Nuromax: Package Insert / Prescribing Info
Package insert / product label
Generic name: doxacurium chloride
Dosage form: injection
Drug class: Neuromuscular blocking agents
Medically reviewed by Drugs.com. Last updated on Mar 25, 2025.
On This Page
This drug should be administered only by adequately trained individuals familiar with its actions, characteristics, and hazards.
Nuromax Description
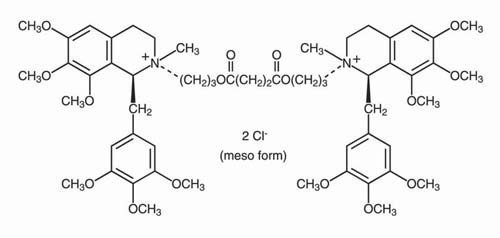
NUROMAX (doxacurium chloride) is a long-acting, nondepolarizing skeletal muscle relaxant for intravenous administration. Doxacurium chloride is [1α,2β(1'S*,2'R*)]-2,2'-[(1,4-dioxo-1,4-butanediyl)bis(oxy-3,1-propanediyl)]bis[1,2,3,4-tetrahydro-6,7,8-trimethoxy-2- methyl-1-[(3,4,5-trimethoxyphenyl)methyl]isoquinolinium] dichloride (meso form). The molecular formula is C56H78CI2N2O16 and the molecular weight is 1106.14. The compound does not partition into the 1-octanol phase of a distilled water/ 1-octanol system, i.e., the n-octanol:water partition coefficient is 0.
Doxacurium chloride is a mixture of three trans, trans stereoisomers, a dl pair [(1R,1'R,2S,2'S) and (1S,1'S,2R,2'R)] and a meso form (1R,1'S,2S,2'R). The meso form is illustrated below:
NUROMAX Injection is a sterile, nonpyrogenic aqueous solution (pH 3.9 to 5.0) containing doxacurium chloride equivalent to 1 mg/mL doxacurium in Water for Injection. Hydrochloric acid may have been added to adjust pH. NUROMAX Injection contains 0.9% w/v benzyl alcohol.
Nuromax - Clinical Pharmacology
NUROMAX binds competitively to cholinergic receptors on the motor end-plate to antagonize the action of acetylcholine, resulting in a block of neuromuscular transmission. This action is antagonized by acetylcholinesterase inhibitors, such as neostigmine.
Pharmacodynamics
NUROMAX is approximately 2.5 to 3 times more potent than pancuronium and 10 to 12 times more potent than metocurine. NUROMAX in doses of 1.5 to 2 × ED95 has a clinical duration of action (range and variability) similar to that of equipotent doses of pancuronium and metocurine (historic data and limited comparison). The average ED95 (dose required to produce 95% suppression of the adductor pollicis muscle twitch response to ulnar nerve stimulation) of NUROMAX is 0.025 mg/kg (range: 0.020 to 0.033) in adults receiving balanced anesthesia.
The onset and clinically effective duration (time from injection to 25% recovery) of NUROMAX administered alone or after succinylcholine during stable balanced anesthesia are shown in Table 1.
| Initial
Dose of NUROMAX (mg/kg) |
|||
|
* Values shown are means (range). † NUROMAX administered after 10% to 100% recovery from an intubating dose of succinylcholine. |
|||
| 0.025†
(n = 34) | 0.05 (n = 27) | 0.08 (n = 9) |
|
| Time to Maximum Block (min) | 9.3 (5.4-16) | 5.2 (2.5-13) | 3.5 (2.4-5) |
| Clinical Duration (min) (Time to 25% Recovery) | 55 (9-145) | 100 (39-232) | 160 (110-338) |
Initial doses of 0.05 mg/kg (2 × ED95) and 0.08 mg/kg (3 × ED95) NUROMAX administered during the induction of thiopental-narcotic anesthesia produced good-to-excellent conditions for tracheal intubation in 5 minutes (13 of 15 cases studied) and 4 minutes (eight of nine cases studied) (which are before maximum block), respectively.
