Indapamide
Drug class: Thiazide-like Diuretics
VA class: CV701
Chemical name: 3-(Aminosulfonyl)-4-chloro-N-(2,3-dihydro-2-methyl-1H-indol-1-yl)benzamide
Molecular formula: C16H16ClN3O3S
CAS number: 26807-65-8
Introduction
An indoline diuretic and antihypertensive agent; pharmacologically similar to thiazide diuretics.
Uses for Indapamide
Hypertension
Used alone or in combination with other antihypertensive agents for all stages of hypertension.
Classified as a thiazide-like drug with regard to management of hypertension; the drug’s efficacy in hypertensive patients is similar to that of the thiazide diuretics.
Thiazide-type diuretics are recommended as one of several preferred agents for the initial management of hypertension according to current evidence-based hypertension guidelines; other preferred options include ACE inhibitors, angiotensin II receptor antagonists, and calcium-channel blockers. While there may be individual differences with respect to recommendations for initial drug selection and use in specific patient populations, current evidence indicates that these antihypertensive drug classes all generally produce comparable effects on overall mortality and cardiovascular, cerebrovascular, and renal outcomes.
Individualize choice of therapy; consider patient characteristics (e.g., age, ethnicity/race, comorbidities, cardiovascular risk) as well as drug-related factors (e.g., ease of administration, availability, adverse effects, cost).
A 2017 ACC/AHA multidisciplinary hypertension guideline classifies BP in adults into 4 categories: normal, elevated, stage 1 hypertension, and stage 2 hypertension. (See Table 1.)
Source: Whelton PK, Carey RM, Aronow WS et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13-115.
Individuals with SBP and DBP in 2 different categories (e.g., elevated SBP and normal DBP) should be designated as being in the higher BP category (i.e., elevated BP).
|
Category |
SBP (mm Hg) |
DBP (mm Hg) |
|
|---|---|---|---|
|
Normal |
<120 |
and |
<80 |
|
Elevated |
120–129 |
and |
<80 |
|
Hypertension, Stage 1 |
130–139 |
or |
80–89 |
|
Hypertension, Stage 2 |
≥140 |
or |
≥90 |
The goal of hypertension management and prevention is to achieve and maintain optimal control of BP. However, the BP thresholds used to define hypertension, the optimum BP threshold at which to initiate antihypertensive drug therapy, and the ideal target BP values remain controversial.
The 2017 ACC/AHA hypertension guideline generally recommends a target BP goal (i.e., BPs to achieve with drug therapy and/or nonpharmacologic intervention) <130/80 mm Hg in all adults regardless of comorbidities or level of atherosclerotic cardiovascular disease (ASCVD) risk. In addition, an SBP goal of <130 mm Hg generally is recommended for noninstitutionalized ambulatory patients ≥65 years of age with an average SBP of ≥130 mm Hg. These BP goals are based upon clinical studies demonstrating continuing reduction of cardiovascular risk at progressively lower levels of SBP.
Previous hypertension guidelines generally have based target BP goals on age and comorbidities. Guidelines such as those issued by the JNC 8 expert panel generally have targeted a BP goal of <140/90 mm Hg regardless of cardiovascular risk and have used higher BP thresholds and target BPs in elderly patients compared with those recommended by the 2017 ACC/AHA hypertension guideline.
Some clinicians continue to support previous target BPs recommended by JNC 8 due to concerns about the lack of generalizability of data from some clinical trials (e.g., SPRINT study) used to support the current ACC/AHA hypertension guideline and potential harms (e.g., adverse drug effects, costs of therapy) versus benefits of BP lowering in patients at lower risk of cardiovascular disease.
Consider potential benefits of hypertension management and drug cost, adverse effects, and risks associated with the use of multiple antihypertensive drugs when deciding a patient's BP treatment goal.
For decisions regarding when to initiate drug therapy (BP threshold), the current ACC/AHA hypertension guideline incorporates underlying cardiovascular risk factors. ASCVD risk assessment recommended by ACC/AHA for all adults with hypertension.
