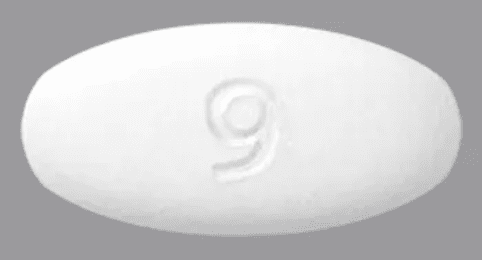
Pemigatinib (Oral)
Generic name: pemigatinib [ pem-i-GA-ti-nib ]
Brand name: Pemazyre
Drug class: Multikinase inhibitors
Medically reviewed by Drugs.com. Last updated on Feb 16, 2025.
Uses for pemigatinib
Pemigatinib is used to treat cholangiocarcinoma (bile duct cancer) that has spread or cannot be removed by surgery in patients who have already tried cancer treatment before and have a certain type of abnormal FGFR2 gene in their cancer. Your doctor will test for the presence of this gene.
Pemigatinib is also used to treat myeloid/lymphoid neoplasms (blood cancer) that has come back or did not respond to treatment in patients who have a certain type of abnormal FGFR1 gene in their cancer. Your doctor will test for the presence of this gene.
Pemigatinib is an antineoplastic (cancer) agent. It interferes with the growth of cancer cells, which are eventually destroyed by the body.
This medicine is available only with your doctor's prescription.
Before using pemigatinib
In deciding to use a medicine, the risks of taking the medicine must be weighed against the good it will do. This is a decision you and your doctor will make. For this medicine, the following should be considered:
Allergies
Tell your doctor if you have ever had any unusual or allergic reaction to this medicine or any other medicines. Also tell your health care professional if you have any other types of allergies, such as to foods, dyes, preservatives, or animals. For non-prescription products, read the label or package ingredients carefully.
Pediatric
Appropriate studies have not been performed on the relationship of age to the effects of pemigatinib in the pediatric population. Safety and efficacy have not been established.
Geriatric
Appropriate studies performed to date have not demonstrated geriatric-specific problems that would limit the usefulness of pemigatinib in the elderly.
Breast Feeding
There are no adequate studies in women for determining infant risk when using this medication during breastfeeding. Weigh the potential benefits against the potential risks before taking this medication while breastfeeding.
Interactions with Medicines
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are taking this medicine, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using this medicine with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Abametapir
- Apalutamide
- Aprepitant
- Atazanavir
- Boceprevir
- Bosentan
- Carbamazepine
- Cenobamate
- Ciprofloxacin
- Clarithromycin
- Cobicistat
- Conivaptan
- Crizotinib
- Cyclosporine
- Diltiazem
- Dronedarone
- Efavirenz
- Enzalutamide
- Erythromycin
- Etravirine
- Fedratinib
- Fexinidazole
- Fluconazole
- Fluvoxamine
- Fosnetupitant
- Fosphenytoin
- Idelalisib
- Imatinib
- Indinavir
- Itraconazole
- Ketoconazole
- Letermovir
- Lopinavir
- Lorlatinib
- Lumacaftor
- Mavacamten
- Mitotane
- Modafinil
- Nafcillin
- Nefazodone
- Nelfinavir
- Netupitant
- Nilotinib
- Omaveloxolone
- Phenobarbital
- Phenytoin
- Posaconazole
- Primidone
- Rifabutin
- Rifampin
- Ritonavir
- Saquinavir
- St John's Wort
- Telaprevir
- Telithromycin
- Verapamil
- Voriconazole
Interactions with Food/Tobacco/Alcohol
Certain medicines should not be used at or around the time of eating food or eating certain types of food since interactions may occur. Using alcohol or tobacco with certain medicines may also cause interactions to occur. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using this medicine with any of the following is usually not recommended, but may be unavoidable in some cases. If used together, your doctor may change the dose or how often you use this medicine, or give you special instructions about the use of food, alcohol, or tobacco.
- Grapefruit Juice
Other Medical Problems
The presence of other medical problems may affect the use of this medicine. Make sure you tell your doctor if you have any other medical problems, especially:
- Eye or vision problem (eg, retinal pigment epithelial detachment)—Use with caution. May make this condition worse.
- Kidney disease, severe or
- Liver disease, severe—Use with caution. The effects may be increased because of slower removal of the medicine from the body.
Proper use of pemigatinib
Medicines used to treat cancer are very strong and can have many side effects. Before using this medicine, make sure you understand all the risks and benefits. It is important for you to work closely with your doctor during your treatment.
Take this medicine exactly as directed by your doctor. Do not take more of it, do not take it more often, and do not take it for a longer time than your doctor ordered. To do so may increase the chance of side effects.
This medicine usually comes with a patient information leaflet. Read and follow the instructions carefully. Ask your doctor or pharmacist if you have any questions.
Take this medicine with or without food, about the same time each day. Pemigatinib is taken in cycles of 21 days.
Swallow the tablet whole with water. Do not crush, break, chew, or dissolve it.
Do not eat grapefruit or drink grapefruit juice while you are using this medicine.