As with other long-acting agents, the clinical duration of neuromuscular block associated with NUROMAX shows considerable interpatient variability. An analysis of 390 cases in US clinical trials utilizing a variety of premedications, varying lengths of surgery, and various anesthetic agents, indicates that approximately two thirds of the patients had clinical durations within 30 minutes of the duration predicted by dose (based on mg/kg actual body weight). Patients ≥ 60 years old are approximately twice as likely to experience prolonged clinical duration (30 minutes longer than predicted) than patients < 60 years old; thus, care should be used in older patients when prolonged recovery is undesirable (see PRECAUTIONS -Geriatric Use and CLINICAL PHARMACOLOGY - Individualization of Dosages subsection). In addition, obese patients (patients weighing ≥ 30% more than ideal body weight for height) were almost twice as likely to experience prolonged clinical duration than non-obese patients; therefore, dosing should be based on ideal body weight (IBW) for obese patients (see CLINICAL PHARMACOLOGY - Individualization of Dosages subsection).
The mean time for spontaneous T1 recovery from 25% to 50% of control following initial doses of NUROMAX is approximately 26 minutes (range: 7 to 104, n = 253) during balanced anesthesia. The mean time for spontaneous T1 recovery from 25% to 75% is 54 minutes (range: 14 to 184, n = 184).
Most patients receiving NUROMAX in clinical trials required pharmacologic reversal prior to full spontaneous recovery from neuromuscular block (see OVERDOSAGE - Antagonism of Neuromuscular Block); therefore, relatively few data are available on the time from injection to 95% spontaneous recovery of the twitch response. As with other long-acting neuromuscular blocking agents, NUROMAX may be associated with prolonged times to full spontaneous recovery. Following an initial dose of 0.025 mg/kg NUROMAX, some patients may require as long as 4 hours to exhibit full spontaneous recovery.
Cumulative neuromuscular blocking effects are not associated with repeated administration of maintenance doses of NUROMAX at 25% T1 recovery. As with initial doses, however, the duration of action following maintenance doses of NUROMAX may vary considerably among patients.
The NUROMAX ED95 for children 2 to 12 years of age receiving halothane anesthesia is approximately 0.03 mg/kg. Children require higher doses of NUROMAX on a mg/kg basis than adults to achieve comparable levels of block. The onset time and duration of block are shorter in children than adults. During halothane anesthesia, doses of 0.03 mg/kg and 0.05 mg/kg NUROMAX produce maximum block in approximately 7 and 4 minutes, respectively. The duration of clinically effective block is approximately 30 minutes after an initial dose of 0.03 mg/kg and approximately 45 minutes after 0.05 mg/kg. NUROMAX has not been studied in pediatric patients below the age of 2 years.
The neuromuscular block produced by NUROMAX may be antagonized by anticholinesterase agents. As with other nondepolarizing neuromuscular blocking agents, the more profound the neuromuscular block at reversal, the longer the time and the greater the dose of anticholinesterase required for recovery of neuromuscular function.
Hemodynamics
Administration of doses of NUROMAX up to and including 0.08 mg/kg (~3 × ED95) over 5 to 15 seconds to healthy adult patients during stable-state balanced anesthesia and to patients with serious cardiovascular disease undergoing coronary artery bypass grafting, cardiac valvular repair, or vascular repair produced no dose-related effects on mean arterial blood pressure (MAP) or heart rate (HR).
No dose-related changes in MAP and HR were observed following administration of up to 0.05 mg/kg NUROMAX over 5 to 15 seconds in 2- to 12-year-old children receiving halothane anesthesia.
Doses of 0.03 to 0.08 mg/kg (1.2 to 3 × ED95) were not associated with dose-dependent changes in mean plasma histamine concentration. Clinical experience with more than 1000 patients indicates that adverse experiences typically associated with histamine release (e.g., bronchospasm, hypotension, tachycardia, cutaneous flushing, urticaria, etc.) are very rare following the administration of NUROMAX (see ADVERSE REACTIONS).
Pharmacokinetics
Pharmacokinetic and pharmacodynamic results from a study of 24 healthy young adult patients and eight healthy elderly patients are summarized in Table 2. The pharmacokinetics are linear over the dosage range tested (i.e., plasma concentrations are approximately proportional to dose).
