Topiramate (Monograph)
Brand names: Eprontia, Qudexy XR, Topamax, Trokendi XR
Drug class: Anticonvulsants, Miscellaneous
Introduction
Anticonvulsant and antimigraine agent; sulfamate-substituted derivative of d-fructose; differs structurally from other currently available anticonvulsant agents.
Uses for Topiramate
Seizure Disorders
Initial monotherapy of partial-onset seizures or primary generalized tonic-clonic seizures in adults and children ≥2 years of age (≥6 years of age for Trokendi XR only).
Adjunctive therapy (i.e., in combination with other anticonvulsants) of partial-onset seizures in adults and children ≥2 years of age (≥6 years of age for Trokendi XR only).
Adjunctive therapy (i.e., in combination with other anticonvulsants) of primary generalized tonic-clonic seizures in adults and children ≥2 years of age (≥6 years of age for Trokendi XR only).
Adjunctive therapy (i.e., in combination with other anticonvulsants) of seizures associated with Lennox-Gastaut syndrome in adults and children ≥2 years of age (≥6 years of age for Trokendi XR only).
Has been used as adjunctive therapy in the treatment of seizures associated with Dravet syndrome† [off-label]. Generally used as a second-line anticonvulsant option after clobazam† [off-label] and valproic acid† [off-label].
Guidelines generally include topiramate among treatment options for adult patients with new-onset focal or generalized epilepsy; however, topiramate has a lower level of recommendation for this indication compared to other therapies (e.g., carbamazepine) due to a lower level of evidence. Topiramate is recommended as monotherapy or adjunctive therapy for management of treatment-resistant epilepsy based on high-quality evidence. The place in therapy for topiramate in the treatment of pediatric epilepsy is not well-defined due to a lack of high-quality evidence.
Migraine Prophylaxis
Prevention of migraine headaches in adults and adolescents ≥12 years of age.
Topiramate is included in guidelines as one of several drugs with established efficacy for migraine prevention in adults. The existing evidence is not sufficient to support superiority of one agent over another; therefore, selection of an appropriate drug should be individualized based on drug efficacy, tolerability, cost, patient comorbidities, and other patient-specific factors. Combining preventive drugs from different classes may be useful when there is a suboptimal response or dose-limiting adverse effects of a particular agent.
Topiramate may also be considered for preventive treatment of migraines in pediatric patients with frequent headaches, disability related to migraine, or medication overuse; however, the evidence supporting topiramate use in this population is of lower quality.
Alcohol Dependence
Has been used in adults for management of alcohol dependence† [off-label].
One of several drugs suggested by the American Psychiatric Association for this use. However, additional studies needed to more clearly establish role.
Has been effective in the management of alcohol withdrawal† [off-label] in a limited number of patients in uncontrolled studies.
Antipsychotic-induced Weight Gain
Has been used for weight loss and prevention of weight gain from second-generation antipsychotics in patients with schizophrenia†.
Binge Eating Disorder
Has been used for the treatment of binge eating disorder†,
Essential Tremor
Has been used for the treatment of essential tremor†.
Topiramate Dosage and Administration
General
Pretreatment Screening
-
Measure serum bicarbonate prior to initiating treatment with topiramate.
Patient Monitoring
-
Closely monitor patients who are currently receiving or beginning therapy with topiramate and/or any other anticonvulsant for any indication for the emergence or worsening of depression, suicidal thoughts or behavior (suicidality), and/or any unusual changes in mood or behavior.
-
Monitor height and weight in pediatric patients receiving long-term treatment with topiramate.
-
Measure serum bicarbonate periodically during treatment with topiramate.
-
Closely monitor patients, particularly pediatric patients, for evidence of decreased sweating and increased body temperature, especially in hot weather.
-
Monitor for seizures/increased seizure frequency when rapid withdrawal of topiramate is medically required.
-
Monitor for signs of hyperammonemic encephalopathy in patients who develop unexplained lethargy, vomiting, or changes in mental status.
Dispensing and Administration Precautions
-
Because of similarity in spelling between Topamax (the trade name for topiramate) and Toprol-XL (a trade name for metoprolol succinate, a β-adrenergic blocking agent), the potential exists for dispensing or prescribing errors involving these drugs. These medication errors have been associated with serious adverse events sometimes requiring hospitalization as a result of either lack of the intended medication (e.g., seizure or hypertension recurrence) or exposure to the wrong drug (e.g., bradycardia in a patient erroneously receiving metoprolol). Therefore, extra care should be exercised to ensure the accuracy of both oral and written prescriptions for these drugs. Patients should be advised to carefully check their medications and to bring any questions or concerns to the attention of the dispensing pharmacist.
-
Dispensing errors involving Topamax (topiramate) and Toprol-XL (metoprolol succinate) should be reported to the manufacturers, the USP/ISMP (Institute for Safe Medication Practices) Medication Errors Reporting Program by phone (800-233-7767), or directly to the FDA MedWatch program by phone (800-FDA-1088), fax (800-FDA-0178), or internet ([Web]).
Administration
Oral Administration
Administer orally as immediate-release tablets, sprinkle capsules, extended-release capsules, or oral solution without regard to meals.
Sprinkle capsule formulation is bioequivalent to immediate-release tablet and may be substituted as a therapeutic equivalent. Extended-release capsule administered once daily is bioequivalent to immediate-release tablet administered twice daily.
Tablets
Tablets should be swallowed intact and not broken or chewed because of the bitter taste.
