Vigabatrin (Monograph)
Brand names: Sabril, Vigadrone, Vigafyde™, Vigpoder™
Drug class: GABA-mediated Anticonvulsants
Warning
Risk Evaluation and Mitigation Strategy (REMS):
FDA approved a REMS for vigabatrin to ensure that the benefits outweigh the risks. The REMS may apply to one or more preparations of vigabatrin and consists of the following: elements to assure safe use and implementation system. See https://www.accessdata.fda.gov/scripts/cder/rems/.
Warning
- Permanent Vision Loss
-
Vigabatrin can cause permanent bilateral concentric visual field constriction, including tunnel vision that may result in disability. In some cases, vigabatrin also can damage the central retina and reduce visual acuity.
-
Risk of vision loss increases with increasing dosage and cumulative exposure; however, no dosage or exposure is known to be without risk.
-
Risk of new and worsening vision loss continues as long as vigabatrin is used and possibly after discontinuance.
-
Baseline and periodic vision assessment recommended in patients receiving vigabatrin. However, such vision assessment cannot always prevent vision damage.
-
Distribution of vigabatrin is restricted.
Introduction
Anticonvulsant; irreversible inhibitor of GABA transaminase (GABA-T).
Uses for Vigabatrin
Refractory Complex Partial Seizures
Management (in combination with other anticonvulsants) of refractory complex partial seizures (CPS) in adults and pediatric patients ≥2 years of age who have not responded adequately to several alternative treatments.
Use only in patients in whom potential benefits outweigh risk of vision loss.
Recommended for treatment-resistant focal epilepsy in adults ; do not use as first-line therapy.
Infantile Spasms
Management (as monotherapy) of infantile spasms (IS; also known as West's syndrome) in pediatric patients 1 month–2 years of age for whom potential benefits outweigh risk of vision loss.
Designated an orphan drug by FDA for this use.
Duration of therapy was evaluated in a Canadian Pediatric Epilepsy Network (CPEN) study; 38 out of 68 infants with IS who responded to vigabatrin continued to receive the drug for a total of 6 months and were followed for an additional 18 months after drug discontinuance. Post hoc analysis indicated no observed IS recurrence in any of the infants.
Guidelines from the American Academy of Neurology (published in 2012, reaffirmed in 2021, retired in 2024) recommend low-dose adrenocorticotropic hormone (ACTH) or vigabatrin for short-term treatment of IS. ACTH is preferred over vigabatrin, except in the setting of tuberous sclerosis complex.
Vigabatrin Dosage and Administration
General
Pretreatment Screening
-
In patients receiving vigabatrin, vision testing is recommended at baseline (no later than 4 weeks after start of therapy).
Patient Monitoring
-
In patients receiving vigabatrin, vision testing is recommended at least every 3 months during treatment, and about 3–6 months following cessation of therapy.
Dispensing and Administration Precautions
- Handling and Disposal
-
Vigabatrin has been identified as a potential hazard by the National Institute for Occupational Safety and Health (NIOSH); use appropriate precautions when handling.
-
If switching between other vigabatrin products and the 100 mg/mL oral solution (Vigafyde™), verify that the correct volume for the correct dosage is prescribed, dispensed, and administered. Compared to vigabatrin tablets and powder for oral solution, the 100 mg/mL oral solution is more concentrated and requires a smaller volume to obtain the same dosage.
REMS
-
Because of the risk of permanent vision loss, vigabatrin is only available through a restricted distribution program called the Vigabatrin REMS Program.
-
The vigabatrin REMS program requires clinicians to be certified by enrolling in the program and agreeing to counsel patients on the risk of vision loss and the need for periodic vision testing during vigabatrin therapy.
-
Pharmacies must be certified and must only dispense vigabatrin to patients who are authorized to receive the drug; any event suggestive of vision loss must be reported to the manufacturer.
-
For further information on the restricted distribution program for vigabatrin, contact the vigabatrin REMS program at 866-244-8175 or consult the manufacturer’s website ([Web]).
Administration
Oral Administration
Administer orally (as powder for oral solution (50 mg/mL) or oral solution (100 mg/mL) for IS and as tablets or powder for oral solution for refractory CPS without regard to meals.
