Chronic Abdominal Pain in Children
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
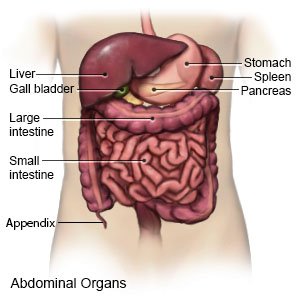
What is chronic abdominal pain?
Chronic abdominal pain happens at least 3 times in 3 months.
 |
What are different types of chronic abdominal pain in children?
- Abdominal migraine is severe abdominal pain with nausea, vomiting, or loss of appetite.
- Functional abdominal pain is pain that has no known cause. Your child may not want to do his or her daily activities because of the pain.
- Functional dyspepsia is upper abdominal pain that does not go away when your child has a bowel movement.
- Irritable bowel syndrome (IBS) is abdominal pain that goes away when your child has a bowel movement. Your child's bowel movements may also look different, or he or she may have more bowel movements than usual.
What causes chronic abdominal pain in children?
The cause of your child's pain may not be found. The following are common causes:
- Inflammation of the esophagus or stomach
- An infection such as a parasite or a urinary tract infection (UTI)
- Menstrual cycle (period) for females
- Anxiety or stress
- Constipation or lactose intolerance
- Crohn disease
- Kidney stones or gallstones
What are the signs and symptoms of chronic abdominal pain?
Signs and symptoms may come and go. Your child may feel pain in all areas of his or her abdomen or just in 1 area. He or she may not want to eat. He or she may not want to do his or her daily activities, such as school or sports. He or she may also have any of the following:
- Cramping
- Bloating and gas
- Constipation or diarrhea
- Slow growth or growth failure
- Nausea or vomiting
How is the cause of chronic abdominal pain diagnosed?
Your child's healthcare provider will ask about your child's family history of abdominal pain. Tell him or her if your child takes any medicines, and how well he or she eats and sleeps. Tell him or her if your child has any other health problems or has missed activities because of the pain. Tell him or her if your child has been stressed or worried lately. Your child may also need any of the following:
- Blood, urine, or bowel movement tests may be used to check for a disease or infection that may be causing pain.
- Ultrasound, x-ray, CT, or MRI pictures may be used to check for problems such as blocked intestines. Your child may be given contrast liquid to help healthcare providers see any problems better. Tell the healthcare provider if your child has ever had an allergic reaction to contrast liquid. Do not let your child enter the MRI room with anything metal. Metal can cause serious injury. Tell the provider if your child has any metal in or on his or her body.
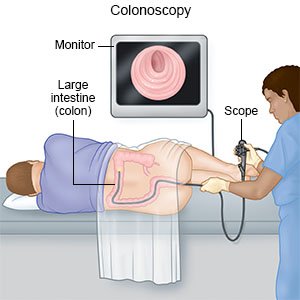
- A colonoscopy is used to check your child's colon. A tube with a light on the end will be put into your child's anus. The tube is then moved up into his or her colon. Problems may be treated during the colonoscopy.
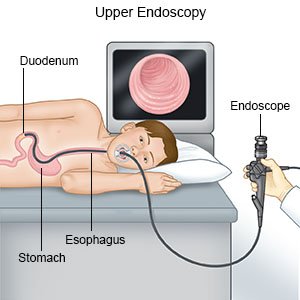
- An endoscopy is used to check your child's digestive tract. A scope is a long, bendable tube with a light on the end. A camera may be hooked to the scope so the healthcare provider can take pictures. Samples may be taken from your child's digestive tract and sent to a lab for tests. Problems may be treated during the endoscopy.
- A food elimination test is used to check for celiac disease or irritable bowel syndrome (IBS). For this test, your child will not eat or drink anything that contains lactose. Examples include milk and cheese. This will continue for a few days to see if your child's symptoms improve. More tests are used to find if your child has celiac disease or IBS.
- A breath test is used to check for problems your child may have with absorbing nutrients.
How is chronic abdominal pain treated?
Healthcare providers may not find a medical problem that is causing your child's pain. If no problem is found, they will work to decrease your child's symptoms so he or she can return to his or her regular activities. With treatment, your child's abdominal pain may decrease, happen less often, or go away. Your child may need any of the following:
- Medicines may be given to help calm your child's stomach and prevent vomiting. Medicines may be given to control your child's anxiety or to lower stomach acid. Medicines may also be given to prevent or treat pain or a bacterial infection.
- Surgery is rarely needed but may be done to treat certain problems.
How can I help manage my child's chronic abdominal pain?
Your child's healthcare provider may give you specific instructions based on your child's age. The following are general guidelines:
- Apply heat on your child's abdomen to help with pain or muscle spasms. You can apply heat with an electric heating pad set on low, a hot water bottle, or a warm compress. Heat should be applied for about 20 to 30 minutes or as long and as often as directed. Always put a cloth between your child's skin and the heat pack to prevent burns.
- Keep track of your child's abdominal pain. This may help your child's healthcare provider learn what is causing the pain. Track when the pain happens, how long it lasts, and how your child describes the pain. Include any other symptoms he or she has with abdominal pain. Also include what your child eats and drinks, and any symptoms that develop after he or she eats.
- Make changes to the foods you give your child, if needed. Do not give foods that cause abdominal pain or other symptoms. Have your child eat small meals more often. The following changes may also help:
- Give more high-fiber foods if your child is constipated. High-fiber foods include fruits, vegetables, whole-grain foods, and legumes such as pinto beans.

- Do not give foods or drinks that cause gas if your child has bloating. Examples include broccoli, cabbage, beans, and carbonated drinks.
- Do not give foods or drinks that contain sorbitol or fructose if your child has diarrhea. Some examples are fruit juices, candy, jelly, and sugar-free gum.
- Do not give high-fat foods. Examples include fried foods, cheeseburgers, hot dogs, and desserts.
- Give more high-fiber foods if your child is constipated. High-fiber foods include fruits, vegetables, whole-grain foods, and legumes such as pinto beans.
- Make changes to the liquids your child drinks, if needed. Do not give liquids that cause pain or make it worse, such as orange juice. The following changes may also help:
- Give your child more liquid, as directed. Give your child liquids throughout the day to help him or her stay hydrated. Ask how much liquid your child should drink each day and which liquids are best for him or her.
- Do not give your child liquid that contains caffeine. Caffeine may make symptoms such as heartburn or nausea worse.
- Help your child manage stress. Stress may cause abdominal pain or make it worse. Your child's healthcare provider may recommend relaxation techniques and deep breathing exercises to help decrease stress. The provider may recommend your child talk to someone about stress or anxiety, such as a counselor or a friend. Help your child get plenty of sleep and physical activity.
When should I seek immediate care?
- Your child's abdominal pain gets worse and spreads to his or her back.
- Your child's bowel movement has blood in it, or looks like black tar.
- Your child cannot stop vomiting, or vomits blood.
- Your child has diarrhea for at least 1 week.
- Your child has trouble breathing, and his or her skin looks pale.
- Your child's pain wakes him or her during the night.
- Your child has trouble swallowing, or pain when he or she swallows.
When should I call my child's doctor?
- Your child has pain on his or her right side that does not go away.
- Your child has a fever.
- Your child is not drinking liquids, and he or she is not urinating.
- You have questions or concerns about your child's condition or care.
Care Agreement
You have the right to help plan your child's care. Learn about your child's health condition and how it may be treated. Discuss treatment options with your child's healthcare providers to decide what care you want for your child. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Chronic Abdominal Pain
Treatment options
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
