Linezolid Side Effects
Medically reviewed by Drugs.com. Last updated on Oct 1, 2024.
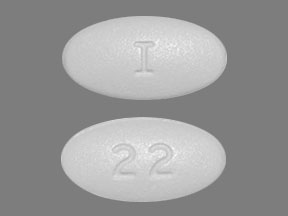
Applies to linezolid: oral powder for suspension, oral tablet.
Other dosage forms:
Precautions
It is very important that your doctor check your or your child's progress while you are taking this medicine, to see if the medicine is working properly. Blood and urine tests may be needed to check for any unwanted effects.
If your or your child's symptoms do not improve within 28 days or if they become worse, check with your doctor.
You should not use this medicine if you or your child have used an MAO inhibitor (MAOI), including isocarboxazid, phenelzine, Eldepryl®, Marplan®, Nardil®, or Parnate® within the past 14 days. Also, do not use this medicine if you or your child are also using the following medicines: buspirone (Buspar®), dobutamine (Dobutrex®), dopamine (Intropin®), epinephrine (Adrenalin®), norepinephrine (Levophed®), cold medicines or decongestants (eg, phenylpropanolamine, pseudoephedrine, or Sudafed®), medicine to treat depression (eg, amitriptyline, bupropion, doxepin, fluoxetine, nortriptyline, paroxetine, Celexa®, Effexor®, Elavil®, Lexapro®, Paxil®, or Zoloft®), medicine to treat migraine headaches (eg, sumatriptan, zolmitriptan, Axert®, Imitrex®, or Zomig®), or narcotic pain medicines (eg, meperidine, Demerol®).
Linezolid can lower the number of white blood cells in your blood temporarily, increasing the chance of getting an infection. It can also lower the number of platelets, which are necessary for proper blood clotting. If this occurs, there are certain precautions your doctor may ask you to take, especially when your blood count is low, to reduce the risk of infection or bleeding:
- If you can, avoid people with infections. Check with your doctor immediately if you think you or your child are getting an infection or if you get a fever or chills, cough or hoarseness, lower back or side pain, or painful or difficult urination.
- Check with your doctor immediately if you notice any unusual bleeding or bruising, black, tarry stools, blood in the urine or stools, or pinpoint red spots on your skin.
This medicine may cause infertility to men. Talk with your doctor before using this medicine if you plan to have children.
This medicine may cause diarrhea, and in some cases it can be severe. It may occur 2 months or more after you Stop taking linezolid. Do not take any medicine to treat diarrhea without first checking with your doctor. If you have any questions or if mild diarrhea continues or gets worse, check with your doctor.
You may develop low blood sugar while you or your child are taking this medicine. You may feel weak, drowsy, confused, anxious, or very hungry. You may have trouble seeing or have a headache that won't go away. Ask your doctor what you should do if this happens. Some things that can lead to low blood sugar are exercising more than normal or waiting too long to eat.
This medicine may cause a serious reaction called lactic acidosis (build-up of acid in the blood). Call your doctor right away if you or your child feel very tired, weak, or nauseated, if you vomit or have trouble breathing, or if you feel lightheaded or fainting.
This medicine may cause serious condition called serotonin syndrome when taken with certain medicines, including medicines to treat depression (SSRIs) or narcotic pain medicines. Check with your doctor first before taking any other medicines. Contact your doctor right away if you or your child experience agitation, confusion, diarrhea, fever, overactive reflexes, poor coordination, restlessness, shivering, sweating, or trembling or shaking.
Check with your doctor right away if blurred vision, difficulty in reading, or any other change in vision occurs during treatment with this medicine. Your eyes may need to be checked by an ophthalmologist (eye doctor).
When taken with certain foods or drinks, linezolid can cause an increase in blood pressure. To avoid this, do not eat large amounts of foods or drink beverages that have a high tyramine content (most common in foods that are aged, fermented, pickled, or smoked to increase their flavor, including aged cheeses, air-dried, fermented, or smoked fish, meat, or poultry, sauerkraut, soy sauce, red wine, or tap beer). If a list of these foods and beverages is not given to you, ask your doctor to provide one.