Reconstitution of Powder for Oral Solution
Review and discuss the vigabatrin medication guide and instructions on proper reconstitution, administration, and dosing procedures with patients or caregivers and confirm their understanding.
Use only water to dissolve the powder; mix thoroughly with a small spoon or other clean utensil until powder completely dissolves and solution is clear.
Empty entire contents of the appropriate number of packets (500 mg/packet) into a clean cup; dissolve with 10 mL of cold or room-temperature water per packet to yield a final concentration of 50 mg/mL.
For doses ≤500 mg, dissolve 1 packet with 10 mL of water; for doses of 501 mg–1 g, dissolve 2 packets with 20 mL of water; and for doses of 1–1.5 g, dissolve 3 packets with 30 mL of water. Discard resulting solution if not clear (or free of particles) and colorless.
Depending on the dose to be administered, use a 3-mL or 10-mL oral syringe supplied by the pharmacy to withdraw the specific volume of solution that will provide the appropriate dose and discard any remaining solution. Administer dose immediately following preparation.
Dosage
Plasma vigabatrin concentrations not directly correlated with efficacy; therapeutic drug monitoring is not useful.
Use the lowest dosage and shortest duration of therapy consistent with clinical objectives.
Dosage regimen depends on the indication, age group, weight, and dosage form (tablets or powder for oral solution).
Pediatric Patients
Adjunctive Therapy of Refractory Complex Partial Seizures
Oral
Pediatric patients ≥17 years of age: May receive adult dosages. Initially, 1 g daily (given as 500 mg twice daily). May increase total daily dosage in 500-mg increments at weekly intervals up to the recommended dosage of 3 g daily (given as 1.5 g twice daily) depending on patient response.
Pediatric patients 2–16 years of age: dosage based on body weight; administer as 2 divided doses. (See Table 1.) May increase total daily dosage at weekly intervals up to the recommended dosage, depending on response. Patients 2–16 years of age weighing >60 kg should be dosed according to adult recommendations.
Patients weighing >60 kg should be dosed according to adult recommendations.
Administered in 2 divided doses.
Maintenance dose is based on 3000 mg per day adult-equivalent dose.
|
Weight (kg) |
Starting Dosage (Total Daily Dose) |
Maintenance Dosage (Total Daily Dose) |
|---|---|---|
|
10–15 |
350 mg daily |
1050 mg daily |
|
>15–20 |
450 mg daily |
1300 mg daily |
|
>20–25 |
500 mg daily |
1500 mg daily |
|
>25–60 |
500 mg daily |
2000 mg daily |
Periodically reassess patient response and continued need for therapy. If substantial clinical benefit not observed within 3 months of therapy initiation, withdraw therapy. If treatment failure is evident earlier, discontinue vigabatrin at that time.
Reduce dosage gradually if discontinuing therapy. In a controlled study in pediatric patients with complex partial seizures, daily dosage was tapered by one-third every week for 3 weeks.
Monotherapy of Infantile Spasms
Oral
Children 1 month–2 years of age: Initially, 50 mg/kg daily, administered in 2 divided doses (given as 25 mg/kg twice daily). May increase dosage in increments of 25–50 mg/kg daily every 3 days up to a maximum of 150 mg/kg daily (given as 75 mg/kg twice daily).
The volume of solution required per dose varies depending on the specific product used; consult the product prescribing information for details.
|
Weight (kg) |
Starting Dosage (50 mg/kg daily) |
Maximum Dosage (150 mg/kg daily) |
|---|---|---|
|
3 |
75 mg twice daily |
225 mg twice daily |
|
4 |
100 mg twice daily |
300 mg twice daily |
|
5 |
125 mg twice daily |
375 mg twice daily |
|
6 |
150 mg twice daily |
450 mg twice daily |
|
7 |
175 mg twice daily |
525 mg twice daily |
|
8 |
200 mg twice daily |
600 mg twice daily |
|
9 |
225 mg twice daily |
675 mg twice daily |
|
10 |
250 mg twice daily |
750 mg twice daily |
|
11 |
275 mg twice daily |
825 mg twice daily |
|
12 |
300 mg twice daily |
900 mg twice daily |
|
13 |
325 mg twice daily |
975 mg twice daily |
|
14 |
350 mg twice daily |
1050 mg twice daily |
|
15 |
375 mg twice daily |
1125 mg twice daily |
|
16 |
400 mg twice daily |
1200 mg twice daily |
Periodically reassess patient response and continued need for therapy. If substantial clinical benefit not observed within 2–4 weeks of therapy initiation, withdraw therapy. If treatment failure is evident earlier, discontinue vigabatrin at that time.