ACC/AHA currently recommend initiation of antihypertensive drug therapy in addition to lifestyle/behavioral modifications at an SBP ≥140 mm Hg or DBP ≥90 mm Hg in adults who have no history of cardiovascular disease (i.e., primary prevention) and a low ASCVD risk (10-year risk <10%).
For secondary prevention in adults with known cardiovascular disease or for primary prevention in those at higher risk for ASCVD (10-year risk ≥10%), ACC/AHA recommend initiation of antihypertensive drug therapy at an average SBP ≥130 mm Hg or an average DBP ≥80 mm Hg.
Adults with hypertension and diabetes mellitus, chronic kidney disease (CKD), or age ≥65 years of age are assumed to be at high risk for cardiovascular disease; ACC/AHA state that such patients should have antihypertensive drug therapy initiated at a BP ≥130/80 mm Hg. Individualize drug therapy in patients with hypertension and underlying cardiovascular or other risk factors.
In stage 1 hypertension, experts state that it is reasonable to initiate drug therapy using the stepped-care approach in which one drug is initiated and titrated and other drugs are added sequentially to achieve the target BP. Initiation of antihypertensive therapy with 2 first-line agents from different pharmacologic classes recommended in adults with stage 2 hypertension and average BP >20/10 mm Hg above BP goal.
Black hypertensive patients generally tend to respond better to monotherapy with thiazide diuretics or calcium-channel blockers than to other antihypertensive drug classes (e.g., ACE inhibitors, angiotensin II receptor antagonists). However, the combination of an ACE inhibitor or an angiotensin II receptor antagonist with a calcium-channel blocker or thiazide diuretic produces similar BP lowering in black patients as in other racial groups.
Thiazide-like diuretics may be preferred in hypertensive patients with osteoporosis. Secondary beneficial effect in hypertensive geriatric patients of reducing the risk of osteoporosis secondary to effect on calcium homeostasis and bone mineralization.
Edema in Heart Failure
Management of edema and salt retention associated with heart failure.
Most experts state that all patients with symptomatic heart failure who have evidence for, or a history of, fluid retention generally should receive diuretic therapy in conjunction with moderate sodium restriction, an agent to inhibit the renin-angiotensin-aldosterone (RAA) system (e.g., ACE inhibitor, angiotensin II receptor antagonist, angiotensin receptor-neprilysin inhibitor [ARNI]), a β-adrenergic blocking agent (β-blocker), and in selected patients, an aldosterone antagonist.
Diuretics produce rapid symptomatic benefits, relieving pulmonary and peripheral edema more rapidly (within hours or days) than cardiac glycosides, ACE inhibitors, or β-blockers (in weeks or months).
Loop diuretics (e.g., bumetanide, ethacrynic acid, furosemide, torsemide) are diuretics of choice for most patients with heart failure.
Edema in Pregnancy
Diuretics should not be used for routine therapy in pregnant women with mild edema who are otherwise healthy.
Use of thiazide-like diuretics may be appropriate in the management of edema of pathologic origin during pregnancy when clearly needed; routine use of diuretics in otherwise healthy pregnant women is irrational.
Use of diuretics for the management of edema of physiologic and mechanical origin during pregnancy generally is not warranted.
Dependent edema secondary to restriction of venous return by the expanded uterus should be managed by elevating the lower extremities and/or by wearing support hose; use of diuretics in these pregnant women is inappropriate.
In rare cases when the hypervolemia associated with normal pregnancy results in edema that produces extreme discomfort, a short course of diuretic therapy may provide relief and may be considered when other methods (e.g., decreased sodium intake, increased recumbency) are ineffective.
Diuretics will not prevent the development of toxemia, nor is there evidence that diuretics have a beneficial effect on the overall course of established toxemia.
Edema (General)
Management of edema resulting from various causes†.
No substantial difference in clinical effects or toxicity of comparable thiazide or thiazide-like diuretics, except metolazone may be more effective in edema with renal impairment.
