Venlafaxine (Monograph)
Brand name: Effexor XR
Drug class: Selective Serotonin- and Norepinephrine-reuptake Inhibitors
Warning
- Suicidal Thoughts and Behaviors
-
Antidepressants may increase risk of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults (18–24 years of age) with major depressive disorder and other psychiatric disorders; balance this risk with clinical need. Venlafaxine is not approved for use in pediatric patients.
-
Studies did not find an increased risk of suicidality in adults >24 years of age and found a reduced risk of suicidality in adults ≥65 years of age with antidepressant therapy compared with placebo.
-
Closely monitor and observe all patients who are started on venlafaxine therapy for clinical worsening or emergence of suicidal thoughts and behaviors, especially during the initial few months of therapy and at times of dosage changes; involve family members and/or caregivers in this process.
Introduction
A selective serotonin- and norepinephrine-reuptake inhibitor (SNRI); antidepressant and anxiolytic agent.
Uses for Venlafaxine
Major Depressive Disorder
Used orally (as venlafaxine hydrochloride conventional tablets, venlafaxine hydrochloride extended-release capsules, venlafaxine hydrochloride extended-release tablets, and venlafaxine besylate extended-release tablets) for the treatment of major depressive disorder in adults.
Guidelines from the American Psychiatric Association (APA) and the Department of Veterans Affairs/Department of Defense state that there is no evidence to suggest superiority of one first-line antidepressant over another. Recommended first-line agents for initial treatment of major depressive disorder include bupropion, mirtazapine, selective serotonin-reuptake inhibitors (SSRIs), SNRIs, trazodone, vilazodone, or vortioxetine. Select an initial antidepressant for treatment based on patient preference, response to prior therapies, and other patient- and drug-related factors.
The manufacturer states that venlafaxine is not approved for use in pediatric patients.
Generalized Anxiety Disorder
Used orally (as venlafaxine hydrochloride extended-release capsules [Effexor XR] and venlafaxine besylate extended-release tablets) for the treatment of generalized anxiety disorder in adults.
Has been used for the treatment of generalized anxiety disorder in pediatric patients ≥6 years of age† [off-label] .
International experts state that the SSRIs escitalopram, paroxetine, and sertraline, as well as the SNRIs venlafaxine and duloxetine, are first-line treatments for generalized anxiety disorder in adults.
Guidelines from the American Academy of Child and Adolescent Psychiatry (AACAP) recommend an SSRI be offered to pediatric patients 6-18 years of age with generalized anxiety disorder if pharmacotherapy is indicated. AACAP suggests that duloxetine or venlafaxine may also be offered.
Social Anxiety Disorder
Used orally (as venlafaxine hydrochloride extended-release capsules [Effexor XR] and extended-release tablets) for the treatment of social anxiety disorder in adults.
Has been used for the treatment of social anxiety disorder in pediatric patients ≥6 years of age† [off-label] .
Guidelines from international experts state that escitalopram, fluvoxamine, paroxetine, sertraline, and venlafaxine are recommended first-line agents for the pharmacological treatment of social anxiety disorder in adults.
Guidelines from AACAP recommend an SSRI be offered to pediatric patients 6-18 years of age with social anxiety disorder if pharmacotherapy is indicated. AACAP suggests that duloxetine or venlafaxine may also be offered.
Panic Disorder
Used orally (as venlafaxine hydrochloride extended-release capsules [Effexor XR]) for the treatment of panic disorder in adults.
Has been used for the treatment of panic disorder in pediatric patients ≥6 years of age† [off-label] .
Legacy guidelines from APA state that SSRIs, SNRIs, tricyclic antidepressants (TCAs), benzodiazepines, and cognitive behavioral therapy have all demonstrated efficacy for the initial treatment of panic disorder in adults. Choice of initial therapy should be based on patient preference, past treatment history, the presence of comorbid medical or psychiatric conditions, potential adverse effects, potential drug interactions, cost, and treatment availability. For patients who prefer to initiate pharmacological treatment, SSRIs and SNRIs are typically recommended first line. Updated guidelines from international experts state that first-line medications for treatment of panic disorder include citalopram, escitalopram, fluvoxamine, fluoxetine, paroxetine, sertraline, and venlafaxine.
AACAP guidelines recommend an SSRI be offered to pediatric patients 6-18 years of age with panic disorder if pharmacotherapy is indicated. Duloxetine and venlafaxine may also be offered.
Vasomotor Symptoms
Has been used for the treatment of vasomotor symptoms† [off-label] in women with breast cancer in postmenopausal women; improved both frequency and severity of vasomotor symptoms (hot flushes [flashes]). Has also been used in men with cancer.
Guidelines from the American Society of Clinical Oncology (ASCO) provide recommendations for women and men with cancer for interventions to address sexual problems. For women, hormone therapy is most effective for vasomotor symptoms; alternatives (paroxetine, venlafaxine, gabapentin, or clonidine) may be offered if hormone therapy is contraindicated. For men with cancer and vasomotor symptoms, venlafaxine, medroxyprogesterone acetate, cyproterone acetate, and gabapentin may be offered for symptomatic improvement.