Reduce dosage gradually if discontinuing therapy. In a controlled study in patients with IS, vigabatrin was tapered at a rate of 25–50 mg/kg daily every 3–4 days.
Adults
Adjunctive Therapy of Refractory Complex Partial Seizures
Oral
Initially, 1 g daily (given as 500 mg twice daily). May increase total daily dosage in 500-mg increments at weekly intervals up to the recommended dosage of 3 g daily (given as 1.5 g twice daily) depending on patient response.
Dosage of 6 g daily was not more effective than 3 g daily and was associated with increased adverse effects.
Periodically reassess patient response and continued need for therapy. If substantial clinical benefit not observed within 3 months of therapy initiation, withdraw therapy. If treatment failure is evident earlier, discontinue vigabatrin at that time.
Reduce dosage gradually if discontinuing therapy. In clinical studies in adults, daily dosage was tapered by 1 g weekly.
Special Populations
Hepatic Impairment
No specific dosage recommendations at this time.
Renal Impairment
Reduce dosage in adults and pediatric patients ≥2 years of age based on severity of renal impairment .
|
Clcr (mL/min) |
Adjusted Dosage Regimen |
|---|---|
|
>50–80 (mild) |
Decrease dosage by 25% |
|
>30–50 (moderate) |
Decrease dosage by 50% |
|
>10–30 (severe) |
Decrease dosage by 75% |
In pediatric patients 2 to <12 years of age, use the following formula to estimate Clcr:
Clcr = [K × height (in cm)] / serum creatinine (in mg/dL)
K for female child (<12 years) = 0.55
K for male child (<12 years) = 0.70
In pediatric patients ≥12 years of age and adults, use the following formula to estimate Clcr:
Clcr male = [(140 - age) × weight (in kg)] / [72 × serum creatinine (in mg/dL)] Clcr female = 0.85 × Clcr male
Information about how to adjust the dosage of vigabatrin in infants with renal impairment is unavailable.
Manufacturer does not provide specific dosage recommendations for patients undergoing hemodialysis.
Geriatric Patients
Carefully select dosage because of possible decreased renal function. Consider adjusting dosage or frequency of administration; may respond to a lower maintenance dosage than younger adults.
Vigabatrin 100 mg/mL oral solution is not approved for use in adults.
Cautions for Vigabatrin
Contraindications
-
None.
Warnings/Precautions
Warnings
Permanent Vision Loss
Risk of visual field defects, including permanent vision loss; may occur at any time after beginning therapy and will not improve after discontinuance. (See Boxed Warning.) In adults, manifestations include tunnel vision to within 10 degrees of visual fixation, which can lead to disability; in some cases, central retinal damage and decreased visual acuity may occur. Although visual field defects observed in pediatric patients, frequency and extent of vision loss are poorly characterized.
Monitoring of vision by an ophthalmic professional recommended at baseline (≤4 weeks after start of therapy), at least every 3 months during treatment, and about 3–6 months following cessation of therapy. Because vision testing in infants is difficult, vision loss may not be detected until it is severe.
If a patient cannot undergo vision testing, clinician may continue treatment according to clinical judgment after appropriate patient counseling.
Unless benefits clearly outweigh risks, do not use in patients with, or at high risk of, other types of irreversible vision loss. Unless benefits clearly outweigh risks, avoid concurrent use with other drugs associated with serious adverse ophthalmic effects (e.g., retinopathy, glaucoma).
Periodically reassess patient response to and continued need for therapy. Discontinue vigabatrin if substantial clinical benefit not evident within 2–4 weeks or within 3 months following therapy initiation in patients with IS or refractory CPS, respectively. If treatment failure becomes obvious earlier, discontinue drug at that time.
It is expected that, even with frequent vision monitoring, some vigabatrin-treated patients will develop severe vision loss. If vision loss is documented, consider drug discontinuance, balancing the benefit and risk of continued therapy.