Check with your doctor right away if you have agitation, coma, confusion, decreased urine output, depression, dizziness, headache, hostility, increased thirst, irritability, lethargy, muscle pain or cramps, muscle twitching, nausea or vomiting, rapid weight gain, seizures, stupor, swelling of the face, ankles, or hands, or unusual tiredness or weakness. These may be symptoms of hyponatremia (low sodium levels in the blood) or syndrome of inappropriate antidiuretic hormone (SIADH).
Do not take other medicines unless thy have been discussed with your doctor. This includes prescription or nonprescription (over-the-counter [OTC]) medicines and herbal or vitamin supplements.
Serious side effects of linezolid
Along with its needed effects, linezolid may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking linezolid:
More common side effects
- chills
- confusion
- diarrhea
- dizziness
- fainting
- fast heartbeat
- fever
- lightheadedness
- pale skin
- rapid, shallow breathing
- rash
- trouble breathing
- unusual bleeding or bruising
- unusual tiredness or weakness
Less common side effects
- black, tarry stools
- bleeding gums
- blood in the urine or stools
- bluish lips or skin
- body aches or pain
- chest pain or tightness
- constipation
- cough
- decreased urine
- dry mouth
- dryness or soreness of the throat
- ear congestion
- headache
- hoarseness
- increased thirst
- irregular heartbeat
- loss of appetite
- loss of voice
- mood changes
- muscle pain or cramps
- nausea or vomiting
- numbness or tingling in the hands, feet, or lips
- painful or difficult urination
- pinpoint red spots on the skin
- runny or stuffy nose
- seizures
- severe stomach pain
- sneezing
- sores, ulcers, or white spots on the lips or in the mouth
- swollen glands
- trouble with swallowing
- voice changes
- vomiting of blood or material that looks like coffee grounds
Incidence not known
- agitation
- blindness
- blistering, peeling, or loosening of the skin
- blurred vision
- burning, numbness, tingling, or painful sensations
- coma
- decreased vision
- depression
- eye pain
- general feeling of discomfort
- hives, itching
- hostility
- irritability
- joint pain
- large, hive-like swelling on the face, eyelids, lips, tongue, throat, hands, legs, feet, or sex organs
- lethargy
- muscle pain, cramping, or twitching
- puffiness or swelling of the eyelids or around the eyes, face, lips, or tongue
- rapid weight gain
- red skin lesions, often with a purple center
- red, irritated eyes
- sleepiness or unusual drowsiness
- stomach discomfort
- stupor
- swelling of the face, ankles, or hands
- swollen glands
- unexplained bleeding or bruising
- unsteadiness or awkwardness
- weakness in the arms, hands, legs, or feet
Other side effects of linezolid
Some side effects of linezolid may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
Less common side effects
- bleeding, blistering, burning, coldness, discoloration of the skin, feeling of pressure, hives, infection, inflammation, itching, lumps, numbness, pain, rash, redness, scarring, soreness, stinging, swelling, tenderness, tingling, ulceration, or warmth at the injection site
- change in taste
- discoloration of the tongue
- itching of the vagina or outside genitals
- pain during sexual intercourse
- pain in the arms or legs
- sore mouth or tongue
- thick, white curd-like vaginal discharge without odor or with mild odor
- trouble sleeping
Incidence not known
- discoloration of the tooth
See also:
Zyvox
Zyvox treats bacterial infections, such as pneumonia, skin infections, and infections resistant to ...
Vancocin
Vancocin is used for bacteremia, bacterial endocarditis prevention, bacterial infection, bone ...
Botox
Botox is used cosmetically to reduce facial lines and wrinkles and for medical purposes for ...
Floxin
Floxin (ofloxacin) is used to treat infections that cause bronchitis, pneumonia, chlamydia ...
