Amprenavir Side Effects
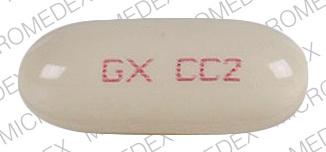
Applies to amprenavir: oral capsule liquid filled, oral solution.
Important warnings
This medicine can cause some serious health issues
Oral route (solution)
Oral solution is contraindicated in infants and children below the age of 4 years, pregnant women, patients with hepatic or renal failure, and patients treated with disulfiram or metronidazole because of the potential risk of toxicity from the large amount of the excipient, propylene glycol.
Precautions
Do not take any other medicines without checking with your doctor first. This includes prescription and nonprescription medicines. This also includes food supplements, herbs and vitamins. To do so may increase the chance of side effects from amprenavir or other medicines.
This medicine may decrease the effects of some oral contraceptives (birth control pills). To avoid unwanted pregnancy, it is a good idea to use some additional contraceptive measures while being treated with amprenavir.
For patients with diabetes: Amprenavir may affect blood sugar levels. If you notice a change in the results of your blood or urine sugar tests or if you have any questions, check with your doctor.
Do not take vitamin E supplements while you are taking amprenavir. At recommended dosages, amprenavir supplies more than the Reference Daily Intake of vitamin E for adults and children.
It is very important that your doctor check your progress at regular visits to make sure this medicine is working properly and to check for unwanted effects, especially increases in blood sugar.
Amprenavir does not decrease the risk of transmitting the HIV infection to others through sexual contact or by contamination through blood. HIV may be acquired from or spread to others through infected body fluids, including blood, vaginal fluid, or semen. If you are infected, it is best to avoid any sexual activity involving an exchange of body fluids with other people. If you do have sex, always wear (or have your partner wear) a condom (“rubber”). Only use condoms made of latex, and use them every time you have vaginal, anal, or oral sex. The use of a spermicide (such as nonoxynol-9) may also help prevent the spread of HIV if it is not irritating to the vagina, rectum, or mouth. Spermicides have been shown to kill HIV in lab tests. Do not use oil-based jelly, cold cream, baby oil, or shortening as a lubricant—these products can cause the condom to break. Lubricants without oil, such as K-Y Jelly, are recommended. Women may wish to carry their own condoms. Birth control pills and diaphragms will help protect against pregnancy, but they will not prevent someone from giving or getting the AIDS virus. If you inject drugs, get help to stop. Do not share needles or equipment with anyone. In some cities, more than half of the drug users are infected, and sharing even 1 needle or syringe can spread the virus. If you have any questions about this, check with your health care professional.
Serious side effects of amprenavir
Along with its needed effects, amprenavir may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor as soon as possible if any of the following side effects occur while taking amprenavir:
More common side effects
- burning or prickling sensation in arms or legs
- dry or itchy skin
- fatigue
- increased cholesterol and triglycerides
- increased hunger
- increased thirst
- increased urination
- skin rash
Less common side effects
- depression
- mood or mental changes
Rare side effects
- back, leg or stomach pains
- bleeding gums
- blistering, peeling, or loosening of skin and mucous membranes
- buffalo hump
- chills
- dark urine
- difficult breathing
- fatigue
- fever
- general body swelling
- general feeling of discomfort or illness
- loss of appetite
- nosebleeds
- pale skin
- sore throat
- unexplained weight loss
- yellowing of eyes or skin
Other side effects of amprenavir
Some side effects of amprenavir may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common side effects
- abdominal pain
- burning or prickling sensation around the mouth
- diarrhea
- headache
- nausea
- vomiting
Less common or rare side effects
- change in sense of taste
- unusual tiredness or weakness
See also:
For healthcare professionals
Applies to amprenavir: oral capsule, oral solution.
General adverse events
Gastrointestinal side effects and skin rashes were the most frequent side effects in clinical trials of amprenavir in combination with other antiretrovirals. Gastrointestinal effects (nausea, vomiting, diarrhea, and abdominal pain) most often resulted in discontinuation of amprenavir during the first 12 weeks of treatment. Skin rashes had a median onset and duration of 11 and 10 days, respectively, and led to discontinuation of amprenavir in 3% of patients.[Ref]
Gastrointestinal
Gastrointestinal side effects have included nausea (74%), vomiting (34%), and diarrhea or loose stools (39%) in clinical trials when amprenavir was administered with lamivudine and zidovudine in therapy-naive patients. This compares to an incidence of 50%, 17%, and 34%, respectively, when therapy-naive patients were only administered lamivudine and zidovudine. Abdominal symptoms (unspecified, 14%) and anorexia have been reported in patients receiving amprenavir in combination with ritonavir plus other antiretrovirals.[Ref]
Dermatologic
Dermatologic side effects have been reported frequently. Skin rash occurred in 28% of HIV-1 infected patients treated with amprenavir in all multidose studies. Severe or life-threatening rash, including Stevens-Johnson syndrome, occurred in 1% of patients.[Ref]
Rashes were usually maculopapular, mild to moderate in intensity, and some with pruritus. The onset of rash development was approximately 10 days and ranged from 7 to 73 days. Amprenavir was often continued with mild to moderate rash and if discontinued, rash did not recur when the drug was restarted. Amprenavir should be discontinued for severe or life-threatening rashes and for moderate rashes accompanied by systemic symptoms.[Ref]
Metabolic