Guidelines from the American College of Obstetricians and Gynecologists (ACOG), the Endocrine Society, and the North American Menopause Society provide recommendations for management of menopausal vasomotor symptoms. For women who cannot or choose not to take systemic hormone therapy, SSRIs, SNRIs (including venlafaxine), gabapentin, and fezolinetant may be effective for vasomotor symptoms.
Posttraumatic Stress Disorder
Has been used for the treatment of PTSD† [off-label] in adults.
Guidelines from the Department of Veterans Affairs/Department of Defense state that paroxetine, sertraline, or venlafaxine are first-line pharmacotherapy options for PTSD. International experts state that first-line medications for the treatment of PTSD include SSRIs (fluoxetine, paroxetine, sertraline) and venlafaxine.
Other Uses
Has been used for the treatment of premenstrual disorders† .
ACOG guidelines recommend SSRIs first-line for management of affective premenstrual symptoms; there is limited evidence that venlafaxine also improves premenstrual symptoms.
Has been used for the treatment of neuropathic pain in patients with diabetes† .
American Diabetes Association (ADA) guidelines recommend gabapentinoids, SNRIs (e.g., duloxetine, venlafaxine, desvenlafaxine), TCAs, and sodium channel blockers as initial pharmacologic treatments for neuropathic pain in patients with diabetes.
Has been used for the treatment of OCD† in adults.
APA guidelines state that patients may switch to another SSRI or venlafaxine, mirtazapine, or clomipramine as a second-line treatment if they fail to respond to initial treatment with an SSRI. International experts provide a limited recommendation for use of venlafaxine in OCD.
Has been used for the prevention of migraines† in adults.
Guidelines from the American Academy of Neurology (AAN) and American Headache Society (AHS) list several medications as effective, probably effective, and possibly effective for migraine prevention. Among several other medications (including amitriptyline, atenolol, and naratriptan), venlafaxine is listed as probably effective and should be considered for migraine prevention. Guidelines from the Department of Veterans Affairs/Department of Defense state there is insufficient evidence to recommend for or against venlafaxine for the prevention of headache.
Venlafaxine Dosage and Administration
General
Pretreatment Screening
-
Screen for a personal or family history of bipolar disorder, mania, or hypomania.
Patient Monitoring
-
Monitor for possible worsening of depression, suicidality, or unusual changes in behavior, especially at the beginning of therapy or during periods of dosage adjustment.
-
Monitor for the emergence of serotonin syndrome during therapy.
-
Monitor blood pressure and lipids periodically during venlafaxine therapy.
-
Monitor coagulation indices for patients taking warfarin and initiating, titrating, or discontinuing venlafaxine.
-
Monitor for withdrawal symptoms when discontinuing venlafaxine.
-
Monitor for signs of hyponatremia.
-
Monitor for changes in height, weight, and appetite, including in pediatric patients.
Dispensing and Administration Precautions
-
The Institute for Safe Medication Practices (ISMP) recommends special safeguards to reduce the risk of errors when prescribing venlafaxine (Effexor) and venlafaxine extended-release (Effexor XR); these may include strategies such as using both brand and generic names on prescriptions/labels and including the purpose of the medication on prescriptions.
Other General Considerations
-
Patients receiving venlafaxine hydrochloride conventional tablets may switch to venlafaxine hydrochloride extended-release tablets or capsules at the nearest equivalent dose (mg per day); individual dosage adjustments may be necessary.
-
Patients receiving venlafaxine hydrochloride conventional tablets may switch to venlafaxine besylate extended-release tablets at the nearest equivalent dose (mg per day) if the total daily dosage is either 112.5 mg or 225 mg once daily.
-
Do not initiate treatment with venlafaxine besylate extended-release tablets as this product is not available at a strength <112.5 mg. Therapy with venlafaxine besylate extended-release tablets may be initiated in patients who have received at least 75 mg per day of another venlafaxine extended-release product for at least 4 days.
-
If a patient is being transitioned to venlafaxine therapy from a monoamine oxidase inhibitor (MAOI), allow at least 14 days to elapse between discontinuation of the MAOI and initiation of venlafaxine. Conversely, if switching from venlafaxine to an MAOI, allow at least 7 days to elapse between discontinuation of venlafaxine and initiation of the MAOI.
-
Do not initiate venlafaxine in patients receiving linezolid or IV methylene blue; if urgent treatment with linezolid or IV methylene blue is required, stop venlafaxine and monitor for symptoms of serotonin syndrome for 7 days or until 24 hours after the last dose of linezolid or IV methylene blue (whichever comes first). Resume venlafaxine 24 hours after the last dose of linezolid or IV methylene blue.