Cubicin
Cubicin is used to treat bacterial infections of the skin and underlying tissues. Learn about side ...
Firvanq
Firvanq is used for bacterial infection, clostridioides difficile infection, enterocolitis
Synercid
Synercid is used for bacteremia, methicillin-resistant staphylococcus aureus infection, skin or ...
Dalfopristin/quinupristin
Dalfopristin/quinupristin is used for bacteremia, methicillin-resistant staphylococcus aureus ...
Daptomycin
Daptomycin is used for bacteremia, endocarditis, methicillin-resistant staphylococcus aureus ...
For healthcare professionals
Applies to linezolid: intravenous solution, oral powder for reconstitution, oral tablet.
General adverse events
This drug was discontinued due to side effects in up to 3.5% of patients. The most common side effects leading to discontinuation were diarrhea, headache, nausea, and vomiting.[Ref]
Nervous system
- Common (1% to 10%): Headache, dizziness, taste alteration/perversion (metallic taste)
- Uncommon (0.1% to 1%): Convulsions, hypoesthesia, paresthesia, tinnitus
- Frequency not reported: Drowsiness, seizure, Bell's palsy, sensory loss
- Postmarketing reports: Serotonin syndrome (with concomitant serotonergic agents), peripheral neuropathy[Ref]
Several cases of peripheral and/or optic neuropathy have been reported, mainly when the duration of therapy was longer than 28 days. For example, irreversible sensory loss and peripheral neuropathy were reported in a patient after using this drug for 6 months for actinomycosis. The time from the onset of therapy to the first sign of peripheral neuropathy averaged 4 months (range: 10 days to 6 months) in 10 patients with only peripheral neuropathy. In all patients with peripheral neuropathy (n=16), complete recovery was not observed after this drug was stopped.
At least 15 instances of serotonin syndrome have been reported in patients using this drug with citalopram, sertraline, venlafaxine, fluoxetine, or paroxetine; other concurrent drugs and/or comorbidities may have contributed to the development of serotonin syndrome. The time from the onset of therapy to the first sign of serotonin syndrome averaged 4 days (range: 1 to 20 days) and from the first sign to stopping this drug ranged from 1 to 16 days. Symptoms resolved within 1 to 9 days in 14 patients while 1 patient died suddenly. Three patients died. The first patient developed symptoms 3 weeks after concurrent use of this drug and citalopram. Severe lactic acidosis developed followed by myocardial infarction, and after 3 further episodes of cardiac arrest, the patient died. The second patient stopped sertraline on day 1 and developed symptoms on day 9 of linezolid therapy. The patient had cardiopulmonary arrest, then anoxic brain injury, hypertension, tachycardia, and diarrhea, and died in 2 weeks; a similar incident occurred 6 weeks earlier when this drug and sertraline were used. The third patient, who was using citalopram, developed symptoms on day 2 of linezolid therapy and died with cerebral hemorrhage 1 month after the start of serotonin syndrome despite stopping this drug.
A 49-year-old male with multiple comorbidities developed symptoms on day 21 of therapy and was diagnosed with Bell's palsy; symptoms included strange sensation in mouth (no pain, sores, blisters), excessive tearing of left eye, inability to drink properly, left facial frowning, and left-sided facial weakness (involving upper and lower facial muscles). This drug was discontinued and the Bell's palsy completely resolved by day 90. The patient restarted linezolid 5 months later and again showed symptoms on day 21 of therapy. This drug was discontinued and by day 35, the Bell's palsy had practically resolved. The patient had no remaining symptoms 4 months after his second episode.