Indapamide Dosage and Administration
General
Monitoring and BP Treatment Goals
-
Monitor BP regularly (i.e., monthly) during therapy and adjust dosage of the antihypertensive drug until BP controlled.
-
If unacceptable adverse effects occur, discontinue drug and initiate another antihypertensive agent from a different pharmacologic class.
-
Assess patient's renal function and electrolytes 2–4 weeks after initiation of diuretic therapy. (See Fluid and Electrolyte Imbalance under Cautions.)
-
If adequate BP response not achieved with a single antihypertensive agent, either increase dosage of single drug or add a second drug with demonstrated benefit and preferably a complementary mechanism of action (e.g., ACE inhibitor, angiotensin II receptor antagonist, calcium-channel blocker). Many patients will require at least 2 drugs from different pharmacologic classes to achieve BP goal; if goal BP still not achieved, add a third drug.
Administration
Administer orally as a single daily dose in the morning.
Dosage
Individualize dosage according to individual requirements and response.
For the management of fluid retention (e.g., edema) associated with heart failure, experts state that diuretics should be administered at a dosage sufficient to achieve optimal volume status and relieve congestion without inducing an excessively rapid reduction in intravascular volume, which could result in hypotension, renal dysfunction, or both.
Adults
Hypertension
Usual Dosage
OralManufacturer recommends initial dosage of 1.25 mg once daily in the morning; if response is inadequate, dosage may be increased at 4-week intervals to 2.5 mg daily and subsequently to 5 mg daily.
Some experts state that usual dosage range is 1.25–2.5 mg once daily.
Dosages >5 mg daily do not appear to result in further improvement in BP and increase the risk of hypokalemia. (See Hypokalemia under Cautions.)
If concomitant therapy with other antihypertensive agents is required, the usual dose of the other agent may need to be reduced initially by up to 50%; subsequent dosage adjustments should be based on BP response. Dosage reduction of both drugs may be required.
Edema in Heart Failure
Oral
Initially, 2.5 mg once daily in the morning.
If response is inadequate after 1 week, dosage may be increased to 5 mg daily given as a single dose in the morning.
Dosages >5 mg daily do not appear to result in further improvement in heart failure and increase the risk of hypokalemia. (See Hypokalemia under Cautions.)
Edema (General)
Oral
Similar dosages to those employed for the management of edema associated with heart failure have been used in the management of edema from other causes†.
Prescribing Limits
Adults
Oral
Dosages >5 mg daily do not appear to result in further improvement in heart failure or BP and are associated with increased risk of hypokalemia; clinical experience with such dosages is limited.
Special Populations
Hepatic Impairment
No specific dosage recommendations. (See Hepatic Impairment under Cautions.)
Renal Impairment
No specific dosage recommendations. (See Renal Impairment under Cautions.)
Geriatric Patients
No specific dosage recommendations. (See Geriatric Use under Cautions.)
Cautions for Indapamide
Contraindications
-
Anuria.
-
Known hypersensitivity to indapamide or other sulfonamide derivatives.
Warnings/Precautions
Warnings
Hyponatremia
Severe hyponatremia (serum sodium concentration <120 mEq/L), accompanied by hypokalemia, occurs rarely. Do not administer sodium chloride unless the hyponatremia is life threatening or actual sodium depletion is documented. If sodium chloride is administered, initially only correct to a state of mild hyponatremia; avoid early overcorrection to normonatremia or hypernatremia (risk of central pontine myelinolysis).
Risk of hyponatremia appears to be dose related; risk is greater in patients receiving a daily dosage of 2.5 or 5 mg.
Possible dilutional hyponatremia; occurs most commonly in patients with edema. Usually asymptomatic and managed by fluid intake restriction (e.g., 500 mL/day) and withdrawal of the diuretic.
Hypokalemia
Hypokalemia occurs commonly. Increased risk of hypokalemia, especially with brisk diuresis; large dosages (i.e., ≥5 mg daily); inadequate oral electrolyte intake; in presence of severe cirrhosis, hyperaldosteronism, or potassium-losing renal diseases; or during concomitant use of corticosteroids or ACTH.