| Healthy
Young Adult Patients (22 to 49 yrs) | Healthy Elderly
Patients (67 to 72 yrs) |
|||
|
* Values shown are means (range). † Time from injection to 25% recovery of the control twitch height. |
||||
| Parameter | 0.025 mg/kg (n = 8) | 0.05 mg/kg (n = 8) | 0.08 mg/kg (n = 8) | 0.025 mg/kg (n = 8) |
| t½ elimination (min) | 86 (25-171) | 123 (61-163) | 98 (47-163) | 96 (50-114) |
| Volume of Distribution at Steady State (L/kg) | 0.15 (0.10-0.21) | 0.24 (0.13-0.30) | 0.22 (0.16-0.33) | 0.22 (0.14-0.40) |
| Plasma Clearance (mL/min per kg) | 2.22 (1.02-3.95) | 2.62 (1.21-5.70) | 2.53 (1.88-3.38) | 2.47 (1.58-3.60) |
| Maximum Block (%) | 97 (88-100) | 100 (100-100) | 100 (100-100) | 96 (90-100) |
| Clinically Effective Duration of Block† (min) | 68 (35-90) | 91 (47-132) | 177 (74-268) | 97 (36-179) |
This study showed that the pharmacokinetics of NUROMAX were similar in healthy young adult and elderly patients. Some healthy elderly patients tended to be more sensitive to the neuromuscular blocking effects of NUROMAX than healthy young adult patients receiving the same dose. The time to maximum block was longer in elderly patients than in young adult patients (11.2 minutes versus 7.7 minutes at 0.025 mg/kg NUROMAX). In addition, the clinically effective duration of block was more variable and tended to be longer in healthy elderly patients than in healthy young adult patients receiving the same dose. In contrast, a second study evaluated the pharmacokinetics and pharmacodynamics of doxacurium and showed that the plasma clearance was lower (1.75 ± 0.16 vs. 2.54 ± 0.24, respectively) and the half-life was longer (120 ± 10 vs. 75.9 ± 4.4 minutes, respectively) in 9 elderly patients (70 to 83 years of age) than in 9 younger patients (19 to 39 years of age) receiving a single intravenous dose of NUROMAX 0.03 mg/kg. In addition, the time to maximum block was slower (12.9 versus 8.9 minutes, respectively) and the time to 25% T1 recovery was longer (113.4 ± 17.0 vs. 48.1 ± 5.2 minutes, respectively) in elderly patients than in younger patients. Overall, these studies showed that there may be differences in the pharmacokinetics of doxacurium in individual elderly patients and that the onset is slower and the duration of action is likely to be more variable and may be longer in elderly patients.
Table 3 summarizes the pharmacokinetic and pharmacodynamic results from a study of nine healthy young adult patients, eight patients with end-stage kidney disease undergoing kidney transplantation, and seven patients with end-stage liver disease undergoing liver transplantation. The results suggest that a longer t½ can be expected in patients with end-stage kidney disease; in addition, these patients may be more sensitive to the neuromuscular blocking effects of NUROMAX. The time to maximum block was slightly longer and the clinically effective duration of block was prolonged in patients with end-stage kidney disease.
| Healthy Young Adult Patients | Kidney Transplant Patients | Liver Transplant Patients | |
|
* Values shown are means (range). |
|||
| Parameter | 0.015 mg/kg (n = 9) | 0.015 mg/kg (n = 8) | 0.015 mg/kg (n = 7) |
| t½ elimination (min) | 99 (48-193) | 221 (84-592) | 115 (69-148) |
| Volume of Distribution at Steady State (L/kg) | 0.22 (0.11-0.43) | 0.27 (0.17-0.55) | 0.29 (0.17-0.35) |
| Plasma Clearance (mL/min per kg) | 2.66 (1.35-6.66) | 1.23 (0.48-2.40) | 2.30 (1.96-3.05) |
| Maximum Block (%) | 86 (59-100) | 98 (95-100) | 70 (0-100) |
| Clinically Effective Duration of Block (min) | 36 (19-80) | 80 (29-133) | 52 (20-91) |
No data are available from patients with liver disease not requiring transplantation. There are no significant alterations in the pharmacokinetics of NUROMAX in liver transplant patients. Sensitivity to the neuromuscular blocking effects of NUROMAX was highly variable in patients undergoing liver transplantation. Three of seven patients developed ≤ 50% block, indicating that a reduced sensitivity to NUROMAX may occur in such patients. In those patients who developed > 50% neuromuscular block, the time to maximum block and the clinically effective duration tended to be longer than in healthy young adult patients (see CLINICAL PHARMACOLOGY - Individualization of Dosages subsection).