Convulsions have also been reported during postmarketing experience.[Ref]
Gastrointestinal
- Common (1% to 10%): Diarrhea, nausea, vomiting, elevated lipase, elevated amylase, tongue discoloration, oral candidiasis, localized abdominal pain, generalized abdominal pain, constipation, dyspepsia
- Uncommon (0.1% to 1%): Pancreatitis, gastritis, abdominal distention, dry mouth, glossitis, loose stools, stomatitis, tongue disorder
- Rare (0.01% to 0.1%): Antibiotic-associated colitis (including pseudomembranous colitis), superficial tooth discoloration
- Frequency not reported: Clostridium difficile-associated diarrhea, lingua villosa nigra, C difficile colitis[Ref]
In cases with known outcome, tooth discoloration was removable with professional dental cleaning (manual descaling).
A 60-year-old man with spondylodiscitis developed a fatal case of C difficile colitis after a long-term course of this drug.
Superficial tooth discoloration and tongue discoloration have also been reported during postmarketing experience.[Ref]
Hematologic
- Common (1% to 10%): Decreased hemoglobin, decreased platelet count, decreased WBC count, anemia, decreased neutrophils, thrombocytopenia/low platelet count (some requiring platelet transfusions), decreased leukocytes, increased neutrophils, increased eosinophils, decreased hematocrit, decreased RBC count, increased platelet count, increased WBC count
- Uncommon (0.1% to 1%): Leukopenia, neutropenia, eosinophilia, increased reticulocyte count
- Rare (0.01% to 0.1%): Pancytopenia
- Frequency not reported: Red cell hypoplasia, myelotoxicity, bleeding events
- Postmarketing reports: Myelosuppression (including anemia, leukopenia, pancytopenia, thrombocytopenia), sideroblastic anemia[Ref]
Thrombocytopenia (platelets less than 100,000/mm3) has been reported in 32% of patients (n=19) using this drug for more than 10 days. In another study (n=295), thrombocytopenia (platelets less than 150 x 10[9]/L) occurred in 6.4% of patients and severe thrombocytopenia (platelets less than 50 x 10[9]/L) occurred in 0.3% using this drug for more than 5 days. It has been suggested that the mechanism of linezolid-associated thrombocytopenia was immune-mediated.
In a study of patients with linezolid-associated thrombocytopenia, the use of vitamin B6 helped reverse the incidence of thrombocytopenia. Vitamin B6 was most effective when used after this drug was held. Once hematologic levels returned to baseline, coadministration of this drug with vitamin B6 resulted in stable hemoglobin levels for the remainder of therapy.
Another study compared this drug plus 50 mg vitamin B6 per day (n=31) with this drug alone (n=62) administered to patients with cancer. This study concluded vitamin B6 was not beneficial in the prevention of leukopenia or thrombocytopenia, but found a possible trend towards the prevention of anemia.[Ref]
Hepatic
- Common (1% to 10%): Elevated ALT, elevated AST, abnormal liver function tests
- Uncommon (0.1% to 1%): Elevated total bilirubin[Ref]
Metabolic
- Common (1% to 10%): Elevated alkaline phosphatase, elevated LDH, elevated nonfasting glucose
- Uncommon (0.1% to 1%): Hyponatremia, decreased nonfasting glucose
- Frequency not reported: Hyperlactatemia, metabolic acidosis, hypokalemia
- Postmarketing reports: Lactic acidosis, hypoglycemia (including symptomatic episodes)[Ref]
