Fingolimod Hydrochloride (Sytemic) (Monograph)
Brand names: Gilenya, Tascenso ODT
Drug class: Sphingosine 1-Phosphate (S1P) Agents
Introduction
Sphingosine 1-phosphate (S1P) receptor modulator with immunomodulatory and disease-modifying activity in multiple sclerosis (MS).
Uses for Fingolimod Hydrochloride (Sytemic)
Multiple Sclerosis
Treatment of relapsing forms of MS, including clinically isolated syndrome, relapsing-remitting disease, and active secondary progressive disease in adults and pediatric patients (≥10 years of age).
Fingolimod is one of several disease-modifying therapies used in the management of relapsing forms of MS. Although not curative, these therapies have all been shown to modify several measures of disease activity, including relapse rates, new or enhancing MRI lesions, and disability progression.
The American Academy of Neurology (AAN) recommends that disease-modifying therapy be offered to patients with relapsing forms of MS who have had recent relapses and/or MRI activity. Clinicians should consider adverse effects, tolerability, method of administration, safety, efficacy, and cost of the drugs in addition to patient preferences when selecting an appropriate therapy.
Has been evaluated, but currently not FDA-labeled for treatment of primary-progressive MS (PPMS)† [off-label]. Did not slow disease progression in a randomized controlled study in patients with PPMS.
Autoimmune Neuropathy
Has been used for treatment of chronic inflammatory demyelinating polyneuropathy† [off-label].
Fingolimod Hydrochloride (Sytemic) Dosage and Administration
General
Pretreatment Screening
-
Evaluate cardiac function in patients with certain preexisting conditions (e.g., ischemic heart disease, history of myocardial infarction, congestive heart failure, history of cardiac arrest, cerebrovascular disease, uncontrolled hypertension, history of symptomatic bradycardia, history of recurrent syncope, severe untreated sleep apnea, atrioventricular (AV) block, sinoatrial heart block). Determine whether patient is taking any drugs that can slow heart rate or AV conduction.
-
Obtain recent (i.e., ≤6 months or after discontinuance of previous therapy) complete blood count (CBC).
-
Do not initiate therapy in patients with active acute or chronic infections until resolution of the infection.
-
Obtain recent (i.e., within the previous 6 months) transaminase and total bilirubin levels.
-
Assess current or prior medications. Consider possible additive immunosuppressive effects in patients receiving or who previously received antineoplastic, immunosuppressive, or immunomodulating therapies.
-
Test patients for antibodies to varicella zoster virus (VZV); VZV vaccination in antibody-negative patients is recommended. Consider vaccination against human papilloma virus (HPV). Cancer screening, including Papanicolaou (Pap) test, is also recommended per standard of care for patients receiving immunosuppressive therapies. Complete all age-appropriate vaccinations for pediatric patients.
-
Verify pregnancy status in females of reproductive potential.
-
Conduct an ophthalmologic examination of the fundus, including the macula, at baseline.
-
Conduct a baseline skin examination.
Patient Monitoring
-
First-dose 6-hour monitoring is recommended for all patients whenever therapy is initiated or reinitiated (after discontinuance for more than 14 days), or when dosage is increased (in pediatric patients).
-
Monitor patients for signs and symptoms of infection during and for 2 months after discontinuing therapy.
-
Monitor transaminase and total bilirubin levels periodically until 2 months after stopping fingolimod.
-
Conduct an ophthalmologic examination 3–4 months after initiation of therapy, periodically while on therapy, and any time there is a change in vision.
-
Evaluate respiratory function with spirometry and diffusion lung capacity for carbon monoxide (DLCO) determinations during fingolimod therapy if clinically indicated.
Dispensing and Administration Precautions
-
Fingolimod is a hazardous drug; follow procedures for proper handling (e.g., use of gloves) when handling the intact capsule.
Administration
Oral Administration
Administer orally once daily without regard to food.
Take fingolimod orally disintegrating tablets immediately after opening the blister pack; do not store orally disintegrating tablet outside blister pack for future use.
First-dose Monitoring
Initiation of fingolimod therapy decreases heart rate and may cause transient AV conduction delays. First-dose monitoring is recommended whenever therapy is initiated or reinitiated (after discontinuance for more than 14 days), or when dosage is increased (in pediatric patients).
Administer first dose in a setting with available resources to appropriately manage symptomatic bradycardia.
Observe all patients for signs and symptoms of bradycardia for at least 6 hours after first dose with hourly pulse and BP measurements. Obtain ECG prior to dosing and at the end of the observation period.
