Sepsis
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
Sepsis is a condition that develops when your immune system reacts too strongly to an infection. Your immune system normally fights the germs causing an infection. Sepsis develops when your immune system stops attacking the germs and starts attacking healthy cells throughout your body. This causes a low blood pressure (BP) and inflammation. Sepsis is considered severe if the inflammation affects how one or more of your organs work. Sepsis must be treated immediately to prevent septic shock. Septic shock is sepsis with a life-threatening low BP that leads to organ failure.
WHILE YOU ARE HERE:
Informed consent
is a legal document that explains the tests, treatments, or procedures that you may need. Informed consent means you understand what will be done and can make decisions about what you want. You give your permission when you sign the consent form. You can have someone sign this form for you if you are not able to sign it. You have the right to understand your medical care in words you know. Before you sign the consent form, understand the risks and benefits of what will be done. Make sure all your questions are answered.
Monitoring:
Healthcare providers will closely monitor your blood pressure, heart rate, breathing rate, temperature, and pain. You will have an IV line used to give medicines or liquid, or to draw blood samples. Providers will also check your kidney function by measuring how much you are urinating.
Medicines:
You may be given medicine to do any of the following:
- Increase your blood pressure and blood flow to your organs
- Treat the infection causing sepsis
- Control or lower your heart rate
- Prevent blood clots
Related medications
Treatment
may include any of the following:
- Removal of any device or tissue that may be causing the infection
- Oxygen or a breathing machine (ventilator) to provide breathing support
- Pneumatic boots to help prevent blood clots
- An IV for nutrition and fluid support
- A blood transfusion to replace red blood cells damaged or lost due to bleeding
- Dialysis for kidney support if your kidneys are not working properly
Treatment options
The following list of medications are related to or used in the treatment of this condition.
Tests:
- An x-ray, ultrasound, CT, or MRI may show the source of infection. You may be given contrast liquid to help the infection show up better in the pictures. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid. Do not enter the MRI room with anything metal. Metal can cause serious injury. Tell the healthcare provider if you have any metal in or on your body.
- Blood and urine tests will show infection, organ function, and give information about your overall health. A blood test may also show what germ is causing your illness.
- Blood gases will show how much oxygen and carbon dioxide are in your blood. The results will tell healthcare providers how well your lungs, heart, and kidneys are working.
- An echocardiogram is a type of ultrasound. Sound waves are used to show the structure and function of your heart. The test will also check for damage to your heart valves that may be caused by infection.
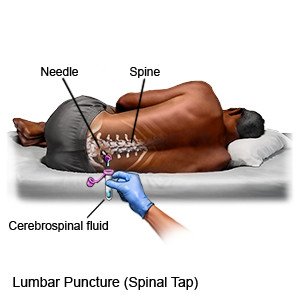
- A lumbar puncture (spinal tap) may be done to test your cerebrospinal fluid (CSF) for germs. It can also check for signs of infection in or around your brain. CSF surrounds your spinal column and your brain.
RISKS:
Without treatment, sepsis may develop into septic shock (sepsis with low blood pressure). Multiple organs may shut down. These problems can be life-threatening. Your organs may be permanently damaged by septic shock.
CARE AGREEMENT:
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Sepsis
Treatment options
Care guides
Medicine.com guides (external)
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