At least 7 instances of lactic acidosis have been reported after use of this drug. The time from the onset of therapy to the first sign of lactic acidosis ranged from 1 to 16 weeks. This drug was stopped within 4 days of identifying lactic acidosis. Two of the 7 patients died despite stopping therapy. The lactate levels normalized in the 5 surviving patients after stopping this drug, but 1 of the patients had sequelae of blindness and disorientation.[Ref]
Renal
- Common (1% to 10%): Elevated BUN
- Uncommon (0.1% to 1%): Elevated creatinine, renal failure
- Frequency not reported: Exacerbation of renal failure, abnormal renal function, acute interstitial nephritis[Ref]
Dermatologic
- Common (1% to 10%): Rash, pruritus
- Uncommon (0.1% to 1%): Urticaria, dermatitis, diaphoresis
- Postmarketing reports: Bullous skin disorders (including severe cutaneous adverse reactions [SCAR] such as Stevens-Johnson syndrome and toxic epidermal necrolysis), angioedema, alopecia[Ref]
Genitourinary
- Common (1% to 10%): Vaginal candidiasis
- Uncommon (0.1% to 1%): Vaginitis, polyuria, vulvovaginal disorder[Ref]
Other
- Common (1% to 10%): Fungal infection, candidiasis, fever, localized pain, decreased total protein, decreased albumin, decreased sodium, decreased calcium, increased/decreased potassium, increased/decreased bicarbonate
- Uncommon (0.1% to 1%): Chills, fatigue, increased thirst, increased sodium, increased calcium, increased/decreased chloride
- Frequency not reported: Generalized edema[Ref]
Ocular
- Uncommon (0.1% to 1%): Blurred vision
- Rare (0.01% to 0.1%): Changes in visual field defect
- Frequency not reported: Partially irreversible bilateral optic neuritis
- Postmarketing reports: Optic neuropathy (sometimes progressing to loss of vision), optic neuritis, loss of vision, changes in visual acuity, changes in color vision[Ref]
Partially irreversible bilateral optic neuritis has been reported after 41 weeks of therapy.
Several cases of peripheral and/or optic neuropathy have been reported. The time from the onset of therapy to the first sign of optic neuropathy averaged 10 months (range: 1 to 48 months) in 6 patients with only optic neuropathy. The time to discontinuation of this drug due to optic neuropathy averaged 11 months (range: 1 to 56 months) after therapy initiation. This drug was stopped in 12 cases after the development of optic neuropathy; improvement or complete recovery was observed in all cases.[Ref]
Cardiovascular
- Common (1% to 10%): Hypertension
- Uncommon (0.1% to 1%): Arrhythmia (tachycardia), transient ischemic attacks, phlebitis, thrombophlebitis
- Frequency not reported: Increased and decreased blood pressure, supraventricular tachycardia[Ref]
Psychiatric
- Common (1% to 10%): Insomnia
- Frequency not reported: Confusion
Musculoskeletal
- Common (1% to 10%): Elevated creatine phosphokinase
Local
- Uncommon (0.1% to 1%): Injection site pain
Hypersensitivity
- Postmarketing reports: Anaphylaxis
Respiratory
- Frequency not reported: Interstitial pneumonia[Ref]
References
1. (2001) "Product Information. Zyvox (linezolid)." Pharmacia and Upjohn
2. Cerner Multum, Inc. "UK Summary of Product Characteristics."
3. Cerner Multum, Inc. "Australian Product Information."
4. Corallo CE, Paull AE (2002) "Linezolid-induced neuropathy." Med J Aust, 177, p. 332
5. Moise PA, Forrest A, Birmingham MC, Schentag JJ (2002) "The efficacy and safety of linezolid as treatment for Staphylococcus aureus infections in compassionate use patients who are intolerant of, or who have failed to respond to, vancomycin." J Antimicrob Chemother, 50, p. 1017-26