Consecutively administered maintenance doses of 0.005 mg/kg NUROMAX, each given at 25% T1 recovery following the preceding dose, do not result in a progressive increase in the plasma concentration of doxacurium or a progressive increase in the depth or duration of block produced by each dose.
NUROMAX is not metabolized in vitro in fresh human plasma. Plasma protein binding of NUROMAX is approximately 30% in human plasma.
In vivo data from humans suggest that NUROMAX is not metabolized and that the major elimination pathway is excretion of unchanged drug in urine and bile. In studies of healthy adult patients, 24% to 38% of an administered dose was recovered as parent drug in urine over 6 to 12 hours after dosing. High bile concentrations of NUROMAX (relative to plasma) have been found 35 to 90 minutes after administration. The overall extent of biliary excretion is unknown. The data derived from analysis of human urine and bile are consistent with data from in vivo studies in the rat, cat, and dog, which indicate that all of an administered dose of NUROMAX is recovered as parent drug in the urine and bile of these species.
Individualization of Dosages
In elderly patients or patients who have impaired renal function, the potential for a prolongation of block may be reduced by decreasing the initial dose of NUROMAX and by titrating the dose to achieve the desired depth of block. In obese patients (patients weighing ≥ 30% more than ideal body weight for height), the dose of NUROMAX should be determined using the patient's ideal body weight (IBW), according to the following formulae:
Men: IBW in kg = [106 + (6 × inches in height above 5 feet)]/2.2
Women: IBW in kg = [100 + (5 × inches in height above 5 feet)]/2.2
Dosage requirements for patients with severe liver disease are variable; some patients may require a higher than normal initial dose of NUROMAX to achieve clinically effective block. Once adequate block is established, the clinical duration of block may be prolonged in such patients relative to patients with normal liver function.
As with pancuronium, metocurine, and vecuronium, resistance to NUROMAX, manifested by a reduced intensity and/or shortened duration of block, must be considered when NUROMAX is selected for use in patients receiving phenytoin or carbamazepine (see PRECAUTIONS - Drug Interactions).
As with other nondepolarizing neuromuscular blocking agents, a reduction in dosage of NUROMAX must be considered in cachectic or debilitated patients; in patients with neuromuscular diseases, severe electrolyte abnormalities, or carcinomatosis; and in other patients in whom potentiation of neuromuscular block or difficulty with reversal is anticipated. Increased doses of NUROMAX may be required in burn patients (see PRECAUTIONS).
Indications and Usage for Nuromax
NUROMAX is a long-acting neuromuscular blocking agent, indicated to provide skeletal muscle relaxation as an adjunct to general anesthesia, for endotracheal intubation or to facilitate mechanical ventilation.
Contraindications
NUROMAX is contraindicated in patients known to have hypersensitivity to it. Use of NUROMAX from multiple-dose vials containing benzyl alcohol as a preservative is contraindicated in patients with a known hypersensitivity to benzyl alcohol.
Warnings
NUROMAX SHOULD BE ADMINISTERED IN CAREFULLY ADJUSTED DOSAGE BY OR UNDER THE SUPERVISION OF EXPERIENCED CLINICIANS WHO ARE FAMILIAR WITH THE DRUG'S ACTIONS AND THE POSSIBLE COMPLICATIONS OF ITS USE. THE DRUG SHOULD NOT BE ADMINISTERED UNLESS FACILITIES FOR INTUBATION, ARTIFICIAL RESPIRATION, OXYGEN THERAPY, AND AN ANTAGONIST ARE WITHIN IMMEDIATE REACH. IT IS RECOMMENDED THAT CLINICIANS ADMINISTERING LONG-ACTING NEUROMUSCULAR BLOCKING AGENTS SUCH AS NUROMAX EMPLOY A PERIPHERAL NERVE STIMULATOR TO MONITOR DRUG RESPONSE, NEED FOR ADDITIONAL RELAXANTS, AND ADEQUACY OF SPONTANEOUS RECOVERY OR ANTAGONISM.
NUROMAX HAS NO KNOWN EFFECT ON CONSCIOUSNESS, PAIN THRESHOLD, OR CEREBRATION. TO AVOID DISTRESS TO THE PATIENT, NEUROMUSCULAR BLOCK SHOULD NOT BE INDUCED BEFORE UNCONSCIOUSNESS.
