnesses, which can cause volume depletion, such as vomiting, diarrhea, or prolonged decreased oral intake, and monitor more frequently. Resume therapy as appropriate, based on assessments of renal function, when oral intake and volume status are normal.
2.2 Iron Overload in Non-Transfusion-Dependent Thalassemia Syndromes
Exjade therapy should only be considered when a patient with NTDT syndrome has an LIC of at least 5 mg Fe/g dw and a serum ferritin greater than 300 mcg/L.
Prior to starting therapy, obtain:
- LIC by liver biopsy or by an FDA-cleared or approved method for identifying patients for treatment with deferasirox therapy
- Serum ferritin level on at least 2 measurements 1-month apart
- Baseline renal function:
- Obtain serum creatinine in duplicate (due to variations in measurements) to establish accurate baseline
- Calculate eGFR. Use a prediction equation appropriate for adult patients (e.g., CKD-EPI, MDRD method) and in pediatric patients (e.g., Schwartz equations).
- Obtain urinalyses and serum electrolytes to evaluate renal tubular function.
- Serum transaminases and bilirubin
- Baseline auditory and ophthalmic examinations
Initiating Therapy:
- The recommended initial dose of Exjade for patients with eGFR greater than 60 mL/min/1.73 m2 is 10 mg per kg body weight orally once daily. Calculate doses (mg per kg per day) to the nearest whole tablet.
- If the baseline LIC is greater than 15 mg Fe/g dw, consider increasing the dose to 20 mg/kg/day after 4 weeks.
During Therapy:
- Monitor serum ferritin monthly to assess the patient’s response to therapy and to minimize the risk of overchelation. Interrupt treatment when serum ferritin is less than 300 mcg/L and obtain an LIC to determine whether the LIC has fallen to less than 3 mg Fe/g dw.
- Use the minimum effective dose to achieve a trend of decreasing ferritin.
- Monitor LIC every 6 months.
- After 6 months of therapy, if the LIC remains greater than 7 mg Fe/g dw, increase the dose of deferasirox to a maximum of 20 mg/kg/day. Do not exceed a maximum of 20 mg/kg/day.
- If after 6 months of therapy, the LIC is 3-7 mg Fe/g dw, continue treatment with deferasirox at no more than 10 mg/kg/day.
- When the LIC is less than 3 mg Fe/g dw, interrupt treatment with deferasirox and continue to monitor the LIC.
- Monitor blood counts, liver function, renal function and ferritin monthly.
- Increase monitoring frequency for pediatric patients who have acute illness, which can cause volume depletion, such as vomiting, diarrhea, or prolonged decreased oral intake. Consider dose interruption until oral intake and volume status are normal.
Restart treatment when the LIC rises again to more than 5 mg Fe/g dw.
2.3 Administration
Do not chew tablets or swallow them whole.
Take Exjade once daily on an empty stomach at least 30 minutes before food, preferably at the same time each day. Completely disperse tablets by stirring in water, orange juice, or apple juice until a fine suspension is obtained. Disperse doses of less than 1 g in 3.5 ounces of liquid and doses of 1 g or greater in 7 ounces of liquid. After swallowing the suspension, resuspend any residue in a small volume of liquid and swallow. Do not take Exjade with aluminum-containing antacid products.
2.4 Use in Patients With Baseline Hepatic or Renal Impairment
Patients with Baseline Hepatic Impairment
Mild (Child-Pugh A) Hepatic Impairment: No dose adjustment is necessary.
Moderate (Child-Pugh B) Hepatic Impairment: Reduce the starting dose by 50%.
Severe (Child-Pugh C) Hepatic Impairment: Avoid Exjade.
Patients with Baseline Renal Impairment
Do not use Exjade in adult or pediatric patients with eGFR less than 40 mL/min/1.73 m2.
For patients with renal impairment (eGFR 40-60 mL/min/1.73 m2), reduce the starting dose by 50%.
Exercise caution in pediatric patients with eGFR between 40 and 60 mL/min/1.73 m2. If treatment is needed, use the minimum effective dose and monitor renal function frequently. Individualize dose titration based on improvement in renal injury.
