Myocarditis
Medically reviewed by Drugs.com. Last updated on Sep 23, 2025.
Myocarditis is inflammation of the heart muscle (myocardium). The myocardium pumps blood through the heart and to other parts of the body. Myocarditis can damage the heart muscle. This weakens the heart and makes it work harder. Over time, this may cause your heart to enlarge, lead to heart failure, and become life-threatening.
DISCHARGE INSTRUCTIONS:
Call your local emergency number (911 in the US) if:
- You have any of the following signs of a heart attack:
- Squeezing, pressure, or pain in your chest
- You may also have any of the following:
- Discomfort or pain in your back, neck, jaw, stomach, or arm
- Shortness of breath
- Nausea or vomiting
- Lightheadedness or a sudden cold sweat
Seek care immediately if:
- Your heart is beating faster than usual, fluttering, or jumping in your chest.
- You are tired and cannot think clearly.
- You have increased swelling in your legs, ankles, or feet.
Call your doctor if:
- Your signs and symptoms come back or get worse.
- You have a fever.
- You have chills, a cough, or feel weak and achy.
- You have questions or concerns about your condition or care.
Medicines:
You may need any of the following:
- Aspirin helps thin the blood to keep clots from forming. If you are told to take aspirin, do not take acetaminophen or ibuprofen instead. This medicine makes it more likely for you to bleed or bruise.
- Blood thinners help prevent blood clots. Clots can cause strokes, heart attacks, and death. Many types of blood thinners are available. Your healthcare provider will give you specific instructions for the type you are given. The following are general safety guidelines to follow while you are taking a blood thinner:
- Watch for bleeding and bruising. Watch for bleeding from your gums or nose. Watch for blood in your urine and bowel movements. Use a soft washcloth on your skin, and a soft toothbrush to brush your teeth. This can keep your skin and gums from bleeding. If you shave, use an electric shaver. Do not play contact sports.
- Tell your dentist and other healthcare providers that you take a blood thinner. Wear a bracelet or necklace that says you take this medicine.
- Do not start or stop any other medicines or supplements unless your healthcare provider tells you to. Many medicines and supplements cannot be used with blood thinners.
- Take your blood thinner exactly as prescribed by your healthcare provider. Do not skip a dose or take less than prescribed. Tell your provider right away if you forget to take your blood thinner, or if you take too much.
- Blood pressure medicine helps lower your blood pressure to reduce the strain on your heart.
- Diuretics may be given to help decrease edema (excess fluid) that collects in a part of your body, such as your legs. Diuretics can also remove excess fluid from around your heart or lungs and decrease your blood pressure. You may urinate more often when you take diuretics.
- Heart medicine may be given to reduce the strain on your heart and regulate your heart rate.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
Treatment:
In addition to medicines, your healthcare provider may recommend a procedure or surgery. Ask for information about each treatment. The following may be used to treat myocarditis:
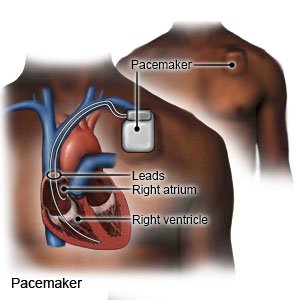
- A pacemaker is a device that helps your heart beat at a regular rate and rhythm. The pacemaker monitors your heart rhythm. If your heart does not beat as it should, the pacemaker sends small electric signals to your heart.
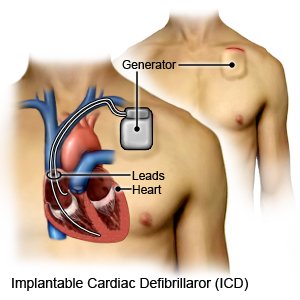
- An implanted cardioverter defibrillator (ICD) is a small device that monitors your heart rate and rhythm. If your ICD senses that your heart is not beating correctly, it will give it a small electrical shock. This helps your heart to beat regularly again.