Institute additional observation until the finding has resolved in the following situations: heart rate 6 hours post-dose is <45 bpm (in adults), <55 bpm (in pediatric patients ≥12 years of age), or <60 bpm (in pediatric patients 10–11 years of age); heart rate 6 hours post-dose is at the lowest value suggesting that the maximum pharmacodynamic effect on the heart may not have occurred; or ECG 6 hours post-dose shows new-onset second-degree or higher AV block. Monitor patients who are at their lowest post-dose heart rate at the end of the observation period until heart rate increases.
If post-dose symptomatic bradycardia occurs, initiate appropriate management, begin continuous ECG monitoring, and continue observation until symptoms resolve. If pharmacologic intervention is required to treat bradycardia, monitor patient overnight with continuous ECG monitoring in a medical facility; repeat first-dose monitoring procedures for the second dose.
First-dose Monitoring in Higher-risk Patients
Patients at higher risk of symptomatic bradycardia or heart block because of a preexisting condition (e.g., ischemic heart disease, history of MI, CHF, history of cardiac arrest, cerebrovascular disease, uncontrolled hypertension, history of symptomatic bradycardia, history of recurrent syncope, severe untreated sleep apnea, AV or SA block): Perform cardiac evaluation by an appropriately trained clinician prior to initiating fingolimod. If decision is made to initiate therapy, institute overnight monitoring with continuous ECG in a medical facility.
Patients with a prolonged corrected QT (QTc) interval (>450 msec in adult and pediatric males; >470 msec in adult females; or >460 msec in pediatric females) before dosing or during the 6-hour observation period: Institute overnight monitoring with continuous ECG in a medical facility.
Patients at additional risk for QT-interval prolongation (e.g., those with hypokalemia, hypomagnesemia, or congenital long QT syndrome): Institute overnight monitoring with continuous ECG in a medical facility.
Patients receiving concurrent therapy with QT-prolonging drugs with a known risk of torsades de pointes: Institute overnight monitoring with continuous ECG in a medical facility.
Patients receiving concurrent therapy with drugs that slow heart rate or AV conduction: Observe patient overnight with continuous ECG monitoring after the first dose of fingolimod.
Reinitiation of Therapy Following Discontinuance
If fingolimod is discontinued for >14 days after the first month of treatment, effects on heart rate and AV conduction may recur upon reintroduction of drug; apply the same precautions (i.e., first-dose monitoring) as for initial dosing.
Within the first 2 weeks of treatment, first-dose monitoring procedures are recommended after treatment interruption of ≥1 day. During weeks 3 and 4 of treatment, first-dose monitoring procedures are recommended after treatment interruption of >7 days.
Washout Period Following Discontinuance of Other MS Therapies
Use caution when switching from drugs with prolonged immune effects (e.g., natalizumab, mitoxantrone, teriflunomide) to fingolimod.
Dosage
Available as fingolimod hydrochloride; dosage expressed in terms of fingolimod.
Pediatric Patients
Multiple Sclerosis
Oral
Children ≥10 years of age weighing >40 kg: 0.5 mg once daily.
Children ≥10 years of age weighing ≤40 kg: 0.25 mg once daily.
Dosages >0.5 mg daily associated with a greater incidence of adverse reactions without additional benefit.
Adults
Multiple Sclerosis
Oral
0.5 mg once daily. Dosages >0.5 mg daily associated with a greater incidence of adverse reactions without additional benefit.
Special Populations
Hepatic Impairment
Severe hepatic impairment: Monitor closely. Routine dosage adjustment does not appear necessary.
Mild or moderate hepatic impairment: Routine dosage adjustment not necessary.
Renal Impairment
Routine dosage adjustment does not appear necessary.
Geriatric Patients
Dosage adjustment not necessary.
Cautions for Fingolimod Hydrochloride (Sytemic)
Contraindications
-
Recent (in the past 6 months) myocardial infarction (MI), unstable angina, stroke, transient ischemic attack (TIA), decompensated heart failure requiring hospitalization, or class III or IV heart failure.
-
History or presence of Mobitz type II second-degree or third-degree atrioventricular (AV) block or sick sinus syndrome unless patient has a functioning pacemaker.
-
Baseline QTc interval ≥500 msec.
-
Cardiac arrhythmia requiring concomitant use of class Ia or class III antiarrhythmic agents.
-
History of hypersensitivity reaction to fingolimod or any ingredient in the formulation.
-
Concomitant use with other products containing fingolimod.
Warnings/Precautions
Bradyarrhythmia and AV Block
Risk of fingolimod-associated bradyarrhythmia and AV block; monitor patients during initiation of therapy.
After the first dose, heart rate decrease starts within an hour; maximal decline on the first day generally occurs within 6 hours and recovery (although not to baseline levels) occurs by 8–10 hours post-dose. A second period of heart rate decrease occurs within 24 hours after the first dose and may be more pronounced in some patients. Heart rates <40 bpm in adults and <50 bpm in pediatric patients observed rarely.
