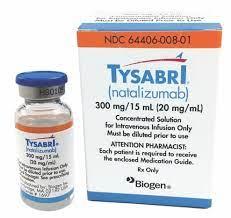
Tysabri
Generic name: natalizumab [ nat-ta-LIZ-yoo-mab ]
Drug class: Selective immunosuppressants
What is Tysabri?
Tysabri is a monoclonal antibody that affects the actions of the body's immune system. Monoclonal antibodies are made to target and destroy only certain cells in the body. This may help to protect healthy cells from damage.
Tysabri is used to treat relapsing forms of multiple sclerosis in adults (including clinically isolated syndrome, relapsing-remitting disease, and active secondary progressive disease).
Tysabri is also used to treat moderate to severe Crohn's disease in adults. It is usually given after other medicines did not work or have stopped working.
Warnings
Tysabri may cause a serious brain infection that can lead to disability or death, especially if you use natalizumab longer than 2 years, if you've used an immunosuppressant drug before, or if you've been infected with John Cunningham Virus (JCV). Call your doctor right away if you have a sudden fever, severe headache, confusion, memory problems, vision changes, eye pain, weakness on one side of your body, or problems with using your arms or legs. These symptoms may start gradually and get worse quickly.
Call your doctor right away if you have any change in your mental state, decreased vision, weakness on one side of your body, or problems with speech or walking. These symptoms may start gradually and get worse quickly.
Call your doctor at once if you develop any symptoms of liver damage, such as nausea, upper stomach pain, itching, loss of appetite, dark urine, clay-colored stools, or jaundice (yellowing of the skin or eyes).
You should also call your doctor right away if you develop any signs of infection such as fever, chills, sore throat, cough, stuffy nose, redness, pain, swelling, or painful urination.
Before taking this medicine
Tysabri may cause a serious brain infection called progressive multifocal leukoencephalopathy (PML). This infection may be more likely if you use Tysabri for longer than 2 years, if you have used an immunosuppressant drug in the past, or if you have been infected with John Cunningham Virus (JCV).
You should not receive Tysabri if you are allergic to natalizumab, or if you have ever had PML.
Tysabri is available only from a certified pharmacy under a special program called the TOUCH Prescribing Program. You must be registered in the program and understand the risks and benefits of taking this medicine.
To make sure this medicine is safe for you, tell your doctor if you have ever had:
-
fever, or an active infection;
-
herpes or shingles;
-
leukemia or lymphoma;
-
HIV, AIDS, or other condition that can weaken your immune system;
-
liver disease;
-
an organ transplant; or
-
hives, itching, or trouble breathing after a dose of Tysabri.
It is not known whether Tysabri will harm an unborn baby. Tell your doctor if you are pregnant or plan to become pregnant.
It may not be safe to breastfeed while using Tysabri. Ask your doctor about any risk.
Tysabri is not approved for use by anyone younger than 18 years old.
How is Tysabri given?
Tysabri given as an IV infusion into a vein, usually once every 4 weeks. A healthcare provider will give you this injection. Tysabri is usually given once every 4 weeks.
Tysabri must be given slowly and the IV infusion can take at least 1 hour to complete. You will be watched closely for at least 1 hour after receiving the infusion, to make sure you do not have an allergic reaction to the medication. An allergic reaction can occur up to 2 hours or longer after your infusion.
Before your first dose, your doctor may recommend an MRI to make sure you do not have any signs of a brain infection.
Tysabri can weaken your immune system. You may get infections more easily, even serious or fatal infections. You will need frequent blood tests. You may also need a brain scan or spinal tap (lumbar puncture) if you develop signs of a brain infection.
It is extremely important that your doctor check you every 3 to 6 months for signs of serious infection. Your doctor may also want to check you for several weeks after you stop using this medicine.
Tell any doctor who treats you that you are using Tysabri.
Dosing information
Usual Adult Dose of Tysabri for Multiple Sclerosis:
300 mg IV over 1 hour once every 4 weeks
Comments:
-Only prescribers registered in the MS TOUCH (R) Prescribing Program may prescribe this drug for multiple sclerosis.
-Patients should be observed during the infusion and for one hour after the infusion is complete.
Use: Multiple Sclerosis (MS): As monotherapy for the treatment of patients with relapsing forms of multiple sclerosis
Usual Adult Dose of Tysabri for Crohn's Disease - Maintenance:
300 mg IV over 1 hour once every 4 weeks
Comments:
-Only prescribers registered in the CD TOUCH (R) Prescribing Program may prescribe this drug for Crohn's disease.
-This drug should not be used with concomitant immunosuppressants (e.g., 6-mercaptopurine, azathioprine, cyclosporine, methotrexate) or concomitant inhibitors of TNF-alpha.
-Aminosalicylates may be continued during treatment with this drug.
-If the patient has not experienced therapeutic benefit by 12 weeks of induction therapy, this drug should be discontinued.
-For patients who start this drug while on chronic oral corticosteroids, steroid tapering should commence as soon as a therapeutic benefit of this drug has occurred; if the patient cannot be tapered off of oral corticosteroids within 6 months of starting this drug, then this drug should be discontinued.
-Other than the initial 6 month taper, prescribers should consider discontinuing this drug for patients who require additional steroid use that exceeds 3 months in a calendar year to control their Crohn's disease.
-Patients should be observed during the infusion and for one hour after the infusion is complete.
Use: Crohn's Disease (CD): For inducing and maintaining clinical response and remission in adult patients with moderately to severely active Crohn's disease with evidence of inflammation who have had an inadequate response to, or are unable to tolerate conventional CD therapies and inhibitors of TNF-alpha
What happens if I miss a dose?