Sprinkle Capsules
Swallow capsules whole.
Alternatively, open capsule and sprinkle entire contents on soft food (e.g., applesauce, custard, ice cream, oatmeal, yogurt, pudding); swallow immediately without chewing.
Drinking fluids immediately after administration may help to ensure that all of the mixture is swallowed.
Do not store sprinkle/food mixture for use at a later time.
Extended-release Capsules
Qudexy XR: Swallow capsules whole or, alternatively, open capsule and sprinkle contents on a small amount of soft food; must swallow sprinkle/food mixture immediately without chewing, crushing, or storing for later use.
Trokendi XR: Must swallow capsules whole; do not open and sprinkle on food, crush, or chew; because of these limitations, Trokendi XR is not recommended for use in children <6 years of age.
Oral Solution
Measure the dose using a calibrated measuring device to ensure accuracy; do not measure the dose using a household tablespoon or teaspoon. Discard any unused portion within 30 days after opening.
Extemporaneously Compounded Oral Liquid
An extemporaneously compounded oral liquid formulation of topiramate has been prepared.
Standardize 4 Safety
Standardized concentrations for an extemporaneously prepared oral liquid preparation of topiramate has been established through Standardize 4 Safety (S4S), a national patient safety initiative to reduce medication errors, especially during transitions of care. Because recommendations from the S4S panels may differ from the manufacturer’s prescribing information, caution is advised when using concentrations that differ from labeling, particularly when using rate information from the label. For additional information on S4S (including updates that may be available), see [Web]
The topiramate concentration is copyright protected by USP and can be used for internal purposes only.
|
Concentration Standard |
|---|
|
20 mg/mL |
Dosage
Pediatric Patients
Seizure Disorders
Monotherapy of Partial-onset Seizures or Primary Generalized Tonic-Clonic Seizures
OralChildren 2–9 years of age (or 6–9 years of age if using Trokendi XR): Initially, 25 mg daily (administered nightly) for first week. Increase to 50 mg daily (administered in 2 divided doses as immediate-release tablets, or sprinkle capsules, or oral solution, or once daily as extended-release capsules) during second week if tolerated. Subsequently increase by 25–50 mg daily each week as tolerated. Attempt titration to minimum recommended maintenance dosage (see Table 1) over 5–7 weeks. May attempt additional increases (in increments of 25–50 mg daily at weekly intervals) up to maximum recommended dosage (see Table 1) based on tolerability and seizure control.
|
Weight (kg) |
Minimum Total Daily Dosage (mg/day) |
Maximum Total Daily Dosage (mg/day) |
|---|---|---|
|
Up to 11 |
150 |
250 |
|
12–22 |
200 |
300 |
|
23–31 |
200 |
350 |
|
32–38 |
250 |
350 |
|
>38 |
250 |
400 |
Children ≥10 years of age: Initially, 50 mg daily (administered in 2 divided doses as immediate-release tablets, sprinkle capsules, or oral solution, or once daily as extended-release capsules). Titrate up to recommended dosage of 400 mg daily as tolerated according to schedule in Table 2 or 3. In clinical studies, approximately 58% of patients achieved the maximum dosage of 400 mg daily.
|
Week |
Morning Dose |
Evening Dose |
|---|---|---|
|
1 |
25 mg |
25 mg |
|
2 |
50 mg |
50 mg |
|
3 |
75 mg |
75 mg |
|
4 |
100 mg |
100 mg |
|
5 |
150 mg |
150 mg |
|
6 |
200 mg |
200 mg |
|
Week |
Dosage |
|---|---|
|
1 |
50 mg once daily |
|
2 |
100 mg once daily |
|
3 |
150 mg once daily |
|
4 |
200 mg once daily |
|
5 |
300 mg once daily |
|
6 |
400 mg once daily |
Adjunctive Therapy of Partial-onset Seizures, Primary Generalized Tonic-Clonic Seizures, or Seizures Associated with Lennox-Gastaut Syndrome
OralChildren 2–16 years of age (or 6–16 years of age if using Trokendi XR): Initially, 25 mg (or less based on a range of 1–3 mg/kg daily) given nightly for the first week. Increase dosage at 1- or 2-week intervals in increments of 1–3 mg/kg daily (administered in 2 divided doses as immediate-release tablets, sprinkle capsules, or oral solution, or once daily as extended-release capsules) to achieve optimal clinical response.
Recommended maintenance dosage is approximately 5–9 mg/kg daily (administered in 2 divided doses as immediate-release tablets, sprinkle capsules, or oral solution, or once daily as extended-release capsules).
Alternatively, some clinicians recommend an initial dosage of 0.5–1 mg/kg daily, with slow titration (in increments of 1–3 mg/kg every other week or in increments of 0.5–1 mg/kg per week) to obtain optimal efficacy with minimal adverse effects.
Adjunctive Therapy of Seizures Associated with Dravet Syndrome†
OralInitial dosage usually 0.5 to 2 mg/kg daily (in divided doses), increasing to a target dosage of 5–12 mg/kg daily.