Patients with bradycardia generally are asymptomatic; however, some experience hypotension, dizziness, fatigue, palpitations, and chest pain, which usually resolve within first 24 hours of therapy.
Following the second dose, a further decrease in heart rate may occur but usually is of a smaller magnitude than that observed after the first dose. With continued dosing, the heart rate returns to baseline within one month. Continue to be alert to patient reports of cardiac symptoms throughout this period.
Transient AV conduction delays (e.g., first-degree or second-degree AV block) may occur when initiating therapy. Conduction abnormalities usually are transient, asymptomatic, and resolve within the first 24 hours of therapy, but occasionally require treatment with atropine or isoproterenol.
During postmarketing surveillance, third-degree AV block and AV block with junctional escape observed during the first-dose, 6-hour observation period. Isolated delayed-onset events, including transient asystole and unexplained death, occurred within 24 hours of the first dose. These events were confounded by concomitant medications and/or preexisting disease; causal relationship to fingolimod is uncertain. Syncope also reported after the first dose.
Infectious Complications
Fingolimod causes a dose-dependent reduction in peripheral lymphocyte count to 20–30% of baseline values. May increase risk of infections; some may be serious, life-threatening, or fatal.
Serious, sometimes fatal herpetic infections (including disseminated primary herpes zoster, herpes simplex encephalitis, and varicella zoster) reported, sometimes with multiorgan failure. In the reported deaths, patients had received higher fingolimod dosages than recommended also received high-dose corticosteroid therapy. Include disseminated herpetic infections in the differential diagnosis of patients who present with an atypical MS relapse or multiorgan failure.
Cases of Kaposi's sarcoma reported during postmarketing experience; promptly evaluate and manage patients with manifestations consistent with Kaposi's sarcoma.
Cryptococcal infections, including some cases of cryptococcal meningitis and disseminated cryptococcal infections, reported. If signs and symptoms consistent with cryptococcal meningitis occur, prompt diagnostic evaluation and treatment necessary.
Human papilloma virus (HPV) infections, including papilloma, dysplasia, warts, and HPV-related cancer, reported.
Before initiating treatment, a recent CBC (i.e., within 6 months or after discontinuance of previous therapy) should be available. Do not begin treatment in patients with active acute or chronic infections until infection(s) has resolved.
Monitor patients for signs and symptoms of infection during and for 2 months after discontinuing therapy. If a serious infection develops, consider drug discontinuance, at least temporarily, and reassess benefits and risks prior to reinitiation of therapy.
Has not been administered concomitantly with antineoplastic, non-corticosteroid immunosuppressive, or immunomodulating therapies used for MS. Concomitant use of these therapies, and also corticosteroid therapy, expected to increase risk of immunosuppression. When switching to fingolimod from immunomodulating or immunosuppressive therapies, consider duration and mechanism of action of the drugs to avoid unintentional additive immunosuppressive effects.
Test patients without a healthcare professional-confirmed history of chickenpox or without documentation of a full course of vaccination against varicella zoster virus (VZV) for antibodies to VZV before initiating fingolimod. VZV vaccination of antibody-negative patients is recommended prior to initiating fingolimod treatment; postpone initiation of fingolimod therapy for 1 month following vaccination. Vaccination against HPV should also be considered prior to initiating fingolimod. Cancer screening, including a Papanicolaou (Pap) test, is recommended.
Progressive Multifocal Leukoencephalopathy (PML)
PML, an opportunistic infection of the brain caused by the JC virus, reported.
At the first sign or symptom suggestive of PML, withhold fingolimod therapy and perform an appropriate diagnostic evaluation. Typical symptoms include progressive weakness on one side of the body, clumsiness of limbs, vision disturbance, changes in thinking, memory, or orientation leading to confusion, and personality changes that have progressed over days to weeks. MRI signs of PML may be apparent before clinical manifestations develop. If PML confirmed, discontinue fingolimod therapy.
Immune reconstitution inflammatory syndrome (IRIS) reported in patients treated with fingolimod who developed PML and subsequently discontinued treatment. Time to onset of IRIS in patients with PML is generally within a few months after fingolimod discontinuation. Monitor patients for IRIS development and appropriately treat the associated inflammation.
Macular Edema
Fingolimod increases the risk of macular edema; appears to be dose dependent, and may occur with or without symptoms (e.g., blurred vision, decreased visual acuity). Generally improves or resolves after drug discontinuance with or without treatment, but residual visual acuity loss has occurred in some patients.
Perform an ophthalmologic evaluation of the fundus, including the macula, at baseline, 3–4 months after treatment initiation, periodically while on therapy, and any time there is a change in vision. Continuation of fingolimod therapy in patients with macular edema not evaluated; weigh risks and benefits when determining whether to discontinue therapy. Risk of recurrence after rechallenge not evaluated.
Increased risk of macular edema in patients with diabetes mellitus or a history of uveitis.