- Heart transplant surgery may be needed if your condition is severe. During a heart transplant, your damaged heart is removed and replaced with a healthy heart from a donor.
Help protect your heart:
- Limit physical activity. Your healthcare provider may suggest that you rest until your symptoms decrease. Your provider may suggest that you avoid heavy lifting or certain physical activities. Ask which activities are safe for you, when to begin exercise, and the best exercise plan for you.
- Eat a variety of heart-healthy foods. Heart-healthy foods are high in potassium, calcium, magnesium, and fiber. These nutrients are added when you eat more fruits, vegetables, and whole grains. Heart-healthy fats can be found in walnuts, salmon, and canola or soybean oil. Limit foods high in sugar, saturated and trans fats, and total fat.

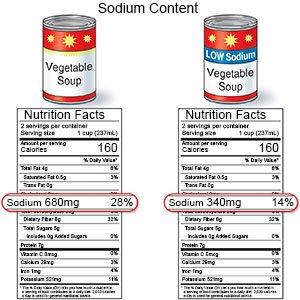
- Limit sodium (salt) as directed. Too much sodium can cause swelling and make your symptoms worse. Ask how much sodium you can have each day. Pay attention to sodium content on food labels.
- Do not drink alcohol, smoke cigarettes, or use drugs. Alcohol, cigarettes, or illegal drugs can damage your heart and worsen your symptoms. Ask for information if you currently use any of these and need help quitting.
Prevent infections:
 |
- Wash your hands often. Wash your hands several times each day. Wash after you use the bathroom, change a child's diaper, and before you prepare or eat food. Use soap and water every time. Rub your soapy hands together, lacing your fingers. Wash the front and back of your hands, and in between your fingers. Use the fingers of one hand to scrub under the fingernails of the other hand. Wash for at least 20 seconds. Rinse with warm, running water for several seconds. Then dry your hands with a clean towel or paper towel. Use hand sanitizer that contains alcohol if soap and water are not available. Do not touch your eyes, nose, or mouth without washing your hands first.

- Cover a sneeze or cough. Use a tissue that covers your mouth and nose. Throw the tissue away in a trash can right away. Use the bend of your arm if a tissue is not available. Wash your hands well with soap and water or use a hand sanitizer.
- Avoid crowds and sick people. This will reduce your risk for infection.
- Do not share items. Do not share towels, razors, or toothbrushes with other people. Avoid sharing utensils, drinks, and food.
- Clean surfaces often. Clean doorknobs, countertops, cell phones, and other surfaces that are touched often. Use a disinfecting wipe, a single-use sponge, or a cloth you can wash and reuse. Use disinfecting cleaners if you do not have wipes. You can create a disinfecting cleaner by mixing 1 part bleach with 10 parts water.
- Ask about vaccines you may need. Certain vaccines can help protect you from infections that can cause serious illness in a person who has myocarditis. Your healthcare provider can tell you which vaccines are right for you. Your provider can also tell you if you should get vaccines not listed below, and when to get them.
- COVID-19 vaccines are given to adults as a shot. At least 1 dose of an updated vaccine is recommended for all adults. COVID-19 vaccines are updated throughout the year. Adults 65 or older need a second dose of updated vaccine at least 4 months after the first dose. Your healthcare provider can help you schedule all needed doses as updated vaccines become available.
- Ask your healthcare provider about the flu and pneumonia vaccines. All adults should get the flu (influenza) vaccine as soon as recommended each year, usually in September or October. The pneumonia vaccine is recommended for all adults aged 50 or older to prevent pneumococcal disease, such as pneumonia. Adults aged 19 to 49 years who are at high risk for pneumococcal disease should also receive the vaccine. You may need 1 dose or 2. The number depends on the vaccine used and your risk factors.
Follow up with your doctor as directed:
Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Myocarditis
- Atorvastatin (Lipitor): Top 12 Drug Facts You Need to Know
- Do blood pressure drugs interact with alcohol?
- Side Effects of Weight Loss Drugs
Treatment options
Care guides
Medicine.com guides (external)
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