Metabolic side effects have included hyperglycemia (37%), hypertriglyceridemia (36%), and hypercholesterolemia (4%) in clinical trials when amprenavir was administered with lamivudine and zidovudine in therapy-naive nonfasting patients. This compares to an incidence of 29%, 22% and 3%, respectively, when therapy-naive nonfasting patients were only administered lamivudine and zidovudine. Grade 3/4 hypertriglyceridemia (8% to 13%) and hyperglycemia (2% to 3%) have been reported in patients receiving amprenavir in combination with ritonavir. New onset and exacerbation of preexisting diabetes mellitus, elevated serum creatine kinase, and ketoacidosis have also been reported.[Ref]
Hepatic
Hepatic side effects have included elevations in AST (greater than 5 times ULN), ALT (greater than 5 times ULN), and amylase (greater than 2 times ULN) in 3% to 5% of patients receiving amprenavir in combination with ritonavir.[Ref]
Nervous system
Nervous system side effects have included oral/perioral paresthesia (26%) and other paresthesias (10%), including peripheral paresthesias, in clinical trials when amprenavir was administered with lamivudine and zidovudine in therapy-naive patients. This compares to an incidence of 6% and 4%, respectively, when therapy-naive patients were only administered lamivudine and zidovudine. Headache (12% to 16%) has been reported in patients receiving amprenavir in combination with ritonavir plus other antiretrovirals.[Ref]
Psychiatric
Psychiatric side effects have included depression and mood disorder in 15% of therapy-naive patients who were administered amprenavir with lamivudine and zidovudine in clinical trials. This compares to an incidence of 4% when therapy-naive patients were only administered lamivudine and zidovudine.[Ref]
Hematologic
Hematologic side effects have included neutropenia and hemolytic anemia. Hematologic side effects associated with protease inhibitors have included spontaneous bleeding in patients with hemophilia A and B. In many of the reported cases, treatment with protease inhibitors was continued or restarted and some patients required additional factor VIII. A causal relationship between protease inhibitor therapy and these episodes has not been established.[Ref]
Other
Redistribution/accumulation of body fat, including central obesity, dorsocervical fat enlargement, peripheral wasting, breast enlargement, and "cushingoid appearance" have been observed in patients receiving protease inhibitors. The mechanism and long-term consequences of these events are currently unknown and a causal relationship has not been established. In one case, reduction of neck fat disposition (buffalo hump) was reported when amprenavir replaced indinavir in a regimen.[Ref]
Other side effects have included taste disorders in 10% of therapy-naive patients who were administered amprenavir with lamivudine and zidovudine in clinical trials. This compares to an incidence of 5% when therapy-naive patients were only administered lamivudine and zidovudine. Fatigue (7% to 14%) and chills have been reported in patients receiving amprenavir in combination with ritonavir plus other antiretrovirals.[Ref]
Hypersensitivity
Hypersensitivity side effects have included urticaria.[Ref]
References
1. (2001) "Product Information. Agenerase (amprenavir)." Glaxo Wellcome
2. Bart PA, Rizzardi GP, Tambussi G, Chave JP, Chapuis AG, Graziois C, Corpataux JM, Halkic N, Meuwly JY, Munoz M, Meylan P, (2000) "Immunological and virological responses in HIV-1-infected adults at early stage of established infection treated with highly active antiretroviral therapy." Aids, 14, p. 1887-97
3. (2001) "Drugs for HIV infection." Med Lett Drugs Ther, 43, p. 103-8
4. Anderson PL (2004) "Pharmacologic perspectives for once-daily antiretroviral therapy." Ann Pharmacother, 38, p. 1969-70
5. Arvieux C, Tribut O (2005) "Amprenavir or Fosamprenavir plus Ritonavir in HIV Infection: Pharmacology, Efficacy and Tolerability Profile." Drugs, 65, p. 633-59
6. Wire MB, Baker KL, Jones LS, et al. (2006) "Ritonavir Increases Plasma Amprenavir (APV) Exposure to a Similar Extent when Coadministered with either Fosamprenavir or APV." Antimicrob Agents Chemother, 50, p. 1578-80
7. DHHS Panel on Antiretroviral Guidelines for Adults and Adolescents -- A Working Group of the Office of AIDS Research Advisory Council (OARAC) (2006) Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. http://aidsinfo.nih.gov/ContentFiles/AdultandAdolescentGL.pdf
8. The National Institutes of Health, The Working Group on Antiretroviral Therapy and Medical Management of HIV Infected Children Francois-Xavier Bagnoud Center, UMDNJ, The Health Resources and Services Administration (2006) Guidelines for the use of antiretroviral agents in pediatric HIV infection. http://aidsinfo.nih.gov/ContentFiles/PediatricGuidelines.pdf
9. Adkins JC, Faulds D (1998) "Amprenavir." Drugs, 55, 837-42;disc. 843-4
10. Borras-Blasco J, Navarro-Ruiz A, Borras C, Castera E (2008) "Adverse cutaneous reactions associated with the newest antiretroviral drugs in patients with human immunodeficiency virus infection." J Antimicrob Chemother, 62, p. 879-88
11. Costa A, Pulido F, Rubio R, Cepeda C, Torralba M, Costa JR (2002) "Lipid changes in HIV-infected patients who started rescue therapy with an amprenavir/ritonavir-based highly active antiretroviral therapy." AIDS, 16, p. 1983-4
12. Bergersen BM (2006) "Cardiovascular Risk in Patients with HIV Infection : Impact of Antiretroviral Therapy." Drugs, 66, p. 1971-87
13. Khanlou H, Adair M, Farthing C (2000) "Reduction of buffalo hump by switching to amprenavir in an HIV-infected patient." Arch Intern Med, 160, p. 3499-500
Frequently asked questions
More about amprenavir
- Check interactions
- Compare alternatives
- Dosage information
- During pregnancy
- Drug class: protease inhibitors
Related treatment guides
Further information
Amprenavir side effects can vary depending on the individual. Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Note: Medication side effects may be underreported. If you are experiencing side effects that are not listed, submit a report to the FDA by following this guide.