Liver Injury
Clinically significant liver injury reported, including acute liver failure requiring liver transplant. Signs of liver injury (e.g., increased serum hepatic enzymes and elevated total bilirubin concentrations) occurred as early as 10 days after first dose but also reported after prolonged use. Most elevations occurred within 6–9 months and returned to normal within approximately 2 months after discontinuance of therapy. Transaminase elevations recurred upon rechallenge in some patients. Patients with preexisting liver disease may be at increased risk.
Review recent (i.e., within last 6 months) transaminase and bilirubin concentrations before initiating treatment and evaluate periodically during treatment until 2 months after the drug is discontinued. Check liver enzymes in patients who develop symptoms suggestive of hepatic dysfunction (e.g., unexplained nausea, vomiting, abdominal pain, anorexia, fatigue, jaundice, dark urine). Discontinue fingolimod if ALT >3 times ULN and serum total bilirubin >2 times ULN. Do not resume treatment unless an alternative etiology is determined.
Closely monitor patients with severe hepatic impairment as exposure to the drug is doubled in these patients, potentially increasing the risk of adverse effects.
Posterior Reversible Encephalopathy Syndrome (PRES)
PRES reported rarely. Symptoms include sudden onset of severe headache, altered mental status, visual disturbances, and seizure. Although symptoms usually reversible, may evolve into ischemic stroke or cerebral hemorrhage; a delay in diagnosis and treatment of PRES may lead to permanent neurologic sequelae.
If PRES is suspected, discontinue fingolimod.
Respiratory Effects
May decrease pulmonary function tests. Dose-dependent reductions in FEV1 and diffusion lung capacity for carbon monoxide (DLCO) observed as early as 1 month after beginning therapy. FEV1 changes appear reversible after discontinuing fingolimod; insufficient information to determine reversibility of the DLCO decrease after drug discontinuance. Dyspnea reported in placebo-controlled and extension studies.
Obtain spirometry and DLCO when clinically indicated.
Fetal/Neonatal Morbidity and Mortality
Animal studies indicate fingolimod may cause fetal harm. Advise pregnant patients and females of reproductive potential of the potential risk. Use effective contraception in females of reproductive potential during and for 2 months after discontinuance of therapy.
Severe Increase in Disability after Discontinuation
Severe increase in disability with new MRI lesions reported, generally within 12 weeks but up to 24 weeks, after discontinuance. Most patients did not return to functional status obtained during fingolimod therapy.
Monitor patients for a serious increase in disability after discontinuing fingolimod. Monitor for IRIS development after discontinuing fingolimod in the setting of PML.
Tumefactive Multiple Sclerosis
MS relapses with tumefactive demyelinating lesions on imaging reported during treatment or after discontinuation. Most cases occurred within 9 months of starting the drug but may occur at any time including after the drug is discontinued.
If a severe MS relapse occurs during fingolimod treatment, especially during initiation or after stopping the drug, consider tumefactive MS; evaluate and initiate appropriate treatment as clinically indicated.
Increased Blood Pressure
May increase BP. In clinical studies average increases in systemic BP and diastolic BP were approximately 3 and 2 mm Hg, respectively; increases first detected approximately 1 month following treatment initiation and persisted with continued treatment. Hypertension reported in 8% of fingolimod-treated patients in controlled trials.
Monitor BP during therapy.
Malignancies
Basal cell carcinoma, melanoma, squamous cell carcinoma, Kaposi's sarcoma, and Merkel cell carcinoma reported.
Perform skin examinations prior to or shortly after initiation of therapy and periodically thereafter for all patients receiving fingolimod, particularly in patients with risk factors for skin cancer.
Monitor patients for any suspicious skin lesions; if observed, promptly evaluate. Take usual precautions for skin cancer (e.g., limit exposure to sunlight and UV light, use sunscreen).
Cases of lymphoma, including both T-cell types, B-cell types, CNS lymphoma, reported. A greater than expected rate of non-Hodgkin lymphoma also reported.
Immune System Effects Following Discontinuance
Fingolimod remains in the blood and has pharmacodynamic effects, including decreased lymphocyte counts, for up to 2 months following the last dose. Initiating other drugs during this period warrants the same considerations needed for concomitant administration (e.g., risk of additive immunosuppressive effects).
Sensitivity Reactions
Hypersensitivity
Hypersensitivity reactions (e.g., rash, urticaria, angioedema) reported during postmarketing experience.
Specific Populations
Pregnancy
No adequate data regarding developmental risk associated with use of fingolimod during pregnancy; however, teratogenic and embryolethal effects demonstrated in animals.