Migraine Prophylaxis
OralAdolescents ≥12 years of age: Recommended dosage is 100 mg daily (administered in 2 divided doses as immediate-release tablets, sprinkle capsules, or oral solution, or once daily as extended-release capsules). Titrate therapy using the schedule in Table 4 or 5.
|
Week |
Morning Dose |
Evening Dose |
|---|---|---|
|
1 |
None |
25 mg |
|
2 |
25 mg |
25 mg |
|
3 |
25 mg |
50 mg |
|
4 |
50 mg |
50 mg |
|
Week |
Dosage |
|---|---|
|
1 |
25 mg once daily |
|
2 |
50 mg once daily |
|
3 |
75 mg once daily |
|
4 |
100 mg once daily |
Titrate dosage based on clinical outcome. Use longer intervals between dose adjustments if required.
Adults
Seizure Disorders
Monotherapy of Partial-onset Seizures or Primary Generalized Tonic-Clonic Seizures
OralInitially, 50 mg daily (administered in 2 divided doses as immediate-release tablets, sprinkle capsules, or oral solution, or once daily as extended-release capsules). Titrate up to recommended dosage of 400 mg daily as tolerated according to schedule in Table 6 or 7, depending on the dosage form used. In clinical studies, approximately 58% of patients achieved the maximum dosage of 400 mg daily.
|
Week |
Morning Dose |
Evening Dose |
|---|---|---|
|
1 |
25 mg |
25 mg |
|
2 |
50 mg |
50 mg |
|
3 |
75 mg |
75 mg |
|
4 |
100 mg |
100 mg |
|
5 |
150 mg |
150 mg |
|
6 |
200 mg |
200 mg |
|
Week |
Dosage |
|---|---|
|
1 |
50 mg once daily |
|
2 |
100 mg once daily |
|
3 |
150 mg once daily |
|
4 |
200 mg once daily |
|
5 |
300 mg once daily |
|
6 |
400 mg once daily |
Adjunctive Therapy of Partial-onset Seizures
OralInitially, 25–50 mg daily. Increase dosage at weekly intervals in increments of 25–50 mg to achieve optimal clinical response.
Recommended maintenance dosage is 200–400 mg daily (administered in 2 divided doses as immediate-release tablets, sprinkle capsules, or oral solution, or once daily as extended-release capsules).
Limited data indicate that titration in increments of 25 mg/week is associated with a lower incidence of cognitive and psychiatric adverse effects and lower discontinuance rates but may delay the time to reach an effective dosage.
Dosages >400 mg daily have not been shown to improve response.
Adjunctive Therapy of Primary Generalized Tonic-Clonic Seizures
OralInitially, 25–50 mg daily. Increase dosage at weekly intervals in increments of 25–50 mg to achieve optimal clinical response.
Recommended maintenance dosage is 400 mg daily (administered in 2 divided doses as immediate-release tablets, sprinkle capsules, or oral solution, or once daily as extended-release capsules).
Limited data indicate that titration in increments of 25 mg/week is associated with a lower incidence of cognitive and psychiatric adverse effects and lower discontinuance rates but may delay the time to reach an effective dosage.
Adjunctive Therapy of Seizures Associated with Lennox-Gastaut Syndrome
OralInitially, 25–50 mg daily. Increase dosage at weekly intervals in increments of 25–50 mg to achieve optimal clinical response.
Recommended maintenance dosage is 200–400 mg daily (administered in 2 divided doses as immediate-release tablets, sprinkle capsules, or oral solution, or once daily as extended-release capsules).
Limited data indicate that titration in increments of 25 mg/week is associated with a lower incidence of cognitive and psychiatric adverse effects and lower discontinuance rates but may delay the time to reach an effective dosage.
Migraine Prophylaxis
Oral
Recommended dosage is 100 mg daily (administered in 2 divided doses as immediate-release tablets, sprinkle capsules, or oral solution, or once daily as extended-release capsules). Titrate therapy using the schedule in Table 8 or 9, depending on the dosage form used.
|
Week |
Morning Dose |
Evening Dose |
|---|---|---|
|
1 |
None |
25 mg |
|
2 |
25 mg |
25 mg |
|
3 |
25 mg |
50 mg |
|
4 |
50 mg |
50 mg |
|
Week |
Dosage |
|---|---|
|
1 |
25 mg once daily |
|
2 |
50 mg once daily |
|
3 |
75 mg once daily |
|
4 |
100 mg once daily |
Titrate dosage based on clinical outcome. Increase intervals between dose adjustments if required.
Alcohol Dependence†
Optimum dosage regimen not established; initial dosage of 25 mg daily followed by gradual titration to maintenance dosage of 200–300 mg daily found to be effective in clinical studies.
Clinical studies suggest that a more gradual titration (e.g., over 8 weeks) may be better tolerated than more rapid titration (e.g., over 6 weeks).
A period of abstinence from alcohol prior to initiating topiramate therapy does not appear to be necessary.
Prescribing Limits
Pediatric Patients
Monotherapy of Partial-onset Seizures or Primary Generalized Tonic-Clonic Seizures
Oral
Pediatric patients 2–9 years of age: Total daily dose should not exceed maximum recommended maintenance dosage for each range of body weight. (See Table 1.)
Adjunctive Therapy of Seizure Disorders
Oral
Pediatric patients 2–16 years of age: Total daily dose should not exceed 400 mg.
Special Populations
Hepatic Impairment
Clearance may be decreased; however, manufacturer makes no specific recommendations regarding dosage adjustment.
Renal Impairment
In patients with renal impairment (Clcr <70 mL/minute per 1.73 m2), decrease daily adult dosage by 50%.
Patients undergoing hemodialysis may require a supplemental dose following dialysis session; determine amount based on duration of dialysis, clearance rate of dialysis system, and the patient’s effective renal clearance of topiramate.