-
When discontinuing therapy, reduce dosage gradually and monitor for possible withdrawal symptoms; avoid abrupt discontinuation whenever possible. Given that venlafaxine besylate extended-release tablet strengths are not available below 112.5 mg, use another venlafaxine extended-release product (i.e., venlafaxine hydrochloride extended-release tablets or capsules) for dose reduction during discontinuation of venlafaxine besylate extended-release tablets.
Administration
Oral Administration
Administer orally with food.
Administer conventional tablets twice or 3 times daily with food.
Administer extended-release capsules or tablets as a single daily dose with food at approximately the same time each day (morning or evening). Swallow extended-release capsules and tablets whole with fluid; do not divide, crush, chew, or place in water.
Alternatively, open extended-release capsule(s) and sprinkle on a small amount of applesauce; swallow immediately without chewing. After administration, the patient should drink a glass of water to ensure that the pellets are completely swallowed.
Dosage
Available as venlafaxine hydrochloride and venlafaxine besylate; dosage expressed in terms of venlafaxine.
Adults
Major Depressive Disorder
Oral
Initially, 75 mg daily administered in 2 or 3 divided doses as conventional tablets or as a single daily dose when using the extended-release capsules or tablets. Alternatively, an initial dosage of 37.5 mg daily as extended-release capsules for the first 4–7 days (followed by an increase to 75 mg daily) may be considered for some patients. If no improvement, dosage may be increased by increments of up to 75 mg daily at intervals of not less than 4 days up to a maximum dosage of 375 mg daily (usually administered in 3 divided doses) as conventional tablets or 225 mg daily as extended-release capsules or tablets.
No additional benefit demonstrated from dosages >225 mg daily as conventional tablets in clinical studies in moderately depressed outpatients, but patients with more severe depression responded to higher dosages (mean dosage of 350 mg daily).
If desired, conventional tablets may be switched to the extended-release capsules or tablets at the nearest equivalent daily venlafaxine dosage (e.g., change 37.5 mg administered twice daily as conventional tablets to 75-mg extended-release capsule or tablet administered once daily). Individualize dosage adjustments as necessary.
May initiate venlafaxine besylate extended-release tablets at a dosage of 112.5 mg once daily if patient has received at least 75 mg per day of another venlafaxine extended-release product for at least 4 days.
Generalized Anxiety Disorder
Oral
Initially, 75 mg once daily as extended-release capsules. In some patients, it may be desirable to initiate therapy with a dosage of 37.5 mg daily given for the first 4–7 days, followed by an increase to 75 mg daily. If no improvement, dosage may be increased in increments of up to 75 mg daily (up to a maximum dosage of 225 mg daily as extended-release capsules) at intervals of not less than 4 days.
May initiate venlafaxine besylate extended-release tablets at a dosage of 112.5 mg once daily if patient has received at least 75 mg per day of another venlafaxine extended-release product for at least 4 days.
Social Anxiety Disorder
Oral
Initially, 75 mg once daily as extended-release capsules or tablets. No evidence that higher dosages of venlafaxine confer additional benefit.
Panic Disorder
Oral
Initially, 37.5 mg once daily as extended-release capsules for 7 days. If no improvement, dosage may be increased in increments of up to 75 mg daily at intervals of not less than 7 days. In clinical trials, 37.5 mg once daily was given initially for 7 days, then 75 mg once daily for 7 days; thereafter, dosage was increased in increments of 75 mg daily every 7 days if necessary. Certain patients not responding to 75 mg once daily may benefit from dosage increases up to a maximum of approximately 225 mg daily.
Vasomotor Symptoms
Oral
Optimum dosage for vasomotor symptoms† in women with breast cancer and in postmenopausal women not established. Some clinicians recommend initial dosage of 37.5 mg once daily as extended-release capsules; may increase as necessary to 75 mg once daily. 75 mg once daily as extended-release capsules appeared optimal in one study. Further dosage increases may not provide additional benefit but are potentially more toxic.
PTSD
Oral
Optimum dosage for PTSD† in adults not established. Initially, some clinicians suggest 25 mg as conventional tablets 2 or 3 times daily or 37.5 mg as extended-release tablets or capsules once daily. Maintenance dosages are 75–375 mg in divided doses for conventional tablets and 75–300 mg once daily for extended-release capsules or tablets.
Special Populations
Hepatic Impairment
Reduce total daily dose of venlafaxine by 50% in patients with mild to moderate hepatic impairment. Reduce total daily dose by >50% in patients with severe hepatic impairment or cirrhosis; it may be desirable to individualize dosages.
Maximum 112.5 mg daily of venlafaxine besylate extended-release tablets in patients with hepatic impairment; use another extended-release product if total daily dosage is <112.5 mg daily.
Renal Impairment
Reduce total daily dosage by 25–50% in patients with mild-to-moderate renal impairment and by ≥50% in patients with severe renal impairment or undergoing hemodialysis. Individualization of dosages may be desirable.