Females of reproductive potential should use effective contraception during and for 2 months following therapy. Consider the possibility of severe increase in disability in females who discontinue fingolimod for pregnancy. Many cases in which an increase in disability occurred after stopping fingolimod were reported in patients who had stopped fingolimod because of pregnancy or planned pregnancy. In females planning to become pregnant, stop fingolimod 2 months before planned conception.
Encourage patients to enroll in Gilenya pregnancy registry by calling 877-598-7237, by email to gpr@quintiles.com, or on the website [Web].
Lactation
Distributed into milk in rats; not known whether distributed into human milk. Effects of the drug on nursing infant or on milk production not known.
Consider benefits of breastfeeding along with the woman's clinical need for fingolimod and any potential adverse effects on the breastfed infant from the drug or underlying maternal condition.
Females and Males of Reproductive Potential
Before initiating treatment, verify pregnancy status in females of reproductive potential. Counsel such females on the serious risk of fingolimod treatment on the developing fetus and need for effective contraceptive measures during treatment. Due to rate of elimination of the drug, females of reproductive potential should use effective contraceptives for at least 2 months after stopping fingolimod.
Pediatric Use
Safety and efficacy not established in patients <10 years of age.
In pediatric patients ≥10 years of age, adverse effects generally were similar to those observed in adults, with the exception of seizures, which occurred at a higher rate.
It is recommended that pediatric patients receive all age-appropriate vaccinations according to current immunization guidelines, if possible, prior to initiating fingolimod therapy.
Geriatric Use
Insufficient experience in patients ≥65 years of age to determine whether geriatric patients respond differently than younger adults. Use with caution because of possible age-related decreases in hepatic and/or renal function and concomitant disease and other drug therapy.
Hepatic Impairment
Closely monitor patients with severe hepatic impairment (Child-Pugh class C) since fingolimod exposure is doubled and risk of adverse reactions may be greater. No dosage adjustment is recommended in patients with mild or moderate hepatic impairment.
Renal Impairment
Increased systemic exposure (up to 13-fold) of some fingolimod metabolites observed in patients with severe renal impairment; toxicity of these metabolites not fully explored. No dosage adjustment is recommended.
Common Adverse Effects
Adverse effects reported in ≥10% of patients receiving fingolimod and more frequently than with placebo include headache, liver transaminase elevation, diarrhea, cough, influenza, sinusitis, back pain, abdominal pain, and pain in extremity.
Drug Interactions
Primarily metabolized by CYP4F2 and possibly other CYP4F isoenzymes. In vitro studies in hepatocytes indicate that CYP3A4 also may contribute to metabolism if there is potent induction of CYP3A4.
Has little or no inhibitory activity on CYP isoenzymes 1A2, 2A6, 2B6, 2C8, 2C9, 2C19, 2D6, 2E1, 3A4/5, or 4A9/11 (fingolimod only). Similarly, fingolimod-phosphate (an active metabolite) has little or no inhibitory activity on CYP isoenzymes 1A2, 2A6, 2B6, 2C8, 2C9, 2C19, 2D6, 2E1, or 3A4.
Does not substantially induce CYP isoenzymes 1A2, 2B6, 2C8, 2C9, 2C19, 3A (including 3A4), or 4F2 or P-glycoprotein. Fingolimod-phosphate does not induce CYP isoenzymes 1A2, 2B6, 2C8, 2C9, 2C19, 3A, 4F2, 4F3B, or 4F12.
Drugs Affecting Hepatic Microsomal Enzymes
Inhibitors or inducers of CYP isoenzyme 4F2 and possibly other CYP4F isoenzymes: Possible altered exposure of fingolimod and/or fingolimod-phosphate.
Potent CYP450 enzyme inducers: Possible reduced exposure of fingolimod and/or fingolimod-phosphate.
Drugs that Prolong QT Interval
Fingolimod initiation decreases heart rate and may prolong the QT interval; monitor patients concurrently receiving non-antiarrhythmic, QT-prolonging drugs with a known risk of torsades de pointes overnight with continuous ECG in a medical facility.
Drugs that Slow Heart Rate or AV Conduction
Limited experience. Concomitant use during fingolimod initiation may be associated with severe bradycardia or heart block.
Before initiating fingolimod, consult prescribing clinician to determine if possible to switch to drugs that do not slow the heart rate or AV conduction.
In patients who cannot switch to another drug, extended continuous ECG monitoring, including overnight monitoring, recommended after the first dose of fingolimod.