Risk of hypochloremic alkalosis associated with hypokalemia, especially in patients with renal or liver disease; usually mild. Specific therapy generally not required.
Supplemental potassium chloride (including potassium-containing salt substitutes) may be necessary to prevent or treat hypokalemia and/or metabolic alkalosis.
Lithium
Generally, do not use with lithium salts. (See Specific Drugs under Interactions.)
Sensitivity Reactions
Dermatologic Reactions
Rash (e.g., erythematous, maculopapular, morbilliform), urticaria, pruritus, and vasculitis reported. In some cases, rash was accompanied by fever and/or dysuria. Rash generally resolves within 2 weeks after drug discontinuance, usually without specific therapy. May be treated with antihistamines.
Erythema multiforme and epidermal necrolysis reported rarely.
General Precautions
Fluid and Electrolyte Imbalance
Risk of electrolyte disturbances (e.g., hyponatremia, hypokalemia, hypochloremic alkalosis, hypomagnesemia). (See Hyponatremia and also Hypokalemia under Cautions.)
Periodic determinations of serum electrolyte concentrations (particularly potassium, sodium, chloride, and bicarbonate) should be performed and are especially important in patients at increased risk from hypokalemia (e.g., geriatric patients, those with cardiac arrhythmias, receiving concomitant cardiac glycosides, and/or with a history of ventricular arrhythmias), and those with diabetes mellitus, vomiting, diarrhea, parenteral fluid therapy, or expectations of other electrolyte imbalance (e.g., heart failure, renal disease, cirrhosis, restricted sodium intake, advanced age).
Observe carefully for manifestations of fluid and electrolyte depletion (e.g., dryness of mouth, thirst, weakness, fatigue, lethargy, drowsiness, restlessness, muscle pains or cramps, muscular fatigue, hypotension, oliguria, tachycardia, arrhythmia, GI disturbance). Measures to maintain normal serum concentrations should be instituted if necessary.
Hyperuricemia
Risk of hyperuricemia, especially in patients with a history of gout, family predisposition to gout, or chronic renal failure. Usually asymptomatic and rarely leads to clinical gout.
Generally avoid or use with caution in hypertensive patients with a history of gout unless patient is receiving uric acid lowering therapy.
Monitor serum uric acid concentrations periodically. Hyperuricemia and gout may be treated with a uricosuric agent.
Endocrine Effects
Risk of increased blood glucose, hyperglycemia, glycosuria, and impaired glucose tolerance; precipitation of diabetes mellitus rarely reported in patients with a history of impaired glucose tolerance (latent diabetes).
Monitor blood glucose concentrations periodically, especially in patients with known or suspected (e.g., marginally impaired glucose tolerance) diabetes mellitus.
Hypercalcemia
May decrease calcium urinary excretion; slight intermittent serum calcium increases reported; clinically important changes in serum total or ionic calcium concentrations have not been reported.
Use with caution in patients with hyperparathyroidism or thyroid disorders. Discontinue prior to performing parathyroid tests.
Lupus Erythematosus
Possible exacerbation or activation of systemic lupus erythematosus.
Sympathectomy
Antihypertensive effect may be enhanced after sympathectomy.
Fetal/Neonatal Morbidity
Diuretics cross the placental barrier and appear in cord blood. Use with caution; possibility of fetal or neonatal jaundice, thrombocytopenia, and other adverse effects reported in adults.
Specific Populations
Pregnancy
Category B.
Diuretics are considered second-line agents for control of chronic hypertension in pregnant women; if initiation of antihypertensive therapy is necessary during pregnancy, other antihypertensives (i.e., methyldopa, nifedipine, labetalol) are preferred.
Diuretics are not recommended for prevention or management of gestational hypertension or preeclampsia.
Lactation
Not known whether distributed into human milk. Manufacturer states to discontinue nursing or the drug; however, considered to be compatible with breast-feeding.