Maximum 112.5 mg daily of venlafaxine besylate extended-release tablets in patients with renal impairment; use another extended-release product if total daily dosage is <112.5 mg daily.
Geriatric Patients
Dosage adjustment not required; use caution when increasing and individualizing dosage.
Pharmacogenomic Considerations in Dosing
Clinical Pharmacogenetics Implementation Consortium (CPIC) guidelines provide dosing recommendations for venlafaxine based on CYP2D6 phenotypes. Initiate therapy with recommended starting dosage for patients identified as normal CYP2D6 metabolizers. For patients identified as ultrarapid or intermediate CYP2D6 metabolizers, no action is recommended because of minimal evidence regarding impact of genotype on efficacy or side effects for venlafaxine. For patients identified as poor metabolizers of CYP2D6, consider a clinically appropriate alternative antidepressant not predominately metabolized by CYP2D6. No recommendations for patients with indeterminate CYP2D6 phenotypes.
Cautions for Venlafaxine
Contraindications
-
Known hypersensitivity to venlafaxine besylate, venlafaxine hydrochloride, desvenlafaxine succinate, or to any excipients in the formulation.
-
Concurrent or recent (i.e., within 14 days) therapy with MAOIs, including linezolid and IV methylene blue.
Warnings/Precautions
Warnings
Suicidal Thoughts and Behaviors
Increased risk of suicidal thoughts and behavior in adolescent and young adult patients taking antidepressants. (See Boxed Warning.) Depression itself is a risk factor for suicidal thoughts and behaviors. Monitor all patients treated with antidepressants for any indication of clinical worsening or emergence of suicidal thoughts and behaviors, particularly during initiation of therapy (i.e., the first few months) and during periods of dosage adjustments. Counsel families and caregivers to monitor for changes in the patient’s behavior, and to report such symptoms to a clinician. Consider changing the therapeutic regimen or discontinuing venlafaxine in patients whose depression is persistently worse or in patients experiencing emergent suicidal thoughts or behaviors.
Other Warnings and Precautions
Serotonin Syndrome
Serotonergic antidepressants can precipitate serotonin syndrome; a potentially life-threatening condition. Increased risk with concurrent use of other serotonergic drugs (e.g., serotonin [5-hydroxytryptamine; 5-HT] type 1 receptor agonists [“triptans”], tricyclic antidepressants [TCAs], fentanyl, lithium, tramadol, tryptophan, buspirone, amphetamines, and St. John’s wort [Hypericum perforatum]) and with drugs that impair serotonin metabolism (i.e., MAO inhibitors [MAOIs]).
Symptoms may include mental status changes (e.g., agitation, hallucinations, delirium, coma), autonomic instability (e.g., tachycardia, labile blood pressure, dizziness, diaphoresis, flushing, hyperthermia), neuromuscular symptoms (e.g., tremor, rigidity, myoclonus, hyperreflexia, incoordination), seizures, and GI symptoms (e.g., nausea, vomiting, diarrhea).
Concurrent or recent (i.e., within 14 days) use of MAOIs is contraindicated. Do not initiate in patients treated with MAOIs such as linezolid or IV methylene blue. If MAOI is necessary, discontinue before initiating the MAOI.
Monitor patients for serotonin syndrome. If manifestations occur, immediately discontinue venlafaxine and any concurrently administered serotonergic agents; initiate supportive symptomatic treatment.
Elevated Blood Pressure
Increases in blood pressure, including sustained elevations, reported.
Control preexisting hypertension before initiating therapy and regularly monitor blood pressure during therapy. If sustained increases in blood pressure occur, consider venlafaxine dosage reduction or discontinuance.
Sexual Dysfunction
May cause sexual dysfunction, including ejaculatory delay or failure, decreased libido, or erectile dysfunction in males and decreased libido or delayed/absent orgasm in females. Obtain history and discuss potential management strategies with patients.
Discontinuation Syndrome
Possibly severe withdrawal reactions (e.g., agitation, anorexia, anxiety, confusion, impaired coordination, diarrhea, dizziness, dry mouth, dysphoric mood, fasciculation, fatigue, flu-like symptoms, headaches, hypomania, insomnia, nausea, nervousness, nightmares, sensory disturbances, somnolence, sweating, tremor, vertigo, vomiting, irritability, lethargy, emotional lability, tinnitus, and seizures); avoid abrupt discontinuance. Taper dosage gradually; monitor carefully for these symptoms and suicidal thoughts, aggression, and violent behavior.
If intolerable symptoms occur following dosage reduction or discontinuance, reinstitute previously prescribed dosage until symptoms abate, then resume more gradual dosage reductions.
Insomnia and Nervousness
May cause anxiety, nervousness, and insomnia.
Weight Changes
Weight loss reported in adults and pediatric patients.