Dosing
The dose of this medicine will be different for different patients. Follow your doctor's orders or the directions on the label. The following information includes only the average doses of this medicine. If your dose is different, do not change it unless your doctor tells you to do so.
The amount of medicine that you take depends on the strength of the medicine. Also, the number of doses you take each day, the time allowed between doses, and the length of time you take the medicine depend on the medical problem for which you are using the medicine.
- For oral dosage form (tablets):
- For cholangiocarcinoma (bile duct cancer):
- Adults—At first, 13.5 milligrams (mg) once a day for 14 days, followed by 7 days off treatment, to complete a 21-day treatment cycle. Your doctor may adjust your dose as needed and tolerated.
- Children—Use and dose must be determined by your doctor.
- For myeloid/lymphoid neoplasms (blood cancer):
- Adults—13.5 milligrams (mg) once a day. Your doctor may adjust your dose as needed and tolerated.
- Children—Use and dose must be determined by your doctor.
- For cholangiocarcinoma (bile duct cancer):
Missed Dose
If you miss a dose of this medicine, take it as soon as possible. However, if it is almost time for your next dose, skip the missed dose and go back to your regular dosing schedule. Do not double doses.
If it is less than 4 hours on the same day, take it as soon as you remember. If more than 4 hours have passed, skip the missed dose and go back to your regular dosing schedule. If you vomit after taking your medicine, do not take an extra dose.
Storage
Store the medicine in a closed container at room temperature, away from heat, moisture, and direct light. Keep from freezing.
Keep out of the reach of children.
Do not keep outdated medicine or medicine no longer needed.
Ask your healthcare professional how you should dispose of any medicine you do not use.
Precautions while using pemigatinib
It is very important that your doctor check your progress at regular visits. This will allow your doctor to see if the medicine is working properly and to decide if you should continue to take it. Blood and urine tests will be needed to check for unwanted effects.
Using this medicine while you are pregnant can harm your unborn baby. If you are a woman who can get pregnant, your doctor may do tests to make sure you are not pregnant before starting treatment. Use an effective form of birth control to keep from getting pregnant during treatment and for at least 1 week after your last dose. Males who are taking this medicine, with female partners who can become pregnant must use effective birth control during treatment and for at least 1 week after the last dose of this medicine. If you think you have become pregnant while using the medicine, tell your doctor right away.
Check with your doctor right away if eye pain, dryness, swelling, or a change in vision occurs during treatment. This could be a sign of a serious eye problem. Your doctor may want your eyes be checked by an ophthalmologist (eye doctor).
This medicine may cause hyperphosphatemia (high potassium levels in the blood). Check with your doctor right away it you have stomach cramps, confusion, seizures, difficulty in breathing, irregular heartbeat, mood or mental changes, muscle cramps in the hands, arms, feet, legs, or face, numbness and tingling around the mouth, fingertips, or feet, or tremor.
Do not take other medicines unless they have been discussed with your doctor. This includes prescription or nonprescription (over-the-counter [OTC]) medicines and herbal or vitamin supplements.
Side Effects of pemigatinib
Along with its needed effects, a medicine may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur:
More common
- Bladder pain
- bloody or cloudy urine
- bloody nose
- changes in the fingernails or toenails
- confusion
- decreased urination
- diarrhea
- difficult, burning, or painful urination
- difficulty in breathing
- dry eyes
- dry mouth
- eye redness, irritation, or pain
- frequent urge to urinate
- increase in heart rate
- irregular heartbeats
- lightheadedness, dizziness, fainting
- loosening of the fingernails
- loss of appetite
- lower back or side pain
- mood or mental changes
- muscle cramps in the hands, arms, feet, legs, or face
- numbness and tingling around the mouth, fingertips, or feet
- pain in the bones
- pale skin
- rapid breathing
- redness or soreness around the fingernails
- seeing flashes or sparks of light
- seeing floating spots before the eyes, or a veil or curtain across part of your vision
- seizures
- stomach cramps
- sunken eyes
- swelling of the hands, ankles, feet, or lower legs
- thirst
- tremor
- unusual bleeding or bruising
- unusual tiredness or weakness
- unusual weight loss
- wrinkled skin
Less common
- Pain or swelling in the arms or legs without any injury
Some side effects may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects. Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common
- Acid or sour stomach
- belching
- bloating or swelling of the face, arms, hands, lower legs, or feet
- changes in taste
- constipation
- difficulty in moving
- dry skin
- hair loss
- heartburn
- indigestion
- loss of taste
- nausea
- pain in the joints
- rapid weight gain
- redness, swelling, pain of the skin
- scaling of the skin on the hands and feet
- stomach discomfort, upset, or pain
- swelling or inflammation of the mouth
- ulceration of the skin
- vomiting
Other side effects not listed may also occur in some patients. If you notice any other effects, check with your healthcare professional.
Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.
Related/similar drugs
Commonly used brand name(s)
In the U.S.
- Pemazyre
Available Dosage Forms:
- Tablet
Therapeutic Class: Antineoplastic Agent
Pharmacologic Class: Tyrosine Kinase Inhibitor
More about pemigatinib
- Check interactions
- Compare alternatives
- Reviews (1)
- Side effects
- Dosage information
- During pregnancy
- Drug class: multikinase inhibitors
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.