Pediatric Use
Safety and efficacy not established.
Geriatric Use
Use with caution in geriatric patients, especially females who are underweight; increased risk of dilutional hyponatremia. (See Hyponatremia under Cautions.)
Increased risk of hypokalemia; close monitoring recommended. (See Hypokalemia under Cautions.)
Hepatic Impairment
Use with caution in hepatic impairment or progressive liver disease (particularly with associated potassium deficiency); electrolyte and fluid imbalance may precipitate hepatic coma.
Increased risk of hypochloremic alkalosis associated with hypokalemia.
Renal Impairment
Use with caution in patients with severe renal disease; reduced plasma volume may exacerbate or precipitate azotemia.
Increased risk of hypochloremic alkalosis associated with hypokalemia.
Risk of hyperuricemia in patients with chronic renal failure.
Diuretic effect declines with decreasing renal function.
Evaluate renal function (e.g., BUN, Scr) periodically.
Consider interruption or discontinuance if progressive renal impairment (rising nonprotein nitrogen, BUN, or Scr) occurs.
Common Adverse Effects
Hypokalemia, headache, dizziness, fatigue, weakness, lethargy, tiredness, malaise, muscle cramps or spasm, numbness of the extremities, nervousness, tension, anxiety, irritability, agitation.
Interactions for Indapamide
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Antihypertensive agents |
Additive hypotensive effect; possible potentiation of postural hypotension |
Usually used to therapeutic advantage If concomitant therapy with other antihypertensive agents is required, dose of the other agent may need to be reduced initially by up to 50%; subsequent dosage adjustments should be based on BP response; dosage reduction of both drugs may be required Monitor for possible postural hypotension |
|
Digitalis glycosides |
Possible electrolyte disturbances (e.g., hypokalemia, hypomagnesemia) may predispose to digitalis toxicity; possibly fatal cardiac arrhythmias |
Monitor electrolytes; correct hypokalemia |
|
Diuretics, potassium-sparing (e.g., amiloride, triamterene) |
Concomitant therapy not fully evaluated |
Safety and efficacy of concurrent use for the prevention of hypokalemia have not been fully determined |
|
Insulin |
Possible precipitation of diabetes mellitus and altered insulin requirements (see Endocrine Effects under Cautions) |
Monitor blood glucose concentrations periodically, especially in patients with known or suspected (e.g., marginally impaired glucose tolerance) diabetes mellitus |
|
Lithium |
Reduced renal clearance of lithium and increased risk of lithium toxicity |
Concomitant use generally contraindicated If concomitant therapy is necessary, monitor serum lithium concentrations and reduce lithium dosage by about 50% |
|
Potassium-depleting drugs (e.g., corticosteroids, corticotropin, amphotericin B) |
Additive hypokalemic effects |
Monitor electrolytes; correct hypokalemia |
|
Vasopressors (e.g., norepinephrine, phenylephrine) |
Possible decrease in arterial responsiveness to vasopressors |
Unlikely to be clinically important |
Indapamide Pharmacokinetics
Absorption
Bioavailability
Rapidly and completely absorbed following oral administration, with peak plasma concentration usually attained within 2–2.5 hours.
Food
Food or antacids do not appear to affect absorption.
Distribution
Extent
Lipophilic; widely distributed into most tissues.
Not known whether indapamide crosses the placenta or is distributed into milk.
Preferentially and reversibly distributes into erythrocytes; whole blood/plasma ratio is about 6 during peak concentration and about 3.5 eight hours after administration.
Competitively and reversibly binds to carbonic anhydrase in erythrocytes, but does not appreciably inhibit the enzyme.
Plasma Protein Binding
Approximately 71–79%.
Elimination
Metabolism
Extensively metabolized in the liver, principally to glucuronide and sulfate conjugates.
Elimination Route
Excreted in urine (70%) mainly as metabolites and in feces (16–23%), probably including biliary elimination.
Half-life
Biphasic; terminal half-life is approximately 14–26 hours.