Height Changes in Pediatric Patients
Height changes reported in pediatric patients. In clinical studies, pediatric patients treated with venlafaxine had height increases that were less than those treated with placebo or were less than expected based on data from age- and sex-matched peers.
Appetite Changes
Anorexia reported in adults and pediatric patients.
Activation of Mania and Hypomania
Activation of mania and hypomania reported with venlafaxine and other antidepressants.
Screen patients for any personal or family history of bipolar disorder, mania, or hypomania prior to starting treatment with venlafaxine.
Hyponatremia
Serotonergic antidepressants, including venlafaxine, may cause hyponatremia; in many cases, SIADH is apparent cause. Increased risk in geriatric patients, and in patients taking diuretics or who are otherwise volume depleted.
Discontinue venlafaxine and initiate appropriate medical intervention in patients with symptomatic hyponatremia; symptoms include headache, difficulty concentrating, memory impairment, confusion, weakness, and unsteadiness, which may lead to falls; more severe and/or acute cases have been associated with hallucinations, syncope, seizure, coma, and respiratory arrest.
Seizures
Seizures reported with use of venlafaxine; not systematically evaluated in patients with seizures. Use with caution in patients with a history of seizures. Discontinue therapy in any patient who develops seizures.
Increased Risk of Bleeding
Possible increased risk of bleeding. Concurrent administration of aspirin, NSAIAs, warfarin, and other anticoagulants may increase risk.
Inform patients about increased risk; for patients taking warfarin, carefully monitor coagulation indices.
Elevated Serum Cholesterol Concentrations
Clinically relevant increases in serum cholesterol concentrations reported. Consider monitoring serum cholesterol concentrations during long-term treatment.
Interstitial Lung Disease and Eosinophilic Pneumonia
Interstitial lung disease and eosinophilic pneumonia reported rarely; signs and symptoms may include progressive dyspnea, cough, or chest discomfort. Promptly evaluate patients with these symptoms and consider discontinuance of venlafaxine therapy.
Use in Patients with Concomitant Illness
Not systemically evaluated in patients with a recent history of myocardial infarction (MI) or other significant heart disease. Changes in electrocardiogram values and increases in heart rate reported in clinical trials. Use caution in patients with known cardiovascular or cerebrovascular disease that could be exacerbated by increases in heart rate (e.g., hyperthyroidism, heart failure, recent MI).
Interference with Cognitive and Motor Performance
No substantial impairment of psychomotor, cognitive, or complex behavior performance was found. However, since any psychoactive drug may impair judgment, thinking, or motor skills, inform patients about activities that require alertness (e.g., operating heavy machinery and motor vehicles), until they are reasonably certain that venlafaxine does not affect them adversely.
Angle-closure Glaucoma
May cause pupillary dilation (mydriasis), which can trigger an angle closure attack in patients without a patent iridectomy with anatomically narrow angles.
Specific Populations
Pregnancy
National Pregnancy Registry for Antidepressants available at 1-844-405-6185 or [Web].
Available epidemiologic data with venlafaxine in pregnant females have not established a drug-associated risk of major birth defects, miscarriage, or other adverse developmental outcomes.
Epidemiologic data found exposure to SNRIs (including venlafaxine), particularly in the month before delivery, is associated with a less than 2-fold increase in the risk of postpartum hemorrhage. Possible complications, sometimes severe and requiring prolonged hospitalization, respiratory support, enteral nutrition, and other forms of supportive care in neonates exposed to venlafaxine and other SNRIs or SSRIs late in the third trimester; may arise immediately upon delivery. Carefully consider the potential risks and benefits of treatment when used during the third trimester of pregnancy.
Neonates exposed to venlafaxine during the third trimester of pregnancy should be monitored for discontinuation syndrome.
Lactation
Distributed into milk; no adverse effects reported in breast-fed infants. Consider the developmental and health benefits of breastfeeding, the mother’s clinical need for the drug, and the potential for adverse effects on the breast-fed infant from exposure to venlafaxine or the underlying maternal condition.
Pediatric Use
Safety and effectiveness not established in pediatric patients; not approved for use in pediatric patients. Increased risk of suicidal thoughts and behaviors observed in pediatric patients treated with antidepressants. Possible decrease in height and weight in pediatric patients. Clinically important BP elevations observed in children and adolescents.
Geriatric Use
No substantial differences in safety and efficacy relative to younger adults, but increased sensitivity cannot be ruled out. May be at greater risk of hyponatremia.
Hepatic Impairment
Decreased clearance; dosage adjustment recommended.
Renal Impairment
Decreased clearance; dosage adjustment recommended.
Pharmacogenomic Considerations
No dosage adjustments necessary in patients known to be poor metabolizers of CYP2D6. CPIC guidelines recommend that a clinically appropriate alternative antidepressant be considered.
Common Adverse Effects
Venlafaxine hydrochloride conventional tablets (incidence ≥5%): asthenia, sweating, nausea, constipation, anorexia, vomiting, somnolence, dry mouth, dizziness, nervousness, anxiety, tremor and blurred vision, and abnormal ejaculation/orgasm and impotence in men.