Geriatric Patients
The manufacturer makes no specific dosage recommendations for geriatric patients.
Cautions for Topiramate
Contraindications
-
Topiramate immediate-release tablets, sprinkle capsules, or oral solution: None.
-
Trokendi XR extended-release capsules: Patients with recent alcohol use (i.e., within 6 hours prior to or 6 hours after topiramate use).
-
Qudexy XR extended-release capsules: None.
Warnings/Precautions
Acute Myopia and Secondary Closure Glaucoma Syndrome
Acute myopia with secondary angle-closure glaucoma reported. Symptoms (e.g., acute onset of decreased visual acuity and/or ocular pain) typically occur within 1 month of initiating therapy. Discontinue treatment with topiramate as rapidly as possible based on clinical judgment if visual problems occur; additional supportive measures may be indicated.
Visual Field Defects
Visual field defects not associated with elevated intraocular pressure also reported.
If adverse ocular effects or visual problems occur, consider discontinuance of therapy. Manifestations generally resolve after drug is discontinued.
Oligohidrosis and Hyperthermia
Possible oligohidrosis and hyperthermia, particularly in pediatric patients; rarely may require hospitalization.
Monitor patients, particularly pediatric patients, closely for decreased sweating and increased body temperature, particularly in hot weather.
Consider risk of hyperthermia when used concomitantly with other drugs that predispose to heat-related disorders (e.g., carbonic anhydrase inhibitors, drugs with anticholinergic activity).
Metabolic Acidosis
Hyperchloremic, non-anion gap, metabolic acidosis reported. Manifestations may include hyperventilation, nonspecific symptoms (e.g., fatigue, anorexia), cardiac arrhythmias, or stupor. Can occur at any time during therapy.
Potential for serious sequelae (e.g., nephrolithiasis, nephrocalcinosis, osteomalacia and/or osteoporosis with increased risk for fractures, reduced growth rates in pediatric patients) from chronic, untreated metabolic acidosis.
Measure serum bicarbonate concentrations at baseline and periodically during therapy.
If metabolic acidosis develops and persists, consider reducing dosage or discontinuing therapy (by gradually tapering dose). If therapy is continued in patient with persistent acidosis, consider alkali treatment.
Interaction with Alcohol
Trokendi XR contraindicated in patients with recent alcohol use (i.e., within 6 hours prior to or 6 hours after topiramate use); marked elevations in plasma concentrations of Trokendi XR can occur in the presence of alcohol and concentrations may become subtherapeutic later in the day.
Suicidal Behavior and Ideation
Increased risk of suicidality (suicidal behavior or ideation) observed in an analysis of studies using various anticonvulsants in patients with epilepsy, psychiatric disorders (e.g., bipolar disorder, depression, anxiety), and other conditions (e.g., migraine, neuropathic pain); risk in patients receiving anticonvulsants (0.43%) was approximately twice that in patients receiving placebo (0.24%). Increased suicidality risk was observed ≥1 week after initiation of anticonvulsant therapy and continued through 24 weeks. Relative risk was higher for patients with epilepsy compared with those receiving anticonvulsants for other conditions.
Balance risk of suicidality with risk of untreated illness. Epilepsy and other illnesses treated with anticonvulsants are themselves associated with morbidity and mortality and an increased risk of suicidality. If suicidal thoughts or behavior emerges during anticonvulsant therapy, consider whether these symptoms may be related to the illness itself.
Cognitive/Neuropsychiatric Effects
Immediate-release formulations of topiramate have been associated with cognitive and neuropsychiatric adverse events; these effects are thus also expected with extended-release preparations. CNS-related adverse effects are common.
CNS effects are generally classified into 3 categories: cognitive-related dysfunction (confusion, psychomotor slowing, difficulty with concentration/attention, difficulty with memory, speech or language problems), psychiatric/behavioral disturbances (e.g., depression, mood problems), and somnolence and fatigue.
Risk is increased with rapid titration and higher initial dosages.
Fetal/Neonatal Morbidity and Mortality
May cause fetal harm. (See Pregnancy under Cautions.) In utero exposure to topiramate associated with increased risk of oral cleft birth defects (cleft lip and/or palate) and risk of neonates being small for gestational age.
Developmental toxicity, including teratogenicity and embryotoxicity, structural malformations, and maternal toxicity demonstrated in animals.
Inform all females of reproductive potential of the potential risks to the fetus from exposure to topiramate.
Withdrawal of Antiepileptic Drugs
Discontinue therapy gradually to minimize the potential for increased seizure frequency. Appropriate monitoring recommended if more rapid withdrawal required.
Decrease in Bone Mineral Density
Reductions in bone mineral density in the lumbar spine and total body less head reported among pediatric patients treated with topiramate. Potential impact on fracture risk cannot be determined due to trial limitations.
Negative Effects on Growth (Height and Weight)
Reductions in growth (height and weight) observed in pediatric patients treated with topiramate. Carefully monitor height and weight in pediatric patients receiving long-term treatment with topiramate.
Serious Skin Reactions
Serious skin reactions, including Stevens-Johnson syndrome and toxic epidermal necrolysis, have occurred. Discontinue therapy at first sign of drug-related rash; do not resume if symptoms of Stevens-Johnson syndrome or toxic epidermal necrolysis occur.
Hyperammonemia and Encephalopathy (without and with Concomitant Valproic Acid Use)
Dose-related hyperammonemia, with or without encephalopathy, reported. In some cases, ammonia concentrations were markedly increased in patients receiving a topiramate dosage of 100 mg daily.