Special Populations
Half-life is not prolonged in patients with impaired renal function.
Not removed from circulation by hemodialysis.
Stability
Storage
Oral
Tablets
Tight, light-resistant containers at 20–25°C; avoid excessive heat.
Actions
-
A sulfonamide diuretic; pharmacologically and structurally related to thiazide diuretics.
-
Enhances excretion of sodium, chloride, and water by interfering with the transport of sodium ions across the renal tubular epithelium.
-
Exact tubular mechanism(s) of action is not known; principal site of action appears to be the cortical diluting segment of the distal convoluted tubules of the nephron.
-
Appears to indirectly increase potassium excretion by increasing the sodium load at the distal renal tubular site of sodium-potassium exchange.
-
Increases proximal calcium reabsorption and does not inhibit distal calcium reabsorption in the renal tubules.
-
Decreases free water clearance during hydration but not during dehydration.
-
Decreases urinary uric acid excretion.
-
No substantial effect on GFR or renal blood flow.
-
May increase plasma renin activity and urinary aldosterone secretion.
-
Hypotensive activity in hypertensive patients; also augments the action of other hypotensive agents.
-
Precise mechanism of hypotensive action has not been determined, but postulated that diuretics lower BP mainly by reducing plasma and extracellular fluid volume and by decreasing peripheral vascular resistance possibly secondary to sodium depletion and/or vascular autoregulatory feedback mechanisms; however, part of the hypotensive effect of indapamide may be caused by direct arteriolar dilation.
-
Reduces total peripheral resistance.
-
Usually no effect on cardiac output or left ventricular function in hypertensive patients.
Advice to Patients
-
Importance of informing patients of the signs and symptoms of electrolyte imbalance and instructing them to contact their clinician if dryness of mouth, thirst, weakness, lethargy, drowsiness, restlessness, oliguria, hypotension, tachycardia, GI disturbance, or muscle pains or cramps occur.
-
Importance of informing patients with diabetes mellitus that blood glucose and urine glucose concentrations may increase.
-
Advise hypertensive patients of importance of continuing lifestyle/behavioral modifications that include weight reduction (for those who are overweight or obese), dietary changes to include foods that are rich in potassium and calcium and moderately restricted in sodium (adoption of the Dietary Approaches to Stop Hypertension [DASH] eating plan), increased physical activity, smoking cessation, and moderation of alcohol intake.
-
Advise that lifestyle/behavioral modifications reduce BP, enhance antihypertensive drug efficacy, and decrease cardiovascular risk and remain an indispensable part of the management of hypertension.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
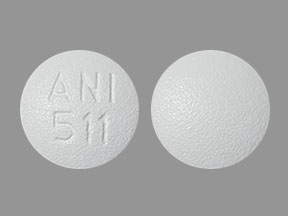
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
1.25 mg* |
Indapamide Tablets |
|
|
2.5 mg* |
Indapamide Tablets |
AHFS DI Essentials™. © Copyright 2022, Selected Revisions January 14, 2019. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Lasix
Lasix is a loop diuretic used to treat fluid retention from heart, liver, or kidney conditions, and ...
Dupixent
Dupixent is used to treat eczema, eosinophilic or oral-corticosteroid-dependent asthma, chronic ...
Aldactone
Aldactone (spironolactone) is used to diagnose or treat a condition in which you have too much ...
Triamterene
Triamterene (Dyrenium) is used to treat fluid retention in people with congestive heart failure ...
Acetazolamide
Acetazolamide is used for edema, epilepsy, glaucoma, hydrocephalus, hypokalemic periodic paralysis ...
Bumetanide
Bumetanide is used for ascites, autism, edema, pulmonary edema
Torsemide
Torsemide is used for ascites, edema, heart failure, high blood pressure, nonobstructive oliguria ...
Spironolactone
Spironolactone is a potassium-sparing diuretic that is primarily used to treat heart failure, high ...
More about indapamide
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (29)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: thiazide diuretics
- Breastfeeding
- En español