Venlafaxine hydrochloride extended-release capsules (incidence ≥5%): sweating, nausea, anorexia, somnolence, dry mouth, constipation, abnormal ejaculation, impotence in men, and libido decreased. Safety of venlafaxine besylate extended-release tablets is based on the extended-release capsules.
Venlafaxine hydrochloride extended-release tablets for major depressive disorder (incidence ≥5%): sweating, GI complaints (nausea, dry mouth, anorexia), CNS complaints (dizziness, somnolence, abnormal dreams), and abnormal ejaculation.
Venlafaxine hydrochloride extended-release tablets for social anxiety disorder (incidence ≥5%): asthenia, sweating, GI complaints (anorexia, dry mouth, nausea), CNS complaints (anxiety, insomnia, libido decreased, nervousness, somnolence, dizziness), abnormalities of sexual function (abnormal ejaculation, orgasmic dysfunction, impotence), yawning, and abnormal vision.
Drug Interactions
Metabolized by CYP isoenzymes, principally by CYP2D6 to O-desmethylvenlafaxine (ODV), its major active metabolite. Also metabolized by CYP3A4. Weak inhibitor of CYP2D6.
Drugs Affecting Hepatic Microsomal Enzymes
CYP2D6 Inhibitors: Potential pharmacokinetic interaction (increased plasma venlafaxine concentrations). No dosage adjustment required.
CYP3A Inhibitors: Increased plasma concentrations of venlafaxine and ODV. Consider dose reduction of venlafaxine with concomitant use of CYP3A inhibitors.
Drugs Metabolized by Hepatic Microsomal Enzymes
Potential pharmacokinetic interaction (increased substrate plasma concentrations) with concomitant use of drugs that are metabolized by CYP2D6. Consider dosage reduction of the CYP2D6 substrate.
CNS-Active Drugs
Concomitant use not systematically evaluated; use caution.
Drugs Affecting Hemostasis
Increased risk of bleeding. Monitor for bleeding in patients receiving an antiplatelet or anticoagulant when venlafaxine is initiated or discontinued.
Serotonergic Drugs
Potential pharmacologic interaction (serotonin syndrome) with serotonergic medications. Monitor for serotonin syndrome with concomitant use, particularly during treatment initiation and dosage increases. If serotonin syndrome occurs, consider discontinuing venlafaxine and any concurrently administered serotonergic agents.
Protein-bound Drugs
Pharmacokinetic interaction unlikely; venlafaxine not highly bound to plasma proteins.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Alcohol |
No apparent additive cognitive or psychomotor effects; no effects on venlafaxine pharmacokinetics |
Avoid concomitant use |
|
Amphetamines |
Risk of serotonin syndrome |
Monitor for signs and symptoms of serotonin syndrome; consider discontinuation if symptoms occur |
|
Buspirone |
Risk of serotonin syndrome |
Monitor for signs and symptoms of serotonin syndrome; consider discontinuation if symptoms occur |
|
Cimetidine |
Increased venlafaxine plasma concentrations, but no effect on ODV |
No dosage adjustment required for most patients; use with caution in geriatric patients and patients with hypertension or hepatic impairment |
|
Clozapine |
Cases of elevated clozapine levels associated with adverse reactions, including seizures, reported |
|
|
Desipramine |
Increased plasma concentrations of desipramine and its metabolite |
|
|
Diazepam |
Pharmacokinetic interactions unlikely |
|
|
5-HT1 receptor agonists ("triptans") |
Risk of serotonin syndrome |
Monitor for signs and symptoms of serotonin syndrome; consider discontinuation if symptoms occur |
|
Haloperidol |
Increased haloperidol plasma concentrations |
|
|
Imipramine |
Pharmacokinetic interaction unlikely |
|
|
Ketoconazole |
Increased plasma concentrations of venlafaxine and ODV |
|
|
Laboratory tests |
False-positive urine immunoassay screening for phencyclidine (PCP) and amphetamine reported |
Use gas chromatography/mass spectrometry for confirmatory testing of PCP and amphetamine |
|
Lithium |
Pharmacokinetic interaction unlikely, but potentially additive serotonergic effects |
Monitor for signs and symptoms of serotonin syndrome; consider discontinuation if symptoms occur |
|
MAOIs (including linezolid and methylene blue) |
Potentially fatal serotonin syndrome |
Concomitant use contraindicated Allow at least 14 days to elapse between discontinuance of an MAOI and initiation of venlafaxine; allow at least 7 days to elapse between discontinuance of venlafaxine and initiation of an MAO inhibitor If an MAOI such as linezolid or IV methylene blue is necessary in a patient receiving venlafaxine, discontinue venlafaxine before initiating the MAOI |
|
Metoprolol |
Increased metoprolol plasma concentration |
|
|
Opioids |
Risk of serotonin syndrome |
Monitor for signs and symptoms of serotonin syndrome; consider discontinuation if symptoms occur |
|
Risperidone |
Increased risperidone plasma concentrations |
|
|
SNRIs or SSRIs |
Risk of serotonin syndrome |
Monitor for signs and symptoms of serotonin syndrome; consider discontinuation if symptoms occur |
|
St John's wort (Hypericum perforatum) |
Risk of serotonin syndrome |
Monitor for signs and symptoms of serotonin syndrome; consider discontinuation if symptoms occur |
|
TCAs |
Risk of serotonin syndrome |
Monitor for signs and symptoms of serotonin syndrome; consider discontinuation if symptoms occur |
|
Tryptophan |
Risk of serotonin syndrome |
Monitor for signs and symptoms of serotonin syndrome; consider discontinuation if symptoms occur |
|
Warfarin |
May increase INR |
Monitor INR during concomitant use |
|
Weight loss drugs (i.e., phentermine) |
Safety and efficacy of concomitant use not established ; venlafaxine not indicated for weight loss |
Concomitant use not recommended |
Venlafaxine Pharmacokinetics
Absorption
Bioavailability
Well absorbed following oral administration.