Other Warnings and Precautions
Magnetic Resonance Imaging Abnormalities in Infants
Abnormal magnetic resonance imaging (MRI) changes characterized by increased T2 signal and restricted diffusion in a symmetric pattern involving deep gray matter areas of the brain reported in some infants ; these specific abnormalities not observed in older pediatric patients (≥3 years of age) and adults.
MRI abnormalities generally are transient, resolve upon drug discontinuance, and may be dose-dependent. In a few patients, the abnormalities resolved despite continued therapy. Coincident motor abnormalities reported in some infants; however, causal relationship to drug not established.
Manufacturer states that routine MRI surveillance is unnecessary in adults.
Neurotoxicity
Intramyelinic edema (IME) reported upon postmortem examination of infants treated with vigabatrin for IS. Neuropathologic and neurobehavioral changes observed in animals receiving vigabatrin. Neurotoxicity (brain histopathology, neurobehavioral abnormalities) observed in animals exposed to vigabatrin during late gestation, neonatal, and/or juvenile periods of development.
Suicidal Behavior and Ideation
Increased risk of suicidality (suicidal ideation or behavior) observed in an analysis of studies using various anticonvulsants in patients with epilepsy, psychiatric disorders (e.g., bipolar disorder, depression, anxiety), and other conditions (e.g., migraine, neuropathic pain); risk in patients receiving anticonvulsants (0.43%) was approximately twice that in patients receiving placebo (0.24%). Vigabatrin 100 mg/mL oral solution is approved for patients 1 month to 2 years of age, and is not approved for use in adolescents and adults; anticonvulsants increase the risk of suicidal thoughts or behavior in adolescents and adults. Increased suicidality risk was observed ≥1 week after initiation of anticonvulsant therapy and continued through 24 weeks. Risk was higher for patients with epilepsy compared with those receiving anticonvulsants for other conditions.
Closely monitor all patients currently receiving or beginning anticonvulsant therapy for changes in behavior that may indicate emergence or worsening of suicidal thoughts or behavior or depression.
Balance risk of suicidality with risk of untreated illness. Epilepsy and other illnesses treated with anticonvulsants are themselves associated with morbidity and mortality and an increased risk of suicidality. If suicidal thoughts or behavior emerge during anticonvulsant therapy, consider whether these symptoms may be related to the illness itself.
Withdrawal of Antiepileptic Drugs
Abrupt withdrawal of anticonvulsants may result in increased seizure frequency in patients with seizure disorders. When discontinuing therapy, withdraw vigabatrin gradually. However, if discontinuance is necessary because of serious adverse effects, may consider prompt withdrawal of the drug.
Anemia
Anemia and/or potentially clinically important hematology changes involving hemoglobin, hematocrit, and/or RBC indices reported.
Somnolence and Fatigue
Somnolence and fatigue reported in adult and pediatric patients, sometimes requiring discontinuance.
May impair mental and/or physical abilities required to perform potentially hazardous tasks such as driving or operating machinery.
Peripheral Neuropathy
Peripheral neuropathy symptoms reported in adults. Initial manifestations include numbness or tingling in the toes or feet, signs of reduced distal lower limb vibration or position sensation, and/or progressive loss of reflexes starting at the ankles.
Studies in pediatric patients not adequately designed to assess peripheral neuropathy symptoms; however, incidence of symptoms in controlled pediatric studies appeared similar with vigabatrin and placebo.
Weight Gain
Weight gain reported in adult and pediatric patients, but long-term effects of such weight gain not known. Weight gain not apparently related to occurrence of edema
Edema
Vigabatrin causes edema in adults. Pediatric clinical studies not designed to assess edema; however, observed incidence of edema appeared similar with vigabatrin and placebo.
No apparent association between edema and adverse cardiovascular effects (e.g., hypertension, CHF) in adults. Edema not associated with laboratory changes suggesting deterioration of renal or hepatic function.
Specific Populations
Pregnancy
No adequate data available on the developmental risk of vigabatrin when used in pregnancy. Limited data from case reports and cohort studies in pregnant patients have not established a drug-associated risk; however, animal data suggest a possibility of fetal harm when used in pregnancy.
North American Antiepileptic Drug (NAAED) Pregnancy Registry (for patients) at 888-233-2334 or [Web].