6. Lee E, Burger S, Shah J, et al. (2003) "Linezolid-associated toxic optic neuropathy: a report of 2 cases." Clin Infect Dis, 37, p. 1389-91
7. Legout L, Senneville E, Gomel JJ, Yazdanpanah Y, Mouton Y (2004) "Linezolid-induced neuropathy." Clin Infect Dis, 38, p. 767-8
8. Rho JP, Sia IG, Crum BA, Dekutoski MB, Trousdale RT (2004) "Linezolid-associated peripheral neuropathy." Mayo Clin Proc, 79, p. 927-30
9. Frippiat F, Derue G (2004) "Causal relationship between neuropathy and prolonged linezolid use." Clin Infect Dis, 39, p. 439
10. Ferry T, Ponceau B, Simon M, et al. (2005) "Possibly linezolid-induced peripheral and central neurotoxicity: report of four cases." Infection, 33, p. 151-4
11. Stein GE (2005) "Safety of newer parenteral antibiotics." Clin Infect Dis, 41 Suppl 5, S293-302
12. Morales-Molina JA, Mateu-de Antonio J, Marin-Casino M, Grau S (2005) "Linezolid-associated serotonin syndrome: what we can learn from cases reported so far." J Antimicrob Chemother, 56, p. 1176-8
13. Soriano A, Miro O, Mensa J (2005) "Mitochondrial toxicity associated with linezolid." N Engl J Med, 353, p. 2305-6
14. Thai XC, Bruno-Murtha LA (2006) "Bell's Palsy Associated with Linezolid Therapy: Case Report and Review of Neuropathic Adverse Events." Pharmacotherapy, 26, p. 1183-9
15. Senneville E, Legout L, Valette M, et al. (2006) "Effectiveness and tolerability of prolonged linezolid treatment for chronic osteomyelitis: A retrospective study." Clin Ther, 28, p. 1155-63
16. Plachouras D, Giannitsioti E, Athanassia S, et al. (2006) "No Effect of Pyridoxine on the Incidence of Myelosuppression during Prolonged Linezolid Treatment." Clin Infect Dis, 43, e89-e91
17. Strouse TB, Kerrihard TN, Forscher CA, Zakowski P (2006) "Serotonin syndrome precipitated by linezolid in a medically ill patient on duloxetine." J Clin Psychopharmacol, 26, p. 681-683
18. Steinberg M, Morin AK (2007) "Mild serotonin syndrome associated with concurrent linezolid and fluoxetine." Am J Health Syst Pharm, 64, p. 59-62
19. Garrabou G, Soriano A, Lopez S, et al. (2006) "Reversible inhibition of mitocondrial protein synthesis during linezolis-related hyperlactatemia." Antimicrob Agents Chemother, 51, p. 962-7
20. Strawn JR, Keck PE Jr, Caroff SN (2007) "Neuroleptic malignant syndrome." Am J Psychiatry, 164, p. 870-6
21. Narita M, Tsuji BT, Yu VL (2007) "Linezolid-associated peripheral and optic neuropathy, lactic acidosis, and serotonin syndrome." Pharmacotherapy, 27, p. 1189-97
22. Wiener M, Guo Y, Patel G, Fries BC (2007) "Lactic Acidosis after Treatment with Linezolid." Infection, 35, p. 278-81
23. Jodlowski TZ, Melnychuk I, Conry J (2007) "Linezolid for the treatment of Nocardia spp. infections (October)." Ann Pharmacother, 41, p. 1694-9
24. Das PK, Warkentin DI, Hewko R, Forrest DL (2008) "Serotonin syndrome after concomitant treatment with linezolid and meperidine." Clin Infect Dis, 46, p. 264-5
25. Scotton P, Fuser R, Torresan S, et al. (2008) "Early linezolid-associated lactic acidosis in a patient treated for tuberculous spondylodiscitis." Infection, 36, p. 387-8
26. Shneker BF, Baylin PD, Nakhla ME (2009) "Linezolid inducing complex partial status epilepticus in a patient with epilepsy." Neurology, 72, p. 378-9
27. Stalker DJ, Jungbluth GL, Hopkins NK, Batts DH (2003) "Pharmacokinetics and tolerance of single- and multiple-dose oral or intravenous linezolid, an oxazolidinone antibiotic, in healthy volunteers." J Antimicrob Chemother, 51, p. 1239-46
