Linezolid (oral/injection)
Generic name: linezolid (oral/injection) [ lin-EZ-oh-lid ]
Brand name: Zyvox
Dosage forms: intravenous solution (2 mg/mL-D5%; 2 mg/mL-NaCl 0.9%), oral powder for reconstitution (100 mg/5 mL),
... show all 3 dosage forms
Drug class: Oxazolidinone antibiotics
What is linezolid?
Linezolid is an antibiotic that fights bacteria in the body. Linezolid is also an MAO (monoamine oxidase) inhibitor.
Linezolid is used to treat different types of bacterial infections, such as pneumonia, skin infections, and infections that are resistant to other antibiotics.
Linezolid may also be used for purposes not listed in this medication guide.
Linezolid side effects
Get emergency medical help if you have signs of an allergic reaction (hives, difficult breathing, swelling in your face or throat) or a severe skin reaction (fever, sore throat, burning eyes, skin pain, red or purple skin rash with blistering and peeling).
Linezolid may cause serious side effects. Call your doctor at once if you have:
-
vision problems, changes in color vision;
-
severe stomach pain, diarrhea that is watery or bloody;
-
a seizure;
-
sweating, feeling anxious or shaky (may be signs of low blood sugar);
-
lactic acidosis--unusual muscle pain, trouble breathing, stomach pain, vomiting, irregular heart rate, dizziness, feeling cold, or feeling very weak or tired; or
-
low blood cell counts--fever, chills, tiredness, weakness, confusion, mouth sores, skin sores, easy bruising, unusual bleeding, pale skin, cold hands and feet, feeling light-headed or short of breath.
Seek medical attention right away if you have symptoms of serotonin syndrome, such as: agitation, hallucinations, fever, sweating, shivering, fast heart rate, muscle stiffness, twitching, loss of coordination, nausea, vomiting, or diarrhea.
Common side effects of linezolid may include:
-
nausea, vomiting, diarrhea;
-
rash;
-
anemia (low red blood cells); or
-
headache, dizziness.
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Related/similar drugs
Warnings
Some medicines can cause unwanted or dangerous effects when used with linezolid. Tell your doctor about all other medicines you use.
Do not use linezolid if you have used an MAO inhibitor in the past 14 days, such as isocarboxazid, linezolid, methylene blue injection, phenelzine, or tranylcypromine.
Before taking this medicine
You should not use linezolid if you are allergic to it.
Do not use linezolid if you have used an MAO inhibitor in the past 14 days. A dangerous drug interaction could occur. MAO inhibitors include isocarboxazid, linezolid, methylene blue injection, phenelzine, tranylcypromine, and others.
Tell your doctor if you also take stimulant medicine, opioid medicine, herbal products, or medicine for depression, mental illness, Parkinson's disease, migraine headaches, serious infections, or prevention of nausea and vomiting. An interaction with linezolid could cause a serious condition called serotonin syndrome.
Tell your doctor if you have ever had:
-
a thyroid disorder;
-
bone marrow suppression or a weak immune system;
-
kidney or liver disease;
-
pheochromocytoma (adrenal gland tumor);
-
diabetes;
-
seizures; or
-
if you use a catheter.
Tell your doctor if you are pregnant or breastfeeding.
If you are breastfeeding, tell your doctor if you notice diarrhea or vomiting in the nursing baby.
Linezolid liquid may contain phenylalanine and could be harmful if you have phenylketonuria (PKU).
How is linezolid used?
Follow all directions on your prescription label and read all medication guides or instruction sheets. Use the medicine exactly as directed.
Linezolid oral is taken by mouth.
Linezolid tablets or liquid can be taken with or without food.
Gently mix the oral suspension (liquid) by turning the bottle upside down 3 to 5 times. Do not shake. Measure a dose with the supplied syringe or a dose-measuring device (not a kitchen spoon).
Linezolid injection is given in a vein.
Read and follow all Instructions for Use. Ask your doctor or pharmacist if you need help.
Prepare an injection only when you are ready to give it. Call your pharmacist if the medicine has particles in it.
Do not reuse a needle or syringe. Place them in a puncture-proof "sharps" container and dispose of it following state or local laws. Keep out of the reach of children and pets.
You will need frequent medical tests. Your vision and blood pressure may also need to be checked often.
Keep using linezolid even if your symptoms quickly improve. Skipping doses could make your infection resistant to medication. Linezolid will not treat a viral infection (flu or a common cold).
Store all forms of linezolid at room temperature away from moisture, heat, and light. Do not freeze. Throw away any liquid not used within 21 days.
What happens if I miss a dose?
Use the medicine as soon as you can, but skip the missed dose if it is almost time for your next dose. Do not use two doses at one time.
What happens if I overdose?
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222.
What should I avoid while using linezolid?
Avoid taking anti-diarrhea medicine without first asking your doctor. Diarrhea may be a sign of a new infection.
Eating tyramine while you are using linezolid can raise your blood pressure to dangerous levels. Avoid foods that have a high level of tyramine, such as:
-
aged cheeses or meats;
-
pickled or fermented meats, smoked or air-dried meats;
-
sauerkraut;
-
soy sauce;
-
tap beer (alcoholic and nonalcoholic);
-
red wine; or
-
any meat, cheese, or other protein-based food that has been improperly stored.
You should be very familiar with the list of foods you must avoid while you are using linezolid.
What other drugs will affect linezolid?
Many drugs can affect linezolid, and some drugs should not be used at the same time. Tell your doctor about all other medicines you use. This includes prescription and over-the-counter medicines, vitamins, and herbal products. Not all possible interactions are listed here.
Frequently asked questions
More about linezolid
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (32)
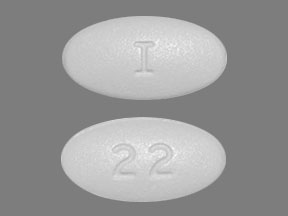
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: oxazolidinone antibiotics
- Breastfeeding
- En español
Patient resources
- Linezolid (Intravenous) advanced reading
- Linezolid (Oral) (Advanced Reading)
- Linezolid Tablets
- Linezolid Injection
- Linezolid Suspension
Other brands
Professional resources
- Linezolid monograph
- Linezolid Injection (FDA)
- Linezolid Oral Suspension (FDA)
- Linezolid Tablets (FDA)
Other brands
Related treatment guides
Further information
Remember, keep this and all other medicines out of the reach of children, never share your medicines with others, and use this medication only for the indication prescribed.
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Copyright 1996-2025 Cerner Multum, Inc. Version: 11.02.