Specific Drugs and Laboratory Tests
|
Drug or Test |
Interaction |
Comments |
|---|---|---|
|
Amantadine |
Clinically important pharmacokinetic interaction unlikely |
|
|
Amitriptyline |
Clinically important pharmacokinetic interaction unlikely |
|
|
Antiarrhythmic agents, class Ia (e.g., quinidine, procainamide) and class III (e.g., amiodarone, sotalol) |
Possible increased risk of torsades de pointes in patients with bradycardia |
Concomitant use contraindicated |
|
Antidepressants, SSRIs (e.g., fluoxetine, paroxetine) |
Pharmacokinetic interaction with fluoxetine and paroxetine unlikely |
|
|
Antipsychotic agents that prolong the QT interval (e.g., chlorpromazine, haloperidol, olanzapine, pimozide, quetiapine, risperidone, thioridazine, ziprasidone) |
Potential additive effects on the QT interval and increased risk of torsades de pointes |
Monitor overnight with continuous ECG in a medical facility during fingolimod initiation |
|
Atropine |
Single-dose fingolimod and fingolimod-phosphate exposure not substantially altered |
|
|
Baclofen |
Clinically important pharmacokinetic interaction unlikely |
|
|
β-Adrenergic blocking agents (e.g., atenolol) |
Risk of severe bradycardia or heart block, particularly during fingolimod initiation Atenolol: Additional 15% reduction of heart rate upon fingolimod initiation; clinically important pharmacokinetic interaction unlikely |
Evaluate if possible to switch to drugs that do not slow heart rate or AV conduction; if switch not possible, overnight continuous ECG monitoring recommended after first dose |
|
Calcium-channel blocking agents (e.g., diltiazem, verapamil) |
Risk of severe bradycardia or heart block, particularly during fingolimod initiation Diltiazem: Clinically important pharmacokinetic interaction unlikely; additive effect on bradycardia not observed in healthy individuals |
Consider switching to drugs that do not slow heart rate or AV conduction; if this is not possible, overnight continuous ECG monitoring recommended after first dose |
|
Carbamazepine |
Concurrent administration of carbamazepine (a potent CYP450 inducer) and fingolimod decreased AUC of fingolimod and fingolimod-phosphate by approximately 40%; clinical importance not known |
|
|
Citalopram |
Potential additive effects on the QT interval and increased risk of torsades de pointes |
Monitor overnight with continuous ECG in a medical facility during fingolimod initiation |
|
Corticosteroids |
Increased risk of immunosuppression and possible infections; clinically important pharmacokinetic interaction unlikely |
|
|
Cyclosporine |
Pharmacokinetics of single-dose fingolimod and steady-state cyclosporine not altered |
|
|
Digoxin |
Risk of severe bradycardia or heart block, particularly during fingolimod initiation |
Consider switching to drugs that do not slow heart rate or AV conduction; if this is not possible, overnight continuous ECG monitoring recommended after first dose |
|
Erythromycin |
Potential additive effects on the QT interval and increased risk of torsades de pointes |
Monitor overnight with continuous ECG in a medical facility during fingolimod initiation |
|
Gabapentin |
Clinically important pharmacokinetic interaction unlikely |
|
|
Immunomodulating therapies (e.g., antineoplastic or immunosuppressive therapies) |
Increased risk of immunosuppression and possible infections |
Use caution when switching from MS drugs with prolonged immunosuppressive effects (e.g., natalizumab, mitoxantrone, teriflunomide) to fingolimod; consider duration and mechanism of these drugs when initiating fingolimod therapy |
|
Isoproterenol |
Single-dose fingolimod and fingolimod-phosphate exposure not substantially altered |
|
|
Ketoconazole |
Blood concentrations of fingolimod and fingolimod-phosphate increased by 1.7-fold; possible increased risk of adverse effects |
Closely monitor patients receiving systemic ketoconazole concomitantly; consider fingolimod dosage reduction if necessary |
|
Lymphocyte counts |
Fingolimod reduces blood lymphocyte counts via redistribution in secondary lymphoid organs |
Do not utilize peripheral blood lymphocyte count to evaluate lymphocyte subset status Ensure availability of a recent CBC before initiating fingolimod therapy |
|
Methadone |
Potential additive effects on the QT interval and increased risk of torsades de pointes |
Monitor overnight with continuous ECG in a medical facility during fingolimod initiation |
|
Modafinil |
Clinically important pharmacokinetic interaction unlikely |
|
|
Oral contraceptives |
Steady-state exposure of ethinyl estradiol and levonorgestrel not substantially affected Interaction not studied with oral contraceptives containing other progestins; clinically important pharmacokinetic interactions unlikely |
|
|
Oxybutynin chloride |
Clinically important pharmacokinetic interaction unlikely |
|
|
Pregabalin |
Clinically important pharmacokinetic interaction unlikely |
|
|
Vaccines |
Reduced immune response to vaccination; vaccination may be less effective during and for up to 2 months following discontinuance of fingolimod Risk of infection with live attenuated vaccines |
Avoid use of live attenuated vaccines during and for 2 months after fingolimod treatment |
Fingolimod Hydrochloride (Sytemic) Pharmacokinetics
Absorption
Bioavailability
Apparent absolute oral bioavailability is 93%. Peak blood concentrations attained approximately 12–16 hours following oral administration.