During postmarketing experience, hyperammonemia with or without encephalopathy reported in patients receiving concomitant topiramate and valproic acid who previously tolerated either drug alone.
Patients with inborn errors of metabolism or reduced hepatic mitochondrial activity may be at increased risk.
Although patients may be asymptomatic, manifestations usually include acute alterations in level of consciousness and/or cognitive function with lethargy or vomiting. In most cases, manifestations abated following discontinuance of therapy.
If unexplained lethargy, vomiting, or changes in mental status occur, consider possibility of hyperammonemic encephalopathy and measure ammonia concentration.
Kidney Stones
Increased incidence of kidney stone formation in clinical trials in adults; incidence higher in men than women. Kidney stones also reported in pediatric patients.
Avoid use in patients receiving other drugs that produce metabolic acidosis and in those on a ketogenic diet.
Maintain adequate fluid intake to decrease stone formation.
Hypothermia with Concomitant Valproic Acid Use
Hypothermia, with or without hyperammonemia, reported in patients receiving concurrent topiramate and valproic acid therapy. Can occur after initiating topiramate therapy or following dosage increase. Manifestations may include lethargy, confusion, coma, or substantial alterations in other major organ systems (e.g., cardiovascular, respiratory).
If hypothermia occurs, consider discontinuance of topiramate or valproic acid. Since hypothermia also may be a manifestation of hyperammonemia, monitor plasma ammonia concentrations as part of clinical management.
Specific Populations
Pregnancy
Risk of fetal harm.
Carefully consider benefits versus risks in females of reproductive potential, particularly when topiramate is used for conditions not usually associated with permanent injury or death. If use is necessary in a female of reproductive potential, advise patient to use effective contraception; consider alternative therapies in patients who are planning a pregnancy.
Effect of topiramate-induced metabolic acidosis not specifically studied during pregnancy; however, metabolic acidosis during pregnancy is known to cause decreased fetal growth, decreased fetal oxygenation, and fetal death. Monitor pregnant patients for metabolic acidosis in the same manner as nonpregnant patients. In addition, monitor neonates since possible drug transfer and transient metabolic acidosis may occur following birth.
North American Antiepileptic Drug (NAAED) Pregnancy Registry at 888-233-2334 or [Web].
Lactation
Distributed into human milk at concentrations similar to those in maternal plasma. Effects of the drug on milk production not known. Diarrhea and somnolence reported in breast-fed infants whose mothers were receiving topiramate.
Consider known benefits of breast-feeding along with the woman’s clinical need for topiramate and any potential adverse effects on the breast-fed infant from the drug or underlying maternal condition.
Females and Males of Reproductive Potential
Inform all females of reproductive potential of the potential risks to the fetus from exposure to topiramate. Consider alternative options in patients who are planning a pregnancy. If topiramate is used in a female of reproductive potential who is not planning a pregnancy, recommend use of effective contraception. Consider the potential for decreased efficacy of estrogen-containing oral contraceptives.
Pediatric Use
Safety and efficacy for management of seizure disorders not established in children <2 years of age. Safety and efficacy for migraine prophylaxis not established in pediatric patients <12 years of age.
Although other preparations of topiramate may be used in children as young as 2 years of age for management of seizure disorders, use of Trokendi XR is recommended only in children ≥6 years of age because the capsule formulation must be swallowed whole and cannot be sprinkled on food, crushed, or chewed.
Hyperchloremic, non-anion gap, metabolic acidosis reported.
Metabolic acidosis in patients <2 years of age (not an FDA-labeled population) notably greater in magnitude than that observed in older children and adults. Potential for serious sequelae (e.g., osteomalacia [rickets], reduced growth rates, decrease in maximal height achieved) resulting from chronic, untreated metabolic acidosis.
Measure serum bicarbonate concentrations at baseline and periodically during therapy. Reductions in bone mineral density and growth reported in pediatric patients treated with topiramate.
Incidence of adverse CNS effects appears to be lower in children than adults.
Oligohidrosis and hyperthermia typically reported in children.
Geriatric Use
Insufficient experience in patients ≥65 years of age to determine whether geriatric patients respond differently than younger patients.
Clearance may be decreased in patients with reduced renal function. Monitor renal function.
Dosage adjustment may be necessary in geriatric patients with impaired renal function.
Hepatic Impairment
Clearance may be decreased.
Renal Impairment
Clearance decreased; dosage adjustment recommended in patients with moderate or severe renal impairment.
Common Adverse Effects
Adults and pediatric patients in seizure studies (≥10%): Paresthesia, anorexia, weight loss, speech disorders or other related speech problems, fatigue, dizziness, somnolence, nervousness, psychomotor slowing, abnormal vision, fever.
Adults and adolescents in migraine studies (≥5%): Paresthesia, anorexia, weight loss, difficulty with memory, taste perversion, diarrhea, hypoesthesia, nausea, abdominal pain, upper respiratory tract infection.
Adults receiving dosages ≤300 mg daily for alcohol dependence†: Paresthesia, taste perversion, fatigue, anorexia, insomnia, concentration and attention difficulties, memory impairment, nervousness, somnolence, diarrhea, dizziness, pruritus.
Drug Interactions
Mild inhibitor of CYP2C19 and mild inducer of CYP3A4.