28. Matson KL, Miller SE (2003) "Tooth discoloration after treatment with linezolid." Pharmacotherapy, 23, p. 682-5
29. Zabel LT, Worm S (2005) "Linezolid Contributed to Clostridium difficile Colitis with Fatal Outcome." Infection, 33, p. 155-7
30. Falagas ME, Manta KG, Ntziora F, Vardakas KZ (2006) "Linezolid for the treatment of patients with endocarditis: a systematic review of the published evidence." J Antimicrob Chemother, 58, p. 273-80
31. Kohno S, Yamaguchi K, Aikawa N, et al. (2007) "Linezolid versus vancomycin for the treatment of infections caused by methicillin-resistant Staphylococcus aureus in Japan." J Antimicrob Chemother, 60, p. 1361-9
32. Refaat M, Hyle E, Malhotra R, Seidman D, Dey B (2008) "Linezolid-Induced Lingua Villosa Nigra." Am J Med, 121, e1
33. Kuter DJ, Tillotson GS (2001) "Hematologic effects of antimicrobials: focus on the oxazolidinone linezolid." Pharmacotherapy, 21, p. 1010-3
34. Lawyer MC, Lawyer EZ (2001) "Linezolid and reversible myelosuppression." JAMA, 286, p. 1974
35. Arellano FM (2001) "Linezolid and reversible myelosuppression." JAMA, 286, 1973-4; discussion 1974
36. Abena PA, Mathieux VG, Scheiff JM, Michaux LM, Vandercam BC (2001) "Linezolid and reversible myelosuppression." JAMA, 286, 1973; discussion 1974
37. Attassi K, Hershberger E, Alam R, Zervos MJ (2002) "Thrombocytopenia Associated with Linezolid Therapy." Clin Infect Dis, 34, p. 695-8
38. Waldrep TW, Skiest DJ (2002) "Linezolid-Induced anemia and thrombocytopenia." Pharmacotherapy, 22, p. 109-12
39. Orrick JJ, Johns T, Janelle J, Ramphal R (2002) "Thrombocytopenia secondary to linezolid administration: what is the risk?" Clin Infect Dis, 35, p. 348-9
40. Halpern M (2002) "Linezolid-induced pancytopenia." Clin Infect Dis, 35, p. 347-8
41. Gerson SL, Kaplan SL, Bruss JB, et al. (2002) "Hematologic Effects of Linezolid: Summary of Clinical Experience." Antimicrob Agents Chemother, 46, p. 2723-2726
42. Davis TM, Syed DA, Ilett KF, Barrett PH (2003) "Toxicity Related to Chloroquine Treatment of Resistant Vivax Malaria." Ann Pharmacother, 37, p. 526-529
43. McNamee WB Jr (2003) "Resumption of linezolid therapy after myelotoxicity." Clin Infect Dis, 37, p. 741-2
44. Nasraway SA, Shorr AF, Kuter DJ, O'Grady N, Le VH, Cammarata SK (2003) "Linezolid does not increase the risk of thrombocytopenia in patients with nosocomial pneumonia: comparative analysis of linezolid and vancomycin use." Clin Infect Dis, 37, p. 1609-16
45. Rao N, Ziran BH, Wagener MM, Santa ER, Yu VL (2004) "Similar hematologic effects of long-term linezolid and vancomycin therapy in a prospective observational study of patients with orthopedic infections." Clin Infect Dis, 38, p. 1058-64
46. Spellberg B, Yoo T, Bayer AS (2004) "Reversal of linezolid-associated cytopenias, but not peripheral neuropathy, by administration of vitamin B6." J Antimicrob Chemother, 54, p. 832-5
47. Senneville E, Legout L, Valette M, et al. (2004) "Risk factors for anaemia in patients on prolonged linezolid therapy for chronic osteomyelitis: a case-control study." J Antimicrob Chemother, 54, p. 798-802
48. Grau S, Morales-Molina JA, Mateu-de Antonio J, Marin-Casino M, Alvarez-Lerma F (2005) "Linezolid: low pre-treatment platelet values could increase the risk of thrombocytopenia." J Antimicrob Chemother, 56, p. 440-1
49. Wu VC, Wang YT, Wang CY, et al. (2006) "High frequency of linezolid-associated thrombocytopenia and anemia among patients with end-stage renal disease." Clin Infect Dis, 42, p. 66-72