NUROMAX Injection is acidic (pH 3.9 to 5.0) and may not be compatible with alkaline solutions having a pH greater than 8.5 (e.g., barbiturate solutions).
NUROMAX Injection contains benzyl alcohol. In newborn infants, benzyl alcohol has been associated with an increased incidence of neurological and other complications which are sometimes fatal (see PRECAUTIONS - Pediatric Use).
Precautions
General
NUROMAX has no clinically significant effects on heart rate; therefore, NUROMAX will not counteract the bradycardia produced by many anesthetic agents or by vagal stimulation.
Neuromuscular blocking agents may have a profound effect in patients with neuromuscular diseases (e.g., myasthenia gravis and the myasthenic syndrome). In these and other conditions in which prolonged neuromuscular block is a possibility (e.g., carcinomatosis), the use of a peripheral nerve stimulator and a small test dose of NUROMAX are recommended to assess the level of neuromuscular block and to monitor dosage requirements. Shorter acting muscle relaxants than NUROMAX may be more suitable for these patients.
Resistance to nondepolarizing neuromuscular blocking agents may develop in patients with burns depending upon the time elapsed since the injury and the size of the burn. NUROMAX has not been studied in patients with burns.
Acid-base and/or serum electrolyte abnormalities may potentiate or antagonize the action of neuromuscular blocking agents. The action of neuromuscular blocking agents may be enhanced by magnesium salts administered for the management of toxemia of pregnancy.
NUROMAX has not been studied in patients with asthma.
No data are available to support the use of NUROMAX by intramuscular injection.
Renal and Hepatic Disease
NUROMAX has been studied in patients with end-stage kidney (n = 8) or liver (n = 7) disease undergoing transplantation procedures (see CLINICAL PHARMACOLOGY). The possibility of prolonged neuromuscular block in patients undergoing renal transplantation and the possibility of a variable onset and duration of neuromuscular block in patients undergoing liver transplantation must be considered when NUROMAX is used in such patients.
Obesity
Administration of NUROMAX on the basis of actual body weight is associated with a prolonged duration of action in obese patients (patients weighing ≥ 30% more than ideal body weight for height) (see CLINICAL PHARMACOLOGY). Therefore, the dose of NUROMAX should be based upon ideal body weight in obese patients (see CLINICAL PHARMACOLOGY - Individualization of Dosages).
Malignant Hyperthermia (MH)
In a study of MH-susceptible pigs, NUROMAX did not trigger MH. NUROMAX has not been studied in MH-susceptible patients. Since MH can develop in the absence of established triggering agents, the clinician should be prepared to recognize and treat MH in any patient scheduled for general anesthesia.
Long-Term Use in the Intensive Care Unit (ICU)
Information on the use of NUROMAX in the ICU is limited. In a double-blind, randomized study, 17 patients received NUROMAX by intermittent bolus injection for a mean of 2.7 ± 0.5 days (range: 0.8 to 6.8 days) to facilitate mechanical ventilation. No evidence of tachyphylaxis, accumulation, or prolonged recovery was observed. The adverse experiences in patients receiving NUROMAX were consistent in type, severity, and frequency to those expected in a critically ill patient population. Since many ICU patients have hepatic and/or renal failure, a prolonged duration of block should be anticipated in these patients after administration of NUROMAX.
WHENEVER THE USE OF NUROMAX OR ANY NEUROMUSCULAR BLOCKING AGENT IS CONTEMPLATED IN THE ICU, IT IS RECOMMENDED THAT NEUROMUSCULAR TRANSMISSION BE MONITORED CONTINUOUSLY DURING ADMINISTRATION WITH THE HELP OF A NERVE STIMULATOR. ADDITIONAL DOSES OF NUROMAX OR ANY OTHER NEUROMUSCULAR BLOCKING AGENT SHOULD NOT BE GIVEN BEFORE THERE IS A DEFINITE RESPONSE TO T1, OR TO THE FIRST TWITCH. IF NO RESPONSE IS ELICITED, BOLUS ADMINISTRATION SHOULD BE DELAYED UNTIL A RESPONSE RETURNS.
Drug Interactions
Prior administration of succinylcholine has no clinically important effect on the neuromuscular blocking action of NUROMAX.
The use of NUROMAX before succinylcholine to attenuate some of the side effects of succinylcholine has not been studied.
There are no clinical data on concomitant use of NUROMAX and other nondepolarizing neuromuscular blocking agents.