Lactation
Distributed into milk; effects on the breast-fed infant and milk production not known. Manufacturer recommends against breast-feeding while taking vigabatrin. If a decision is made to continue breastfeeding during therapy; monitor the nursing infant for potential adverse effects.
Pediatric Use
Safety and efficacy of tablets and powder for oral solution for adjunctive therapy of refractory CPS established in pediatric patients 2–16 years of age. Indicated for such use in pediatric patients ≥2 years of age who have not responded adequately to several alternative treatments. Adverse effects in this pediatric population are similar to those observed in adults.
Safety and efficacy of vigabatrin 100 mg/mL oral solution not established in any population for the treatment of refractory CPS. Safety and efficacy of tablets and powder for solution for treatment of CPS in pediatric patients <2 years of age also not established.
All formulations are indicated as monotherapy in pediatric patients 1 month–2 years of age with IS for whom potential benefits outweigh the risk of vision loss; safety and efficacy for treating IS not established outside this age group.
Abnormal MRI signal changes and IME observed in some infants and young children receiving vigabatrin for IS.
Geriatric Use
Insufficient experience in patients ≥65 years of age to determine whether geriatric patients respond differently than younger adults.
Moderate to severe sedation and confusion reported in several patients >65 years of age with reduced renal function (Clcr <50 mL/minute). Other reported clinical experience has not identified differences in response.
Reduced renal function more likely in geriatric patients. Carefully select dosage; renal function monitoring may be useful.
Hepatic Impairment
Pharmacokinetics in patients with hepatic impairment not evaluated.
Suppresses ALT and AST activity.
Renal Impairment
Decreased clearance; use with caution. Adjust dosage in pediatric patients ≥2 years of age and adults and monitor for dose-related adverse effects. Information about how to adjust vigabatrin dosage in infants is not available.
Race
Race-related pharmacokinetic differences not specifically evaluated. Limited data suggest that renal clearance may be lower in Japanese than in Caucasian populations.
Common Adverse Effects
Causes permanent vision damage in a high percentage of patients.
Adolescents and adults (>16 years of age) with refractory CPS (incidence ≥5% over placebo): Blurred vision, somnolence, dizziness, abnormal coordination, tremor, fatigue.
Pediatric patients 3–16 years of age with refractory CPS (incidence ≥5% over placebo): Weight gain.
Pediatric patients with IS (adverse effects occurring in >5% of vigabatrin-treated patients and more frequent than in placebo recipients): Somnolence, bronchitis, ear infection, acute otitis media.
Drug Interactions
Not extensively metabolized by hepatic CYP isoenzymes.
Induces CYP2C9; does not appear to induce other hepatic CYP isoenzymes.
Drugs Affecting or Metabolized by Hepatic Microsomal Enzymes
Substrates of CYP2C9: potential pharmacokinetic interaction (decreased plasma substrate concentrations).
Substrates of other CYP isoenzymes: clinically important interactions unlikely.
Drugs associated with Serious Adverse Ophthalmic Effects
Avoid concurrent use with other drugs associated with serious adverse ophthalmic effects (e.g., retinopathy, glaucoma) unless benefits clearly outweigh risks.
Specific Drugs and Laboratory Tests
|
Drug or Test |
Interaction |
Comments |
|---|---|---|
|
Alcohol |
Pharmacokinetic interaction not observed; |
|
|
Carbamazepine |
No clinically significant pharmacokinetic interactions expected with concomitant use |
|
|
Clonazepam |
Increased peak plasma concentrations and decreased time to peak concentration of clonazepam; no substantial change in plasma concentrations of vigabatrin |
|
|
Clorazepate |
No apparent effect on vigabatrin plasma concentrations |
|
|
Contraceptives, oral |
No substantial effect on CYP3A4-mediated metabolism of ethinyl estradiol/levonorgestrel; unlikely to affect efficacy of steroid oral contraceptives Pharmacokinetics of vigabatrin not substantially affected |
|
|
Phenobarbital |
Clinically important pharmacokinetic interaction unlikely |
|
|
Phenytoin |
Moderate decrease in total plasma phenytoin concentrations (by 16–20%), probably due to induction of CYP2C9 |
Routine phenytoin dosage adjustment not required; adjust dosage if clinically indicated |
|
Primidone |
Clinically important pharmacokinetic interaction unlikely |
|
|
Tests for ALT and AST activity |
Possible suppression of ALT and AST activity |
Consider that these tests, particularly ALT, may not be useful for detection of early hepatic injury |
|
Tests for amino acids in urine |
Possible increased amino acid concentrations in urine; may result in false positive tests for certain rare genetic metabolic disorders (e.g., alpha aminoadipic aciduria) |
|
|
Valproic acid |
Clinically important pharmacokinetic Interaction unlikely |
Vigabatrin Pharmacokinetics
Absorption
Bioavailability
Rapidly and essentially completely absorbed following oral administration.