Does not inhibit CYP1A2, 2A6, 2B6, 2C9, 2D6, 2E1, or 3A4/5.
Drugs Metabolized by Hepatic Microsomal Enzymes
Pharmacokinetic interactions with drugs metabolized by CYP2C19 or CYP3A4 are possible.
Drugs Predisposing to Heat-related Disorders
Potential pharmacologic interaction (increased risk of hyperthermia) with drugs that predispose to heat-related disorders; use with caution.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Alcohol |
Potential for additive CNS effects Trokendi XR extended-release capsules: In vitro data indicate that topiramate plasma concentrations may be markedly increased soon after dosing and become subtherapeutic later in the day |
Use caution Use of Trokendi XR contraindicated in patients with recent alcohol use (i.e., within 6 hours prior to or 6 hours after topiramate use) |
|
Amitriptyline |
Increased plasma amitriptyline concentrations |
Adjust amitriptyline dosage based on clinical response |
|
Anticholinergic agents |
Possible increased risk of hyperthermia |
|
|
Carbamazepine |
Clinically important decreases in plasma concentrations of topiramate observed; plasma concentrations of carbamazepine or its active metabolite not substantially altered |
Dosage adjustment may be required |
|
Carbonic anhydrase inhibitors (e.g., acetazolamide, dichlorphenamide, zonisamide) |
Possible increased risk or severity of metabolic acidosis and kidney stone formation; possible increased risk of hyperthermia |
Monitor for onset or worsening of metabolic acidosis |
|
CNS depressants |
Potential for enhanced CNS depression |
Use with extreme caution |
|
Digoxin |
Possible decrease in serum digoxin concentrations |
Clinical importance unknown |
|
Dihydroergotamine |
Pharmacokinetic interaction unlikely |
|
|
Diltiazem |
Possible decreased plasma diltiazem concentrations and increased topiramate concentrations |
|
|
Glyburide |
Possible decrease in plasma glyburide concentrations |
|
|
Haloperidol |
No effect on pharmacokinetics of haloperidol |
|
|
Hydrochlorothiazide |
Possible increased plasma topiramate concentrations; pharmacokinetics of hydrochlorothiazide not substantially altered Enhanced risk of hypokalemia |
Although clinical importance of this interaction not known, topiramate dosage adjustment may be necessary when hydrochlorothiazide is initiated |
|
Lamotrigine |
Decreased plasma topiramate concentrations; lamotrigine concentrations not likely to be affected by concurrent administration of up to 400 mg daily of topiramate |
|
|
Lithium |
Possible increased exposure to lithium with concurrent administration of high-dose (up to 600 mg daily) topiramate |
Monitor serum lithium concentrations in patients receiving concurrent lithium and high-dose topiramate therapy |
|
Metformin |
Possible increase in plasma metformin concentrations; possible decrease in topiramate clearance |
Clinical importance of these pharmacokinetic effects unknown; however, topiramate can cause metabolic acidosis, a condition for which the use of metformin is contraindicated |
|
Oral contraceptives |
Substantial decrease in ethinyl estradiol exposure reported in patients receiving an oral contraceptive containing ethinyl estradiol and norethindrone in conjunction with topiramate and valproic acid |
Consider possibility of decreased oral contraceptive efficacy and breakthrough bleeding |
|
Phenobarbital |
<10% change in plasma concentrations of phenobarbital |
|
|
Phenytoin |
Clinically important decreases in plasma topiramate concentrations observed; possible increase in serum phenytoin concentrations (generally in those receiving twice-daily phenytoin regimen) |
Dosage adjustment may be required |
|
Pioglitazone |
Decreased systemic exposure to active metabolites of pioglitazone; however, clinical importance not known |
When topiramate therapy is initiated in patients receiving pioglitazone or vice versa, monitor blood glucose control carefully |
|
Primidone |
<10% change in plasma concentrations of primidone |
|
|
Propranolol |
Pharmacokinetic interaction unlikely |
|
|
Risperidone |
Decreased plasma risperidone concentrations; increased plasma topiramate concentrations No clinically important changes observed |
|
|
Sumatriptan |
No effect on pharmacokinetics of sumatriptan |
|
|
Valproic acid |
Possible decrease in plasma concentrations of valproic acid and topiramate Concomitant use associated with hyperammonemia with or without encephalopathy; also associated with hypothermia (with or without hyperammonemia) |
Consider discontinuance of topiramate or valproic acid if hypothermia occurs |
|
Venlafaxine |
Pharmacokinetics of venlafaxine or topiramate not affected |
|
|
Warfarin |
Decreased INR and PT observed with concomitant use |
Topiramate Pharmacokinetics
Absorption
Bioavailability
Rapidly absorbed following oral administration; peak plasma concentrations achieved in about 2 hours (following administration of tablets or sprinkle capsules), 30 minutes (following administration of the oral solution) or 20–24 hours (following administration of extended-release formulations).
Sprinkle capsule formulation is bioequivalent to immediate-release tablet. At steady state, extended-release capsules administered once daily are bioequivalent to immediate-release tablets administered twice daily.
Food
Food may affect time to peak concentrations (depending on formulation), but does not appear to affect systemic exposure.
Distribution
Extent
Appears to cross the placenta.
Distributes into breast milk.
Plasma Protein Binding
Approximately 15–41%. Fraction bound decreases with increasing plasma topiramate concentrations.
Elimination
Metabolism
Not extensively metabolized. Six minor metabolites identified; none constitutes more than 5% of administered dose.