Isoflurane, enflurane, and halothane decrease the ED50 of NUROMAX by 30% to 45%. These agents may also prolong the clinically effective duration of action by up to 25%.
Other drugs which may enhance the neuromuscular blocking action of nondepolarizing agents such as NUROMAX include certain antibiotics (e.g., aminoglycosides, tetracyclines, bacitracin, polymyxins, lincomycin, clindamycin, colistin, and sodium colistimethate), magnesium salts, lithium, local anesthetics, procainamide, and quinidine.
As with some other nondepolarizing neuromuscular blocking agents, the time of onset of neuromuscular block induced by NUROMAX is lengthened and the duration of block is shortened in patients receiving phenytoin or carbamazepine.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis and fertility studies have not been performed. NUROMAX was evaluated in a battery of four short-term mutagenicity tests. It was nonmutagenic in the Ames Salmonella assay, in the mouse lymphoma assay, and in the human lymphocyte assay. In the in vivo rat bone marrow cytogenetic assay, statistically significant increases in the incidence of structural abnormalities, relative to vehicle controls, were observed in male rats dosed with 0.1 mg/kg (0.625 mg/m2) NUROMAX and sacrificed at 6 hours, but not at 24 or 48 hours, and in female rats dosed with 0.2 mg/kg (1.25 mg/m2) NUROMAX and sacrificed at 24 hours, but not at 6 or 48 hours. There was no increase in structural abnormalities in either male or female rats given 0.3 mg/kg (1.875 mg/m2) NUROMAX and sacrificed at 6, 24, or 48 hours. Thus, the incidence of abnormalities in the in vivo rat bone marrow cytogenetic assay was not dose-dependent and, therefore, the likelihood that the observed abnormalities were treatment-related or clinically significant is low.
Pregnancy
Teratogenic Effect
Pregnancy Category C.
Teratology testing in nonventilated, pregnant rats and mice treated subcutaneously with maximum subparalyzing doses of NUROMAX revealed no maternal or fetal toxicity or teratogenic effects. There are no adequate and well-controlled studies of NUROMAX in pregnant women. Because animal studies are not always predictive of human response and the doses used were subparalyzing, NUROMAX should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Labor and Delivery
The use of NUROMAX during labor, vaginal delivery, or cesarean section has not been studied. It is not known whether NUROMAX administered to the mother has immediate or delayed effects on the fetus. The duration of action of NUROMAX exceeds the usual duration of operative obstetrics (cesarean section). Therefore, NUROMAX is not recommended for use in patients undergoing C-section.
Nursing Mothers
It is not known whether NUROMAX is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised following administration of NUROMAX to a nursing woman.
Pediatric Use
NUROMAX has not been studied in pediatric patients below the age of 2 years. See CLINICAL PHARMACOLOGY and DOSAGE AND ADMINISTRATION for clinical experience and recommendations for use in children 2 to 12 years of age.
Geriatric Use
Of the total number of subjects in the clinical studies of NUROMAX, 134 were 60 years of age and over while 37 were 70 years of age and over. The geriatric population included a subset of patients with significant cardiovascular disease. The clearance of doxacurium may be reduced and the half-life may be prolonged in elderly patients. In addition, the onset of maximum block is slower and the duration of neuromuscular block produced by NUROMAX is more variable and, in some cases, longer than in young adult patients (see CLINICAL PHARMACOLOGY - Pharmacodynamics and Individualization of Dosages).
This drug is known to be excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection and it may be useful to monitor renal function.
Adverse Reactions/Side Effects
The most frequent adverse effect of nondepolarizing blocking agents as a class consists of an extension of the pharmacological action beyond the time needed for surgery and anesthesia. This effect may vary from skeletal muscle weakness to profound and prolonged skeletal muscle paralysis resulting in respiratory insufficiency and apnea which require manual or mechanical ventilation until recovery is judged to be clinically adequate (see OVERDOSAGE). Inadequate reversal of neuromuscular block from NUROMAX is possible, as with all nondepolarizing agents. Prolonged neuromuscular block and inadequate reversal may lead to postoperative complications.