Peak plasma concentrations generally occur within approximately 2.5 hours in infants (5 months–2 years of age) and 1 hour in children and adolescents (3–16 years of age) and adults following oral administration.
Little accumulation occurs with multiple dosing in adult and pediatric patients.
Food
Food decreases peak plasma concentrations by 33% and increases time to peak concentrations, but does not affect systemic exposure.
Special Populations
Systemic exposure increased by approximately 30%, 2-fold, and 4.5-fold in adults with mild, moderate, and severe renal impairment, respectively.
Distribution
Extent
Widely distributed.
Distributed into milk,
Plasma Protein Binding
Not appreciably bound to plasma proteins.
Elimination
Metabolism
Not extensively metabolized.
Elimination Route
Principally excreted in urine (95% of orally administered dose recovered over 72 hours), with unchanged drug accounting for 80% of the recovered dose.
Half-life
Adults: About 10.5 hours.
Pediatric patients 10–16 years of age: About 9.5 hours.
Pediatric patients 3–9 years of age: about 6.8 hours.
Pediatric patients 5 months–2 years of age: About 5.7 hours.
Special Populations
In adults with mild, moderate, or severe renal impairment, terminal half-life is increased by 55%, 2-fold, or 3.5-fold, respectively.
Effect of hemodialysis on clearance not adequately studied. In case reports, hemodialysis reduced plasma concentrations by 40–60%.
Pharmacokinetics in patients with hepatic impairment not evaluated.
In individuals >65 years of age, renal clearance is reduced by 36% compared with younger individuals.
Stability
Storage
Oral
Oral Solution
20–25°C (excursions permitted to 15–30°C). After opening, store between 2–30°C; discard any unused medication within 90 days of first opening.
Powder for Oral Solution
20–25°C.
Tablets
20–25°C.
Actions
-
Structural analog of GABA, the primary inhibitory neurotransmitter in the CNS.
-
Exact mechanism of antiseizure effect unknown; thought to be related to preferential and irreversible inhibition of GABA-T, the enzyme responsible for the degradation of GABA, and the resultant increase in GABA concentrations in the central nervous (CNS).
-
Following oral administration, CNS and blood concentrations of GABA increase in a dose-related matter, but there is no direct correlation between plasma concentrations and drug efficacy.
-
Highly selective and specific for GABA-T; does not affect other enzymatic pathways in the GABA system.
-
Commercially available as a racemic mixture of 2 enantiomers; the S enantiomer is pharmacologically active and the R enantiomer is inactive.
Advice to Patients
-
Advise patients or caregivers to read the manufacturer's patient information (medication guide).
-
Inform patients and caregivers of the risk of permanent vision loss, particularly loss of peripheral vision, from vigabatrin, and the need for monitoring vision. Monitoring of vision, including assessment of visual fields and visual acuity, is recommended at baseline (no later than 4 weeks after starting vigabatrin), at least every 3 months while on therapy, and about 3–6 months after discontinuation of therapy. In patients for whom vision testing is not possible, treatment may continue without recommended testing according to clinical judgment with appropriate patient or caregiver counseling. Inform patients or caregivers that if baseline or subsequent vision is not normal, vigabatrin should only be used if the benefits of vigabatrin treatment clearly outweigh the risks of additional vision loss. Advise patients and caregivers that vision testing may be insensitive and may not detect vision loss before it is severe. Also advise patients and caregivers that if vision loss occurs, such loss is irreversible. Ensure that both of these points are understood by patients and caregivers. Inform patients and caregivers that if changes in vision are suspected, they should notify their physician immediately.