Absolute bioavailability is about 45%.
Peak plasma concentrations of conventional tablets achieved in 2 hours.
Peak plasma concentrations of venlafaxine hydrochloride extended-release formulations achieved in 5.5 hours.
Peak plasma concentrations of venlafaxine besylate extended-release tablets achieved in 5-18 hours.
Food
Venlafaxine hydrochloride formulations: Food does not affect GI absorption of venlafaxine or bioavailability of ODV, its major active metabolite.
Venlafaxine besylate formulations: High-fat meal increases mean peak plasma concentrations of venlafaxine and ODV.
Distribution
Extent
Distributed into human milk.
Plasma Protein Binding
Venlafaxine: Approximately 27%.
ODV: Approximately 30%.
Elimination
Metabolism
Extensively metabolized in the liver via CYP2D6 to O-desmethylvenlafaxine (ODV), its major active metabolite; also metabolized to N, O-didesmethylvenlafaxine and other minor metabolites. Minor metabolism by CYP3A4 to N-desmethylvenlafaxine, a minor, less active metabolite.
Elimination Route
Renal elimination of venlafaxine and its metabolites is the primary route of excretion (87%).
Half-life
Elimination half-lives of venlafaxine and ODV are approximately 5 and 11 hours, respectively.
Special Populations
In cirrhotic patients, elimination half-lives of venlafaxine and ODV are prolonged by about 30–60% and clearance decreased by about 30–50% compared with values in healthy subjects. Patients with more severe cirrhosis had a more substantial decrease in venlafaxine clearance (about 90%).
In patients with mild to moderate hepatic impairment (Child-Pugh Score A and Child-Pugh Score B, respectively), oral elimination half-life was approximately twice as long and oral clearance was reduced by more than half when compared with healthy subjects.
In renally impaired patients (GFR=10–70 mL/min), elimination half-lives of venlafaxine and ODV are prolonged by about 40–50% and venlafaxine clearance was reduced by about 24% compared with values in healthy subjects. In dialysis patients, venlafaxine and ODV elimination half-lives were prolonged by about 142–180% and clearance was reduced by about 56–57%.
In patients with the CYP2D6 poor metabolizer phenotype, metabolism of venlafaxine may be decreased, leading to increased serum levels of venlafaxine and decreased levels of its active metabolite ODV.
Stability
Storage
Oral
Tablets
Venlafaxine hydrochloride: 20–25°C. Keep dry.
Extended-release Tablets
Venlafaxine hydrochloride: 20–25°C (excursions permitted between 15–30°C). Protect from moisture and humidity.
Venlafaxine besylate: 20–25°C (excursions permitted between 15–30°C).
Extended-release Capsules
Venlafaxine hydrochloride: 20–25°C.
Actions
-
Mechanisms of antidepressant and anxiolytic actions are uncertain but appear to be associated with the potentiation of neurotransmitter activity in the CNS.
-
Venlafaxine and ODV are potent inhibitors of neuronal serotonin and norepinephrine reuptake and weak inhibitors of dopamine reuptake.
-
Possesses no significant affinity for muscarinic cholinergic, H1-histaminergic, or α1-adrenergic receptors.
Advice to Patients
-
Advise patients to read the FDA-approved patient labeling (medication guide).
-
Advise patients and caregivers to monitor for the emergence of suicidal thoughts and behaviors, especially during the first few months of therapy or during periods of dosage adjustment. Instruct patients and caregivers to report such symptoms to their clinician.
-
Advise patients not to take venlafaxine or any of its formulations with a MAOI or within 14 days of stopping an MAOI.