Observed in Clinical Trials
Adverse experiences were uncommon among the 1034 surgical patients and volunteers who received NUROMAX and other drugs in US clinical studies in the course of a wide variety of procedures conducted during balanced or inhalational anesthesia. The following adverse experiences were reported in patients administered NUROMAX (all events judged by investigators during the clinical trials to have a possible causal relationship):
Incidence Less than 1%
| Cardiovascular:* | Hypotension,† flushing,† ventricular fibrillation, myocardial infarction |
|
* Reports of ventricular fibrillation (n = 1) and myocardial infarction (n = 1) were limited to ASA Class 3-4 patients undergoing cardiac surgery (n = 142). † 0.3% incidence. All other reactions unmarked were ≤ 0.1%. |
|
| Respiratory: | Bronchospasm, wheezing |
| Dermatological: | Urticaria, injection site reaction |
| Special Senses: | Diplopia |
| Nonspecific: | Difficult neuromuscular block reversal, prolonged drug effect, fever |
Related/similar drugs
Overdosage
Overdosage with neuromuscular blocking agents may result in neuromuscular block beyond the time needed for surgery and anesthesia. The primary treatment is maintenance of a patent airway and controlled ventilation until recovery of normal neuromuscular function is assured. Once evidence of recovery from neuromuscular block is observed, further recovery may be facilitated by administration of an anticholinesterase agent (e.g., neostigmine, edrophonium) in conjunction with an appropriate anticholinergic agent (see Antagonism of Neuromuscular Block below).
Antagonism of Neuromuscular Block
ANTAGONISTS (SUCH AS NEOSTIGMINE) SHOULD NOT BE ADMINISTERED PRIOR TO THE DEMONSTRATION OF SOME SPONTANEOUS RECOVERY FROM NEUROMUSCULAR BLOCK. THE USE OF A NERVE STIMULATOR TO DOCUMENT RECOVERY AND ANTAGONISM OF NEUROMUSCULAR BLOCK IS RECOMMENDED. T4/T1 SHOULD BE > ZERO BEFORE ANTAGONISM IS ATTEMPTED.
In an analysis of patients in whom antagonism of neuromuscular block was evaluated following administration of single doses of neostigmine averaging 0.06 mg/kg (range: 0.05 to 0.075) administered at approximately 25% T1 spontaneous recovery during balanced anesthesia, 71% of patients exhibited T4/T1≥ 0.7 before monitoring was discontinued. For these patients, the mean time to T4/T1≥ 0.7 was 19 minutes (range: 7 to 55). As with other long-acting nondepolarizing neuromuscular blocking agents, the time for recovery of neuromuscular function following administration of neostigmine is dependent upon the level of residual neuromuscular block at the time of attempted reversal; longer recovery times than those cited above may be anticipated when neostigmine is administered at more profound levels of block (i.e., at < 25% T1 recovery).
Patients should be evaluated for adequate clinical evidence of antagonism, e.g., 5-second head lift, and grip strength. Ventilation must be supported until no longer required. As with other neuromuscular blocking agents, physicians should be alert to the possibility that the action of the drugs used to antagonize neuromuscular block may wear off before the effects of NUROMAX on the neuromuscular junction have declined sufficiently.
Antagonism may be delayed in the presence of debilitation, carcinomatosis, and the concomitant use of certain broad-spectrum antibiotics or anesthetic agents and other drugs which enhance neuromuscular block or separately cause respiratory depression (see PRECAUTIONS - Drug Interactions). Under such circumstances the management is the same as that of prolonged neuromuscular block.
In clinical trials, a dose of 1 mg/kg edrophonium was not as effective as a dose of 0.06 mg/kg neostigmine in antagonizing moderate to deep levels of neuromuscular block (i.e., < 60% T1 recovery). Therefore, the use of 1 mg/kg edrophonium is not recommended for reversal from moderate to deep levels of block. The use of pyridostigmine has not been studied.
Nuromax Dosage and Administration
NUROMAX SHOULD ONLY BE ADMINISTERED INTRAVENOUSLY.
NUROMAX, like other long-acting neuromuscular blocking agents, displays variability in the duration of its effect. The potential for a prolonged clinical duration of neuromuscular block must be considered when NUROMAX is selected for administration. The dosage information provided below is intended as a guide only. Doses should be individualized (see CLINICAL PHARMACOLOGY -Individualization of Dosages). Factors that may warrant dosage adjustment include: advancing age, the presence of kidney or liver disease, or obesity (patients weighing ≥ 30% more than ideal body weight for height). The use of a peripheral nerve stimulator will permit the most advantageous use of NUROMAX, minimize the possibility of overdosage or underdosage, and assist in the evaluation of recovery.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration whenever solution and container permit.