Elimination Route
Eliminated principally in urine as unchanged drug (approximately 70%).
Half-life
Immediate-release tablets, sprinkle capsules, oral solution: Approximately 21 hours.
Extended-release capsules (Trokendi XR): Approximately 31 hours.
Extended-release capsules (Qudexy XR): Approximately 56 hours.
Special Populations
In pediatric patients, clearance is 50% higher, resulting in a shorter elimination half-life and lower plasma concentrations, relative to adults.
In geriatric patients with reduced renal function (Clcr reduced by 20% compared with younger adults), clearance was decreased.
In patients with hepatic impairment, clearance may be decreased; mechanism not fully understood.
In patients with moderate or severe renal impairment, clearance is reduced by 42 or 54%, respectively. In patients undergoing hemodialysis, clearance is 4–6 times more rapid than in healthy individuals.
Stability
Storage
Oral
Extended-release Capsules
Qudexy XR: Tight containers at 20–25°C (excursions permitted to 15–30°C). Protect from moisture.
Trokendi XR: Tight containers at 25°C (excursions permitted to 15–30°C). Protect from moisture and light.
Sprinkle Capsules
Tight containers at ≤25°C. Protect from moisture.
Tablets
Tight containers at 15–30°C. Protect from moisture.
Oral Solution
20–25°C (excursions permitted to 15–30°C). Discard unused portion 30 days after first opening.
Actions
-
Mechanism of action is unknown; however, properties that may contribute to anticonvulsant and antimigraine activities, including blocking sodium channels, enhancing the inhibitory action of GABA by acting at some subtypes of GABA-A receptor, antagonizing AMPA/kainate subtype of glutamate receptor, and inhibiting carbonic anhydrase enzymes have been demonstrated in electrophysiologic and biochemical studies.
-
Precise mechanism of action in alcohol dependence† unknown; however, properties that may result in suppression of mesocorticolimbic dopaminergic activity include potentiation of GABA-mediated inhibitory neurotransmission and inhibition of glutamate-mediated neuroexcitation.
Advice to Patients
-
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
-
Counsel patients to swallow Qudexy XR capsules whole or carefully open and sprinkle the entire contents on a spoonful of soft food. This drug/food mixture should be swallowed immediately and not chewed. Do not store drug/food mixture for future use. Counsel patients to swallow Trokendi XR capsules whole and intact. Trokendi XR should not be sprinkled on food, chewed or crushed.
-
Counsel patients that Eprontia may be taken with or without food. Advise patients that the dosage of Eprontia should be measured using a calibrated measuring device and not a household teaspoon and that an oral dosing syringe may be obtained from their pharmacist. Instruct patients to discard any unused Eprontia 30 days after first opening the bottle.
-
Advise patients to completely avoid consumption of alcohol at least 6 hours prior to and 6 hours after taking Trokendi XR.
-
Instruct patients taking topiramate to seek immediate medical attention if they experience blurred vision, visual disturbances, or periorbital pain.
-
Closely monitor patients treated with topiramate, especially pediatric patients, for evidence of decreased sweating and increased body temperature, especially in hot weather. Counsel patients to contact their healthcare professionals immediately if they develop a high or persistent fever, or decreased sweating.
-
Warn patients about the potential significant risk for metabolic acidosis that may be asymptomatic and may be associated with adverse effects on kidneys (e.g., kidney stones, nephrocalcinosis), bones (e.g., osteoporosis, osteomalacia, and/or rickets in children), and growth (e.g., growth delay/retardation) in pediatric patients, and on the fetus.
-
Counsel patients, their caregivers, and families that antiepileptic drugs, including topiramate, may increase the risk of suicidal thoughts and behavior, and advise of the need to be alert for the emergence or worsening of the signs and symptoms of depression, any unusual changes in mood or behavior or the emergence of suicidal thoughts, or behavior or thoughts about self-harm. Instruct patients to immediately report behaviors of concern to their healthcare providers.
-
Warn patients about the potential for somnolence, dizziness, confusion, difficulty concentrating, or visual effects, and advise patients not to drive or operate machinery until they have gained sufficient experience on topiramate to gauge whether it adversely affects their mental performance, motor performance, and/or vision.
-
Even when taking topiramate or other anticonvulsants, some patients with epilepsy will continue to have unpredictable seizures. Therefore, advise all patients taking topiramate for epilepsy to exercise appropriate caution when engaging in any activities where loss of consciousness could result in serious danger to themselves or those around them (including swimming, driving a car, climbing in high places, etc.). Some patients with refractory epilepsy will need to avoid such activities altogether. Discuss the appropriate level of caution with patients, before patients with epilepsy engage in such activities.
-
Inform pregnant patients and females of reproductive potential that use of topiramate during pregnancy can cause fetal harm, including an increased risk for cleft lip and/or cleft palate (oral clefts), which occur early in pregnancy before many people know they are pregnant. Also inform patients that infants exposed to topiramate monotherapy in utero may be small for gestational age. There may also be risks to the fetus from chronic metabolic acidosis with use of topiramate during pregnancy. When appropriate, counsel pregnant patients and females of reproductive potential about alternative therapeutic options.
-
Advise females of reproductive potential who are not planning a pregnancy to use effective contraception while using topiramate, keeping in mind that there is a potential for decreased contraceptive efficacy when using estrogen-containing birth control with topiramate.