2.5 Dose Modifications for Decreases in Renal Function While on Exjade
Exjade is contraindicated in patients with eGFR less than 40 mL/min/1.73 m2.
For decreases in renal function while receiving Exjade, modify the dose as follows:
Transfusional Iron Overload
Adults:
- If the serum creatinine increases by 33% or more above the average baseline measurement, repeat the serum creatinine within 1 week, and if still elevated by 33% or more, reduce the dose by 10 mg per kg.
Pediatric Patients (ages 2 years–17 years):
- Reduce the dose by 10 mg/kg/day if eGFR decreases by greater than 33% below the average baseline measurement and repeat the eGFR within 1 week.
- Interrupt Exjade for acute illnesses, which can cause volume depletion, such as vomiting, diarrhea, or prolonged decreased oral intake, and monitor more frequently. Resume therapy as appropriate, based on assessments of renal function, when oral intake and volume status are normal. Avoid use of other nephrotoxic drugs.
- In the setting of decreased renal function, evaluate the risk benefit profile of continued Exjade use. Use the minimum effective Exjade dose and monitor renal function more frequently, by evaluating tubular and glomerular function. Titrate dosing based on renal injury. Consider dose reduction or interruption and less nephrotoxic therapies until improvement of renal function. If signs of renal tubular or glomerular injury occur in the presence of other risk factors such as volume depletion, reduce or interrupt Exjade to prevent severe and irreversible renal injury.
All Patients (regardless of age):
- Discontinue therapy for eGFR less than 40 mL/min/1.73 m2.
Non-Transfusion-Dependent Thalassemia Syndromes
Adults:
- If the serum creatinine increases by 33% or more above the average baseline measurement, repeat the serum creatinine within 1 week, and if still elevated by 33% or more, interrupt therapy if the dose is 5 mg per kg, or reduce by 50% if the dose is 10 or 20 mg per kg.
Pediatric Patients (ages 10 years–17 years):
- Reduce the dose by 5 mg/kg/day if eGFR decreases by greater than 33% below the average baseline measurement and repeat the eGFR within 1 week.
- Increase monitoring frequency for pediatric patients who have acute illnesses, which can cause volume depletion, such as vomiting, diarrhea, or prolonged decreased oral intake. Consider dose interruption until oral intake and volume status are normal. Avoid use of other nephrotoxic drugs.
- In the setting of decreased renal function, evaluate the risk benefit profile of continued Exjade use. Use the minimum effective Exjade dose and monitor renal function more frequently, by evaluating tubular and glomerular function. Titrate dosing based on renal injury. Consider dose reduction or interruption and less nephrotoxic therapies until improvement of renal function. If signs of renal tubular or glomerular injury occur in the presence of other risk factors such as volume depletion, reduce or interrupt Exjade to prevent severe and irreversible renal injury.
All Patients (regardless of age):
- Discontinue therapy for eGFR less than 40 mL/min/1.73 m2.
2.6 Dose Modifications Based on Concomitant Medications
UDP-glucuronosyltransferases (UGT) Inducers
Concomitant use of UGT inducers decreases Exjade systemic exposure. Avoid the concomitant use of potent UGT inducers (e.g., rifampicin, phenytoin, phenobarbital, ritonavir) with Exjade. If you must administer Exjade with 1 of these agents, consider increasing the initial dose of Exjade by 50%, and monitor serum ferritin levels and clinical responses for further dose modification.
Bile Acid Sequestrants
Concomitant use of bile acid sequestrants decreases Exjade systemic exposure. Avoid the concomitant use of bile acid sequestrants (e.g., cholestyramine, colesevelam, colestipol) with Exjade. If you must administer Exjade with 1 of these agents, consider increasing the initial dose of Exjade by 50%, and monitor serum ferritin levels and clinical responses for further dose modification.
More about Exjade (deferasirox)
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (1)
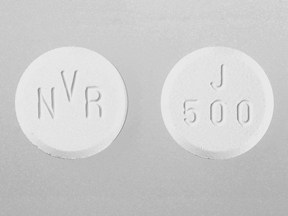
- Drug images
- Side effects
- During pregnancy
- Generic availability
- FDA approval history
- Drug class: chelating agents
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.