Food
Food does not alter peak concentrations or AUC of fingolimod or fingolimod-phosphate.
Plasma Concentrations
Steady-state concentrations achieved within 1–2 months following once-daily oral administration.
Special Populations
Severe renal impairment: Peak blood concentrations and AUCs of fingolimod increased by 32 and 43%, respectively; peak blood concentrations and AUCs of fingolimod-phosphate increased by 25 and 14%, respectively. Systemic exposure of 2 fingolimod metabolites (M2 and M3) increased by threefold and 13-fold, respectively.
Mild or moderate renal impairment: Pharmacokinetics not evaluated.
Mild, moderate, or severe hepatic impairment (Child-Pugh class A, B, or C, respectively): Fingolimod AUCs increased by 12, 44, and 103%, respectively.
Severe hepatic impairment: Peak concentrations of fingolimod-phosphate decreased by 22%; AUC not substantially changed.
Distribution
Extent
Fingolimod extensively distributes into body tissues.
Fingolimod: Highly distributes (86%) in RBCs.
Fingolimod-phosphate: Smaller uptake in blood cells (<17%).
Distributed into milk in rats; not known whether distributes into human milk.
Plasma Protein Binding
Fingolimod and fingolimod-phosphate: >99.7%.
Elimination
Metabolism
Biotransformation occurs by 3 main pathways: reversible stereoselective phosphorylation to the pharmacologically active S-enantiomer of fingolimod-phosphate, oxidative biotransformation mainly via the CYP4F2 isoenzyme and possibly other CYP4F isoenzymes with subsequent fatty acid-like degradation to inactive metabolites, and formation of pharmacologically inactive nonpolar ceramide analogs of fingolimod.
CYP3A4 also may contribute to metabolism if potent induction of CYP3A4 occurs.
Elimination Route
About 81% of the dose is slowly excreted in urine as inactive metabolites. Fingolimod and fingolimod-phosphate are not excreted intact in urine, but are the major components in feces with amounts of each representing <2.5% of the dose.
Half-life
Fingolimod: 6–9 days; fingolimod-phosphate appears to have a similar half-life.
Special Populations
Severe renal impairment: Half-life of fingolimod is unchanged.
Mild hepatic impairment: Half-life of fingolimod is unchanged.
Moderate or severe hepatic impairment: Half-life of fingolimod is prolonged by about 50%.
Stability
Storage
Oral
Capsules
20–25°C (may be exposed to 15-30°C); protect from moisture.
Tablets, Orally Disintegrating
20–25°C (excursions permitted to 15–30ºC). Protect from moisture. Store in sealed blister pack. Do not open blister until ready to administer.
Actions
-
Derived from the fungal metabolite myriocin; used orally as a disease-modifying treatment for multiple sclerosis (MS).
-
Sphingosine kinase, predominantly type 2, metabolizes fingolimod to the active metabolite, fingolimod-phosphate. Fingolimod-phosphate is a sphingosine 1-phosphate (S1P) receptor modulator and binds with high affinity to S1P receptor subtypes 1, 3, 4, and 5.
-
The S1P1 receptor regulates lymphocyte egress from both the thymus and peripheral lymphoid organs and is essential for lymphocyte recirculation. Binding of fingolimod-phosphate to S1P1 blocks the capacity of lymphocytes to egress from lymph nodes, reducing the number of lymphocytes in the peripheral blood and CNS.
-
Exact mechanism of fingolimod’s therapeutic effects in MS unknown; may involve reduction of lymphocyte migration into the CNS.
-
Preclinical findings suggest fingolimod may directly affect neuropathologic processes such as neurodegeneration, gliosis, and endogenous repair mechanisms within the CNS through modulation of S1P receptors expressed on neural cells.
Advice to Patients
-
Advise patients to read the medication guide prior to initiating therapy and each time the prescription is refilled.
-
Risk of transient decrease in heart rate, particularly after the first dose; may recur when therapy is resumed after an interruption. Advise patients that medical observation is required after the first dose and also may be required after the drug is restarted following treatment interruption. Stress importance of immediately contacting clinician or seeking emergency care if dizziness, tiredness, or slow or irregular heartbeat occurs.
-
Inform patients that PML has occurred in fingolimod-treated patients. Advise patients to inform their clinician of any symptoms suggestive of PML (e.g., progressive weakness on one side of the body; clumsiness of limbs; vision disturbance; changes in thinking, memory, or orientation leading to confusion and personality changes) that have progressed over days to weeks.
-
Possible increased risk of infections, since fingolimod may reduce lymphocyte count. Stress importance of immediately contacting clinician if any symptoms of infection (e.g., fever, chills, tiredness, body aches, nausea, vomiting, or headache with fever, neck stiffness, sensitivity to light, nausea, or confusion) develop during or within 2 months after fingolimod therapy. Inform patients that prior or concomitant use of drugs that suppress the immune system may increase risk of infection.