Adults
Initial Doses
When administered as a component of a thiopental/narcotic induction-intubation paradigm as well as for production of long-duration neuromuscular block during surgery, 0.05 mg/kg (2 × ED95) NUROMAX produces good-to-excellent conditions for tracheal intubation in 5 minutes in approximately 90% of patients. Lower doses of NUROMAX may result in a longer time for development of satisfactory intubation conditions. Clinically effective neuromuscular block may be expected to last approximately 100 minutes on average (range: 39 to 232) following 0.05 mg/kg NUROMAX administered to patients receiving balanced anesthesia.
An initial NUROMAX dose of 0.08 mg/kg (3 × ED95) should be reserved for instances in which a need for very prolonged neuromuscular block is anticipated. In approximately 90% of patients, good-to-excellent intubation conditions may be expected in 4 minutes after this dose; however, clinically effective block may be expected to persist for as long as 160 minutes or more (range: 110 to 338) (see CLINICAL PHARMACOLOGY).
If NUROMAX is administered during steady-state isoflurane, enflurane, or halothane anesthesia, reduction of the dose of NUROMAX by one third should be considered.
When succinylcholine is administered to facilitate tracheal intubation in patients receiving balanced anesthesia, an initial dose of 0.025 mg/kg (ED95) NUROMAX provides about 60 minutes (range: 9 to 145) of clinically effective neuromuscular block for surgery. For a longer duration of action, a larger initial dose may be administered.
Maintenance Doses
Maintenance dosing will generally be required about 60 minutes after an initial dose of 0.025 mg/kg NUROMAX or 100 minutes after an initial dose of 0.05 mg/kg NUROMAX during balanced anesthesia. Repeated maintenance doses administered at 25% T1 recovery may be expected to be required at relatively regular intervals in each patient. The interval may vary considerably between patients. Maintenance doses of 0.005 and 0.01 mg/kg NUROMAX each provide an average 30 minutes (range: 9 to 57) and 45 minutes (range: 14 to 108), respectively, of additional clinically effective neuromuscular block. For shorter or longer desired durations, smaller or larger maintenance doses may be administered.
Children
When administered during halothane anesthesia, an initial dose of 0.03 mg/kg (ED95) produces maximum neuromuscular block in about 7 minutes (range: 5 to 11) and clinically effective block for an average of 30 minutes (range: 12 to 54). Under halothane anesthesia, 0.05 mg/kg produces maximum block in about 4 minutes (range: 2 to 10) and clinically effective block for 45 minutes (range: 30 to 80). Maintenance doses are generally required more frequently in children than in adults. Because of the potentiating effect of halothane seen in adults, a higher dose of NUROMAX may be required in children receiving balanced anesthesia than in children receiving halothane anesthesia to achieve a comparable onset and duration of neuromuscular block. NUROMAX has not been studied in pediatric patients below the age of 2 years.
Compatibility
Y-site Administration
NUROMAX Injection may not be compatible with alkaline solutions with a pH greater than 8.5 (e.g., barbiturate solutions).
NUROMAX is compatible with:
- 5% Dextrose Injection, USP
- 0.9% Sodium Chloride Injection, USP
- 5% Dextrose and 0.9% Sodium Chloride Injection, USP
- Lactated Ringer's Injection, USP
- 5% Dextrose and Lactated Ringer's Injection
- Sufenta® (sufentanil citrate) Injection, diluted as directed
- Alfenta® (alfentanil hydrochloride) Injection, diluted as directed
- Sublimaze® (fentanyl citrate) Injection, diluted as directed
Dilution Stability
NUROMAX diluted up to 1:10 in 5% Dextrose Injection, USP or 0.9% Sodium Chloride Injection, USP has been shown to be physically and chemically stable when stored in polypropylene syringes at 5° to 25°C (41° to 77°F), for up to 24 hours. Since dilution diminishes the preservative effectiveness of benzyl alcohol, aseptic techniques should be used to prepare the diluted product. Immediate use of the diluted product is preferred, and any unused portion of diluted NUROMAX should be discarded after 8 hours.
| NUROMAX
doxacurium chloride injection |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Abbott Laboratories |