-
Stress importance of taking vigabatrin only as prescribed. When using the powder for oral solution, confirm that the patient/caregiver understand instructions for reconstitution of vigabatrin powder for oral solution and administration of the correct dosage.
-
If a patient is switching from vigabatrin powder for oral solution to vigabatrin oral solution , inform the caregiver that vigabatrin oral solution is more concentrated (100 mg/mL) compared to reconstituted solutions of vigabatrin powder for oral solution (50 mg/mL), and the volume of solution that should be given will be lower than previously prescribed. Advise patients to stop using other products that contain vigabatrin.
-
Physicians should confirm caregiver(s) understand how to measure and administer the correct dose of vigabatrin oral solution. Instruct caregivers vigabatrin 100 mg/mL oral solution should not be diluted prior to dosing. Advise caregivers to measure vigabatrin oral solution with the syringe provided by the pharmacy. A household teaspoon is not an accurate measuring device. Advise the caregiver to discard any remaining vigabatrin oral solution 90 days after first opening.
-
Inform patients that vigabatrin is only available through a restricted program called the Vigabatrin REMS Program. Inform patients/caregivers that they must be enrolled in the program, and that vigabatrin is only available through pharmacies that are enrolled in the program.
-
Inform caregivers about the possibility that infants receiving vigabatrin may develop abnormal MRI signal changes of unknown clinical importance.
-
Counsel patients, their caregiver(s), and families that antiepileptic drugs, including vigabatrin, may increase the risk of suicidal thoughts and behavior. Also advise patients/caregivers of the need to be alert for the emergence or worsening of symptoms of depression, any unusual changes in mood or behavior, or the emergence of suicidal thoughts, behavior, or thoughts of self-harm. Behaviors of concern should be reported immediately to healthcare providers.
-
Advise patients/caregivers that vigabatrin should not be suddenly stopped and should be gradually withdrawn.
-
Inform clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements, as well as any concomitant illness (e.g., kidney disease, vision problems, depression or other mood disorders) or family history of suicidality or bipolar disorder.
-
Advise patients to inform clinicians if they are or plan to become pregnant or plan to breast-feed. Advise pregnant females and females of child-bearing potential that use of vigabatrin during pregnancy can cause fetal harm, which may occur early in pregnancy before many females know they are pregnant. Advise patients there is a pregnancy exposure registry that collects information about the safety of antiepileptic drugs during pregnancy. Counsel patients vigabatrin is excreted in breast milk. Because of the potential for serious adverse reactions in nursing infants from vigabatrin, breast-feeding is not recommended. If a decision is made to breast-feed, nursing mothers should be counseled to observe the infant for signs of vision loss, sedation, and poor sucking.
-
Inform patients/caregivers of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
Distribution of vigabatrin is restricted.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Powder for oral solution |
500 mg |
Sabril (available in packets) |
Lundbeck |
|
500 mg |
Vigadrone (available in packets) |
|||
|
500 mg |
Vigpoder™ (available in packets) |
|||
|
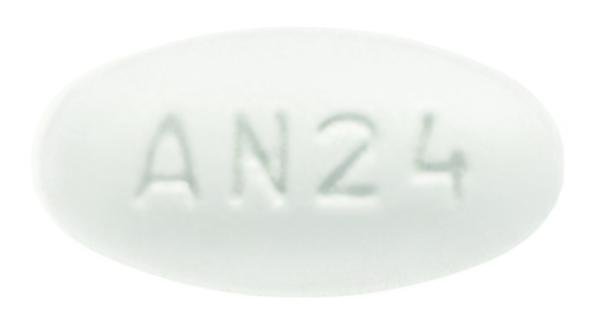
Tablets, film-coated |
500 mg |
Sabril (scored) |
Lundbeck |
|
|
500 mg |
Vigadrone (scored) |
|||
|
Oral Solution |
100 mg/mL |
Vigafyde™ |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions May 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
Frequently asked questions
More about vigabatrin
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (2)
- Drug images
- Latest FDA alerts (1)
- Side effects
- Dosage information
- During pregnancy
- Drug class: gamma-aminobutyric acid analogs
- Breastfeeding
- En español
Patient resources
Professional resources
Other brands
Sabril, Vigpoder, Vigafyde, Vigadrone