-
Inform patients of the risk of serotonin syndrome with concomitant use of venlafaxine and other serotonergic agents including SNRIs, SSRIs, triptans, TCAs, opioids, lithium, buspirone, amphetamines, tryptophan, and St. John’s wort (Hypericum perforatum). Stress importance of seeking immediate medical attention if symptoms of serotonin syndrome develop.
-
Advise patients to regularly monitor blood pressure while taking venlafaxine therapy as venlafaxine may cause elevated blood pressure.
-
Advise patients about the increased risk of bleeding with concomitant use of venlafaxine with NSAIAs, aspirin, other antiplatelet drugs, warfarin, or other anticoagulants.
-
Advise patients to exercise caution while operating hazardous machinery, including driving a motor vehicle, until they are reasonably certain that venlafaxine therapy does not adversely affect their ability to engage in such activities.
-
Advise patients to avoid alcohol consumption during venlafaxine therapy.
-
Advise patients and their caregivers to look for signs of activation of mania/hypomania.
-
Use venlafaxine with caution in patients with cardiovascular, cerebrovascular, or lipid metabolism disorders.
-
Inform patients that elevations in blood cholesterol levels, including total cholesterol, low-density lipoprotein (LDL) cholesterol, and triglycerides, may occur with venlafaxine therapy and advise patients to consider monitoring serum lipid levels.
-
Advise patients not to abruptly stop taking venlafaxine without first talking with their clinician. Inform patients that withdrawal symptoms may occur when suddenly stopping venlafaxine, and they should monitor for withdrawal symptoms.
-
Inform patients that venlafaxine can cause sexual dysfunction, and advise patients to discuss any changes and potential management strategies with their healthcare clinician.
-
Advise patients to notify their clinician if any sign or symptoms of an allergic reaction develop during venlafaxine therapy (e.g., rash, hives, swelling, difficulty breathing).
-
Advise patients that venlafaxine can cause mild pupillary dilation, which can lead to an episode of angle-closure glaucoma in susceptible individuals.
-
Advise patients that venlafaxine hydrochloride extended-release capsules contain spheroids, which release slowly into the digestive tract. Patients may notice spheroids passing in the stool or via colostomy due to elimination of the insoluble portion of these spheroids. Patients should be aware that the active medication has already been absorbed by the time the spheroids are seen.
-
Advise females to inform their clinicians if they are or plan to become pregnant or plan to breast-feed. Advise females that there is a pregnancy exposure registry that monitors pregnancy outcomes in females exposed to venlafaxine during pregnancy.
-
Advise patients that venlafaxine use during mid to late pregnancy may lead to an increased risk of preeclampsia and may increase the risk for neonatal complications requiring prolonged hospitalization, respiratory support, and tube feeding.
-
Advise patients to inform their clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary and herbal supplements, as well as any concomitant illnesses.
-
Advise patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
25 mg (of venlafaxine)* |
Venlafaxine Hydrochloride Tablets |
|
|
37.5 mg (of venlafaxine)* |
Venlafaxine Hydrochloride Tablets |
|||
|
50 mg (of venlafaxine)* |
Venlafaxine Hydrochloride Tablets |
|||
|
75 mg (of venlafaxine)* |
Venlafaxine Hydrochloride Tablets |
|||
|
100 mg (of venlafaxine)* |
Venlafaxine Hydrochloride Tablets |
|||
|
Tablets, extended-release |
37.5 mg (of venlafaxine)* |
Venlafaxine Hydrochloride Extended-release Tablets |
||
|
75 mg (of venlafaxine)* |
Venlafaxine Hydrochloride Extended-release Tablets |
|||
|
150 mg (of venlafaxine)* |
Venlafaxine Hydrochloride Extended-release Tablets |
|||
|
225 mg (of venlafaxine)* |
Venlafaxine Hydrochloride Extended-release Tablets |
|||
|
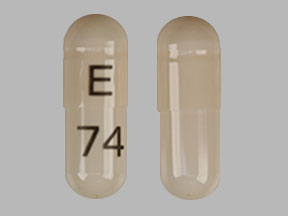
Capsules, extended-release |
37.5 mg (of venlafaxine)* |
Effexor XR |
Viatris |
|
|
Venlafaxine Hydrochloride Extended-release Capsules |
||||
|
75 mg (of venlafaxine)* |
Effexor XR |
Viatris |
||
|
Venlafaxine Hydrochloride Extended-release Capsules |
||||
|
150 mg (of venlafaxine)* |
Effexor XR |
Viatris |
||
|
Venlafaxine Hydrochloride Extended-release Capsules |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, extended-release |
112.5 mg (of venlafaxine) |
Venlafaxine Besylate Extended-release Tablets |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Frequently asked questions
- How long do venlafaxine withdrawal symptoms last?
- SSRIs vs SNRIs - What's the difference between them?
- What drugs can cause serotonin syndrome?
More about venlafaxine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (2,808)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: serotonin-norepinephrine reuptake inhibitors
- Breastfeeding
- En español