Hypocalcemia
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
Hypocalcemia is a low level of calcium in your blood. Your body may lose too much calcium or not absorb enough from the foods you eat.
DISCHARGE INSTRUCTIONS:
Call your local emergency number (911 in the US) or have someone call if:
- You have a seizure.
- You see or hear things that are not really there.
Return to the emergency department if:
- You have a slow or uneven heartbeat and feel lightheaded.
Call your doctor or endocrinologist if:
- You have dry skin and brittle nails.
- Your symptoms do not go away, or they get worse.
- You feel depressed, anxious, angry, or confused.
- You have questions or concerns about your condition or care.
Related medications
Treatment options
The following list of medications are related to or used in the treatment of this condition.
Medicines:
- Medicines will be given to bring your calcium and vitamin D levels back to normal. You may also need medicines to prevent bone loss.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
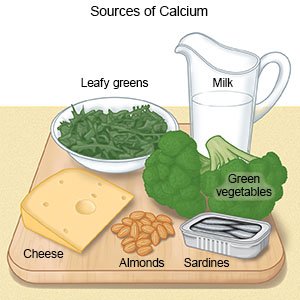
Eat foods rich in calcium:
Foods that contain calcium include milk, yogurt, cereals, and cheese. Leafy green vegetables, oranges, canned salmon, shrimp, and peanuts also contain calcium. Do not have caffeine or alcohol. These can slow your body's ability to absorb calcium. You may need to meet with a dietitian to help plan the best meals for you.
 |
Get safe amounts of sunlight:
You may need to expose your skin to more sunlight to get more vitamin D. Ask your healthcare provider how to safely expose yourself to UV light if you need it.
Do not smoke:
Nicotine and other chemicals in cigarettes and cigars can worsen hypocalcemia. Ask your provider for information if you currently smoke and need help to quit. E- cigarettes and smokeless tobacco still contain nicotine. Talk to your provider before you use these products.
Follow up with your doctor or endocrinologist every 3 to 6 months, or as directed:
You will need to return to have your calcium levels checked. Bring a list of any questions you have so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Hypocalcemia
Treatment options
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