Call your doctor for instructions if you miss an appointment for your Tysabri injection.
What happens if I overdose?
Since this medicine is given by a healthcare professional in a medical setting, an overdose is unlikely to occur.
What should I avoid while receiving Tysabri?
Avoid being near people who are sick or have infections. Tell your doctor at once if you develop signs of infection.
Tysabri side effects
Get emergency medical help if you have signs of an allergic reaction to Tysabri: hives, rash; wheezing, difficult breathing; swelling of your face, lips, tongue, or throat.
Some allergic reactions may occur during the injection. Tell your caregiver right away if you feel dizzy, nauseated, light-headed, itchy, cold, sweaty, or if you have chest pain, trouble breathing, or swelling in your face.
Tysabri may cause serious viral infections of the brain or spinal cord that can lead to disability or death. Call your doctor right away if you have any of the following symptoms during treatment with Tysabri or up to 6 months after your last dose (these symptoms may start gradually and get worse quickly):
-
sudden fever or severe headache;
-
confusion, memory problems, or other changes in your mental state;
-
weakness on one side of your body;
-
vision changes, eye pain or redness;
-
problems with speech or walking; or
-
trouble using your arms and legs.
Also call your doctor at once if you have:
-
fever, chills, cough with yellow or green mucus;
-
easy bruising, unusual bleeding (nosebleeds, bleeding gums, heavy menstrual periods), purple or red spots under your skin;
-
any bleeding that will not stop;
-
pain or burning when you urinate; or
-
liver problems - nausea, upper stomach pain, itching, tiredness, loss of appetite, dark urine, clay-colored stools, or jaundice (yellowing of the skin or eyes).
Common Tysabri side effects may include:
-
headache, tired feeling;
-
nausea, diarrhea, stomach pain;
-
cold symptoms such as stuffy nose, sneezing, sore throat;
-
joint pain, pain in your arms and legs; or
-
vaginal itching or discharge.
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Related/similar drugs
What other drugs will affect Tysabri?
Tell your doctor about all your current medicines and any you start or stop using, especially drugs that weaken the immune system such as cancer medicine, steroids, and medicines to prevent organ transplant rejection.
Other drugs may interact with natalizumab, including prescription and over-the-counter medicines, vitamins, and herbal products. Not all possible interactions are listed in this medication guide.
Tysabri Biosimilars
Biosimilar and interchangeable products are biological products that are highly similar to and have no clinically meaningful differences from the reference product.
Reference products
These are biological products that have already been approved by the FDA, against which biosimilar products are compared. There is 1 for Tysabri.
Tysabri (natalizumab) - Biogen Inc.
| Formulation type | Strength |
|---|---|
| Single-Dose Vial | 300 mg/15 mL (20 mg/mL) |
Tysabri biosimilar products
Biosimilar products can only be dispensed in place of the reference product if the healthcare provider specifically prescribes the biosimilar product by name.
Pharmacy laws for biosimilar prescribing may vary by state
Tyruko (natalizumab-sztn) - Sandoz Inc.
| Formulation type | Strength |
|---|---|
| Single-Dose Vial | 300 mg/15 mL (20 mg/mL) |
View Tyruko information in detail.
Popular FAQ
Does Tysabri suppress the immune system?
Yes, treatment with Tysabri can weaken your immune system. This may increase your risk of getting an unusual or serious infection. Tysabri increases the risk of progressive multifocal leukoencephalopathy (PML), a rare brain infection. If you have or have had PML, you cannot use Tysabri. Continue reading
How long can you take Tysabri for?
You can take Tysabri for as long as you want providing you tolerate it well, have not developed any serious side effects, and Tysabri is still preventing relapses if you have multiple sclerosis (MS) or reducing symptoms, if you have Crohn’s disease. For people with MS, some response is noted at 12 weeks, but it may take up to 2 years for the full effects to be seen. People with Crohn’s disease should discontinue Tysabri if there is no benefit after 12 weeks Continue reading
Is Tysabri a form of chemotherapy?
Tysabri is not chemotherapy, it is a targeted treatment that works by blocking the migration of lymphocytes (a type of immune cell) from the lymph nodes, across the epithelium, and into inflamed tissue. It binds to a receptor that is present on all leukocytes apart from neutrophils and prevents them from binding to their counter receptors. It may also act in several other ways to prevent the further recruitment and inflammatory activity of activated immune cells. Tysabri belongs to the class of medicines known as integrin receptor antagonists. It may also be called a selective immunosuppressant or a monoclonal antibody. Continue reading
Does Tysabri cause cancer?
Cancer has not been reported as a side effect of Tysabri (natalizumab) in clinical studies. You should tell your doctor if you have cancer now or a history of cancer (for example, leukemia or lymphoma) before you start treatment with Tysabri. Continue reading
What is the Tysabri Touch Prescribing Program?
The Tysabri TOUCH Prescribing Program is a restricted program developed by the manufacturer of Tysabri and the FDA intended to educate healthcare professionals and patients on the risks of using Tysabri, including progressive multifocal leukoencephalopathy (PML).
Continue readingHow long does a Tysabri infusion take?
Tysabri takes one hour to infuse. After a Tysabri infusion patients are also monitored for one hour for signs of a hypersensitivity-type reaction. Continue reading
More FAQ
- What biosimilars have been approved in the United States?
- How to prevent hair loss from Tysabri (natalizumab)?
More about Tysabri (natalizumab)
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (98)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- FDA approval history
- Drug class: selective immunosuppressants
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Related treatment guides
Further information
Remember, keep this and all other medicines out of the reach of children, never share your medicines with others, and use Tysabri only for the indication prescribed.
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Copyright 1996-2025 Cerner Multum, Inc. Version: 12.01.