Fingolimod Dosage
Medically reviewed by Drugs.com. Last updated on Jun 12, 2025.
Applies to the following strengths: 0.5 mg; 0.25 mg
Usual Adult Dose for:
Usual Pediatric Dose for:
Additional dosage information:
Usual Adult Dose for Multiple Sclerosis
0.5 mg orally once a day
Comments:
- This drug can be taken with or without food.
- See DOSE ADJUSTMENTS for recommended pre-dose testing and monitoring recommendations.
Use: For relapsing forms of multiple sclerosis (MS)
Usual Pediatric Dose for Multiple Sclerosis
10 years and older and weighing 40 kg or less:
0.25 mg orally once a day
10 years and older and weighing more than 40 kg:
0.5 mg orally once a day
Comments:
- This drug can be taken with or without food.
- See DOSE ADJUSTMENTS for recommended pre-dose testing and monitoring recommendations.
Use: For relapsing forms of multiple sclerosis (MS) in patients 10 years and older
Renal Dose Adjustments
No adjustment recommended.
Liver Dose Adjustments
Mild to moderate hepatic impairment: No adjustment recommended.
Severe hepatic impairment: Closely monitor patients.
Dose Adjustments
- Obtain a cardiac evaluation in patients with certain preexisting conditions (e.g., ischemic heart disease, history of myocardial infarction, congestive heart failure, history of cardiac arrest, cerebrovascular disease, uncontrolled hypertension, history of symptomatic bradycardia, history of recurrent syncope, severe untreated sleep apnea, AV block, sinoatrial heart block).
- Prior to starting therapy, determine if patients are taking drugs that could slow heart rate or atrioventricular conduction.
- If patients are taking antineoplastic, immunosuppressive, or immune-modulating therapies, or if there is a history of prior use of these drugs, consider possible unintended additive immunosuppressive effects before initiating therapy with this drug.
- Test patients for antibodies to varicella zoster virus (VZV) before initiating therapy; VZV vaccination of antibody negative patients is recommended prior to initiating this drug.
FIRST 6 HOUR MONITORING:
Administer the first dose in a setting with resources to manage symptomatic bradycardia. Monitor all patients for 6 hours after the first dose for bradycardia with hourly pulse and blood pressure measurement.
ADDITIONAL MONITORING AFTER 6-HOUR MONITORING:
- Continue monitoring until the abnormality resolves if any of the following is present (even in the absence of symptoms) after 6 hours:
2) The heart rate 6 hours post dose is at the lowest value post dose suggesting that the maximum pharmacodynamic effect on the heart may not have occurred.
3) The ECG 6 hours post dose shows new onset second degree or higher atrioventricular (AV) block.
- If post dose symptomatic bradycardia occurs, initiate appropriate management, begin continuous ECG monitoring, and continue monitoring until the symptoms have resolved if no pharmacological treatment is required. If pharmacological
OVERNIGHT MONITORING:
Continuous overnight ECG monitoring in a medical facility should be instituted:
- In patients that require pharmacologic intervention for symptomatic bradycardia. In these patients, the first dose monitoring strategy should be repeated after the second dose.
- In patients with some preexisting heart and cerebrovascular conditions.
- In patients with a prolonged QTc interval before dosing or during 6 hour observation, or at additional risk for QT prolongation, or on concurrent therapy with QT prolonging drugs with a known risk of torsade de pointes.
- In patients receiving concurrent therapy with drugs that slow heart rate or atrioventricular conduction.
MONITORING AFTER REINITIATION OF THERAPY FOLLOWING DISCONTINUATION:
- When restarting this drug after discontinuation for more than 14 days after the first month of treatment, perform first dose monitoring, because effects on heart rate and AV conduction may recur on reintroduction of therapy. The same precautions (first dose monitoring) as for initial dosing are applicable.
- Within the first 2 weeks of therapy, first dose procedures are recommended after interruption of 1 day or more; during weeks 3 and 4 of treatment first dose procedures are recommended after treatment interruption of more than 7 days.
Precautions
CONTRAINDICATIONS:
- Hypersensitivity to the active component or any of the ingredients
- Patients with myocardial infarction (MI), unstable angina pectoris, stroke/transient ischemic attack (TIA), decompensated heart failure (requiring inpatient treatment), or New York Heart Association (NYHA) class III/IV heart failure in the previous 6 months
- Patients with a history or presence of Mobitz Type II second-degree or third-degree atrioventricular (AV) block or sick sinus syndrome, unless patient has a functioning pacemaker
- Patients with a baseline QTc interval 500 msec or greater
- Concomitant treatment with Class Ia or Class III anti-arrhythmic drugs
Safety and efficacy have not been established in patients younger than 10 years.
Consult WARNINGS section for additional precautions.
Dialysis
Data not available
Other Comments
Administration advice:
- Take with or without food.
- Doses higher than 0.5 mg are associated with a greater incidence of adverse reactions without additional benefit.
Storage requirements:
- Store at room temperature in the original blister pack; protect from moisture.
Frequently asked questions
- Gilenya vs Tecfidera. How do they compare?
- How much does Gilenya cost?
- What happens when you stop taking Gilenya?
- Does Gilenya suppress the immune system?
- Where is Gilenya manufactured and by whom?
- How long does it take Gilenya to work?
- Does Gilenya cause hair loss?
- What does Gilenya do for multiple sclerosis (MS)?
More about fingolimod
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (99)
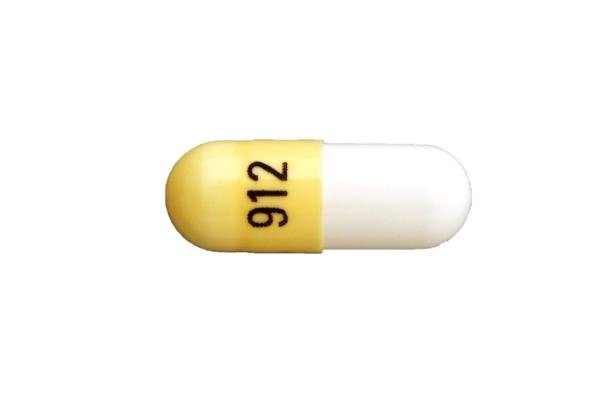
- Drug images
- Side effects
- During pregnancy
- Drug class: selective immunosuppressants
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
See also:
Copaxone
Copaxone is used to treat relapsing forms of multiple sclerosis (MS) in adults (including ...
Tecfidera
Tecfidera (dimethyl fumarate) is used to treat relapsing forms of multiple sclerosis. Learn about ...
Kesimpta
Kesimpta is used to treat relapsing forms of multiple sclerosis (MS), including clinically isolated ...
Aubagio
Aubagio (teriflunomide) is used to reduce flare-ups in people with relapsing multiple sclerosis ...
Avonex
Avonex is an interferon used to treat relapsing multiple sclerosis. It is given by injection into a ...
Tysabri
Tysabri is used to treat multiple sclerosis and Crohn's disease. Learn about side effects ...
Gilenya
Gilenya (fingolimod) is used to treat relapsing forms of multiple sclerosis. Includes Gilenya side ...
Betaseron
Betaseron is used to treat relapsing multiple sclerosis (MS). Learn about side effects ...
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.