-
Inform clinicians of any vaccinations given within 1 month before starting fingolimod. Stress importance of avoiding some vaccines during treatment and for 2 months after drug discontinuance. Advise patients to delay fingolimod therapy until after varicella zoster virus (VZV) vaccination if they have not had chickenpox or a previous VZV vaccination.
-
Risk of posterior reversible encephalopathy syndrome; advise patients to immediately report any manifestations (e.g., sudden onset of severe headache, altered mental status, visual disturbance, or seizure) to their clinician. Any delay in treatment could lead to permanent neurologic disability.
-
Risk of macular edema, particularly in individuals who are diabetic or have had uveitis. Some symptoms may resemble those of an MS attack (optic neuritis); some patients may not notice symptoms. Vision testing recommended when starting fingolimod therapy, 3–4 months after treatment initiation, periodically while on therapy, and any time vision changes occur. Stress importance of immediately contacting clinician if any vision changes (e.g., blurriness or shadows in the center of vision, blind spot in the center of vision, sensitivity to light, unusually colored or tinted vision) occur. Inform patients that their risk of developing macular edema is higher if they have diabetes or have had uveitis.
-
Risk of breathing problems. Stress importance of immediately contacting clinician if any breathing difficulties (e.g., new onset or worsening of shortness of breath) occur.
-
Risk of increased liver enzymes and liver injury. Stress importance of contacting clinician if unexplained nausea, vomiting, abdominal pain, fatigue, anorexia, jaundice, and/or dark urine occurs. Inform patients that liver function tests will be monitored before treatment and periodically during treatment.
-
Risk of basal cell carcinoma and melanoma; advise patients that any suspicious skin lesions should be promptly evaluated. Advise patients to limit exposure to sunlight and UV light by wearing protective clothing and using a sunscreen with a high protection factor.
-
Risk of hypersensitivity reactions; advise patients to contact their clinician if any manifestations (e.g., rash, urticaria, angioedema) occur.
-
Inform clinicians if worsening symptoms of multiple sclerosis occur after stopping fingolimod.
-
Stress importance of not discontinuing fingolimod without first talking with clinician. Advise patients to inform their clinician if they accidently take more than a prescribed dose.
-
Risk of fetal harm. Advise female patients of reproductive potential to use effective contraception during therapy and for 2 months after the last dose. Stress importance of women immediately informing their clinician if pregnancy occurs during this time period.
-
Stress importance of women informing clinicians if they plan to breast-feed.
-
Advise patients that fingolimod remains in the blood and continues to have effects (e.g., decreased lymphocyte counts) for up to 2 months after the last dose.
-
Stress importance of patients informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, vitamins, and herbal supplements, as well as any concomitant illnesses.
-
Inform patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
Fingolimod is available through a specialty pharmacy network. Clinicians may consult the Gilenya website at [Web] or the Tascenso ODT website at [Web] for availability information.
|
Routes |
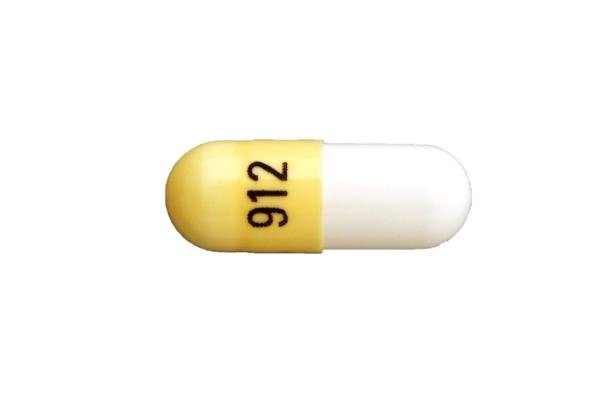
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules |
0.25 mg (of fingolimod) |
Gilenya |
Novartis |
|
0.5 mg (of fingolimod) |
Gilenya |
Novartis |
||
|
Tablets, orally disintegrating |
0.25 mg (of fingolimod) |
Tascenso ODT |
Cycle Pharmaceuticals |
|
|
0.5 mg (of fingolimod) |
Tascenso ODT |
Cycle Pharmaceuticals |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions September 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Frequently asked questions
- Gilenya vs Tecfidera. How do they compare?
- How much does Gilenya cost?
- What happens when you stop taking Gilenya?
- Does Gilenya suppress the immune system?
- Where is Gilenya manufactured and by whom?
- How long does it take Gilenya to work?
- Does Gilenya cause hair loss?
- What does Gilenya do for multiple sclerosis (MS)?
More about fingolimod
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (99)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: selective immunosuppressants
- Breastfeeding
- En español