-
Encourage pregnant patients using topiramate to enroll in the North American Antiepileptic Drug (NAAED) Pregnancy Registry. The registry is collecting information about the safety of antiepileptic drugs during pregnancy.
-
Inform the patient or caregiver that long-term treatment with topiramate can decrease bone formation and increase bone resorption in children.
-
Discuss with the patient or caregiver that long-term topiramate treatment may attenuate growth as reflected by slower height increase and weight gain in pediatric patients.
-
Inform patients about the signs of serious skin reactions. Instruct patients to immediately inform their healthcare provider at the first appearance of skin rash.
-
Warn patients about the possible development of hyperammonemia with or without encephalopathy. Although hyperammonemia may be asymptomatic, clinical symptoms of hyperammonemic encephalopathy often include acute alterations in level of consciousness and/or cognitive function with lethargy and/or vomiting. This hyperammonemia and encephalopathy can develop with topiramate treatment alone or with topiramate treatment with concomitant valproic acid. Instruct patients to contact their physician if they develop unexplained lethargy, vomiting, or changes in mental status.
-
Instruct patients, particularly those with predisposing factors, to maintain an adequate fluid intake in order to minimize the risk of kidney stone formation.
-
Counsel patients taking extended-release forms of topiramate that these formulations can cause a reduction in body temperature, which can lead to alterations in mental status. If they note such changes, they should call their health care professional and measure their body temperature. Patients taking concomitant valproic acid should be specifically counseled on this potential adverse reaction.
-
Instruct patients that if they miss a single dose of immediate-release topiramate, it should be taken as soon as possible. However, if a patient is within 6 hours of taking the next scheduled dose, tell the patient to wait until then to take the usual dose of topiramate and to skip the missed dose. Tell patients that they should not take a double dose in the event of a missed dose. Advise patients to contact their healthcare provider if they have missed more than one dose.
-
Advise female patients to inform their clinician if they are or plan to become pregnant or plan to breast-feed.
-
Advise patients to inform their clinician of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary and herbal supplements, as well as any concomitant illnesses.
-
Advise patients of other important precautionary information. (See Cautions.)
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
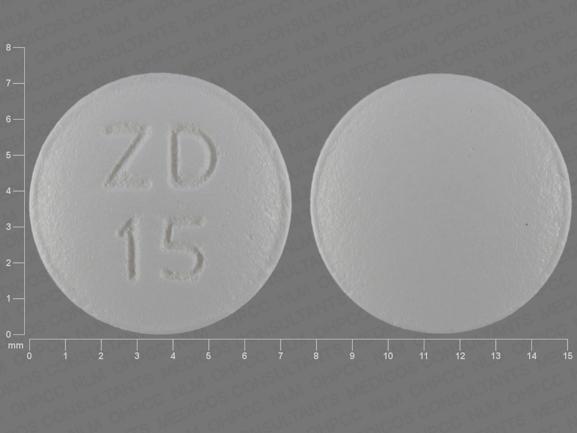
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules (containing coated particles) |
15 mg* |
Topamax Sprinkle Capsules |
Janssen |
|
Topiramate Sprinkle Capsules |
||||
|
25 mg* |
Topamax Sprinkle Capsules |
Janssen |
||
|
Topiramate Sprinkle Capsules |
||||
|
Capsules, extended-release |
25 mg* |
Qudexy XR |
Upsher-Smith |
|
|
Topiramate Extended-release Capsules |
||||
|
Trokendi XR |
Supernus |
|||
|
50 mg* |
Qudexy XR |
Upsher-Smith |
||
|
Topiramate Extended-release Capsules |
||||
|
Trokendi XR |
Supernus |
|||
|
100 mg* |
Qudexy XR |
Upsher-Smith |
||
|
Topiramate Extended-release Capsules |
||||
|
Trokendi XR |
Supernus |
|||
|
150 mg* |
Qudexy XR |
Upsher-Smith |
||
|
Topiramate Extended-release Capsules |
||||
|
200 mg* |
Qudexy XR |
Upsher-Smith |
||
|
Topiramate Extended-release Capsules |
||||
|
Trokendi XR |
Supernus |
|||
|
Solution |
25 mg/mL |
Eprontia |
Azurity |
|
|
Tablets, film-coated |
25 mg* |
Topamax |
Janssen |
|
|
Topiramate Tablets |
||||
|
50 mg* |
Topamax |
Janssen |
||
|
Topiramate Tablets |
||||
|
100 mg* |
Topamax |
Janssen |
||
|
Topiramate Tablets |
||||
|
200 mg* |
Topamax |
Janssen |
||
|
Topiramate Tablets |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Frequently asked questions
- How effective is Topamax (topiramate) for weight loss?
- Does Topamax (topiramate) cause hair loss?
- Best time to take Topamax (topiramate): morning or night?
- Can you drink alcohol while taking Topamax (topiramate)?
- Topamax for migraines: how long should you take it?
- How long does it take for Topamax to start working?
- How long does Topamax stay in your system?
- Is Topamax (topiramate) a controlled substance?
- Are Topamax and Trokendi XR the same thing?
More about topiramate
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (1,343)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: carbonic anhydrase inhibitor anticonvulsants
- Breastfeeding
Patient resources
Professional resources
- Topiramate prescribing information
- Topiramate Capsules (FDA)
- Topiramate ER Capsules (FDA)
- Topiramate Oral Solution (FDA)
- Topiramate Tablets (FDA)
Other brands
Topamax, Trokendi XR, Eprontia, Qudexy XR