50. Tattevin P, Camus C (2006) "What can we learn from studies comparing linezolid with vancomycin in neutropenic patients when vancomycin dosages are not optimized?" Clin Infect Dis, 42, 1813-4; author reply 1814-5
51. Akins RL, Haase MR, Levy EN (2006) "Pharmacokinetics of daptomycin in a critically ill adolescent with vancomycin-resistant enterococcal endocarditis." Pharmacotherapy, 26, p. 694-8
52. McNicholas S, Barber A, Corbett-Feeney G, Cormican M (2006) "Linezolid audit: similarities and contrasts with published experience." J Antimicrob Chemother, 57, p. 1008-9
53. John CC, Schreiber JR (2006) "Therapies and Vaccines for Emerging Bacterial Infections: Learning from Methicillin-resistant Staphylococcus aureus." Pediatr Clin North Am, 53, p. 699-713
54. Mateu de Antonio J, Grau S, Morales-Molina JA, Marin-Casino M (2006) "Thrombocytopenia and anemia associated with linezolid in patients with kidney failure." Clin Infect Dis, 42, 1500; author reply 1501
55. Faguer S, Kamar N, Fillola G, Guitard J, Rostaing L (2007) "Linezolid-related pancytopenia in organ-transplant patients: report of two cases." Infection, 35, p. 275-7
56. Youssef S, Hachem R, Chemaly RF, et al. (2008) "The role of vitamin B6 in the prevention of haematological toxic effects of linezolid in patients with cancer." J Antimicrob Chemother, 61, p. 421-4
57. (2009) "Drugs for MRSA with reduced susceptibility to vancomycin." Med Lett Drugs Ther, 51, 36; quiz 37
58. Apodaca AA, Rakita RM (2003) "Linezolid-induced lactic acidosis." N Engl J Med, 348, p. 86-7
59. Meyer B, Thalhammer F (2006) "Linezolid and continuous venovenous hemofiltration." Clin Infect Dis, 42, 435-6; author reply 437-8
60. Marino EA, Blanchard E, Samuel R, Gallagher J (2009) "Acute interstitial nephritis associated with linezolid." Ann Pharmacother, 43, p. 1728
61. Frippiat F, Bergiers C, Michel C, Dujardin JP, Derue G (2004) "Severe bilateral optic neuritis associated with prolonged linezolid therapy." J Antimicrob Chemother, 53, p. 1114-5
62. Saijo T, Hayashi K, Yamada H, Wakakura M (2005) "Linezolid-induced Optic Neuropathy." Am J Ophthalmol, 139, p. 1114-6
63. Joshi L, Taylor SR, Large O, Yacoub S, Lightman S (2009) "A case of optic neuropathy after short-term linezolid use in a patient with acute lymphocytic leukemia." Clin Infect Dis, 48, e73-4
64. Cleveland KO, Gelfand MS (2009) "Optic neuropathy following linezolid use in a patient with acute lymphocytic leukemia." Clin Infect Dis, 49, 645-6; author reply 646
Frequently asked questions
More about linezolid
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (32)
- Drug images
- Dosage information
- During pregnancy
- Drug class: oxazolidinone antibiotics
- Breastfeeding
- En español
Patient resources
- Linezolid oral/injection drug information
- Linezolid (Intravenous) (Advanced Reading)
- Linezolid (Oral) (Advanced Reading)
- Linezolid Tablets
- Linezolid Injection
- Linezolid Suspension
Other brands
Professional resources
- Linezolid monograph
- Linezolid Injection (FDA)
- Linezolid Oral Suspension (FDA)
- Linezolid Tablets (FDA)
Other brands
Related treatment guides
Further information
Linezolid side effects can vary depending on the individual. Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Note: Medication side effects may be underreported. If you are experiencing side effects that are not listed, submit a report to the FDA by following this guide.