Tipranavir (Monograph)
Brand name: Aptivus
Drug class: HIV Protease Inhibitors
Warning
- Hepatotoxicity
-
Clinical hepatitis and hepatic decompensation, including some fatalities, reported.
-
Extra vigilance warranted in HIV-infected patients with chronic HBV or HCV coinfection since these individuals are at increased risk of hepatotoxicity.
- Intracranial Hemorrhage
-
Intracranial hemorrhage, including some fatalities, reported.
Introduction
Antiretroviral; HIV protease inhibitor (PI).
Uses for Tipranavir
Treatment of HIV Infection
Treatment of HIV-1 infection in adult and pediatric patients weighing ≥36 kg. Must be used in combination with low-dose ritonavir (ritonavir-boosted tipranavir) and other antiretrovirals.
Used in patients who are antiretroviral-experienced and infected with HIV-1 resistant to >1 HIV protease inhibitors (PIs).
Should not be used in antiretroviral-naive patients.
Tipranavir was previously used in combination with ritonavir (ritonavir-boosted) as part of a fully suppressive antiretroviral regimen. Current guidelines do not recommend its use due to inferior virological efficacy and toxicities. Consult guidelines for the most current information on recommended regimens. Selection of an initial antiretroviral regimen should be individualized based on factors such as virologic efficacy, toxicity, pill burden, dosing frequency, drug-drug interaction potential, resistance test results, comorbid conditions, access, and cost.
Tipranavir Dosage and Administration
General
Pretreatment Screening
-
Perform liver function testing (e.g., serum AST, ALT, bilirubin).
-
Use genotype or phenotype testing and consider treatment history to guide the use of ritonavir-boosted tipranavir. Ritonavir-boosted tipranavir should not be used in antiretroviral-naive patients.
-
Evaluate serum triglyceride and cholesterol concentrations; manage lipid disorders as clinically appropriate.
Patient Monitoring
-
Monitor liver function (e.g., serum AST, ALT, bilirubin) frequently during treatment and monitor for signs or symptoms of hepatitis (e.g., fatigue, malaise, anorexia, nausea, jaundice, bilirubinuria, acholic stools, liver tenderness, hepatomegaly).
-
Monitor for bleeding in patients with hemophilia.
-
Monitor for persistent hyperglycemia, new-onset diabetes mellitus, or exacerbation of preexisting diabetes mellitus. It may be necessary to initiate or adjust dosage of antidiabetic therapy (e.g., insulin, oral hypoglycemic agents).
-
Monitor serum triglyceride and cholesterol concentrations periodically during therapy with ritonavir-boosted tipranavir; manage lipid disorders as clinically appropriate.
Dispensing and Administration Precautions
-
The Institute for Safe Medication Practices (ISMP) list of error-prone abbreviations, symbols, and dose designations states that the use of abbreviations for antiretroviral medications (e.g., DOR, TAF, TDF) during the medication use process should be avoided as their use has been associated with serious medication errors.
Other General Considerations
-
Use of other antiretroviral agents active against HIV-1 with ritonavir-boosted tipranavir is associated with a greater likelihood of treatment response.
-
Use ritonavir-boosted tipranavir with caution in patients with elevated AST or ALT, in the presence of hepatitis B or C co-infection, and in patients with mild hepatic impairment (Child-Pugh Class A).
-
Use ritonavir-boosted tipranavir with caution in patients with known hypersensitivity to sulfonamide-containing drugs.
-
Use ritonavir-boosted tipranavir with caution in patients at an increased risk for bleeding, or in those receiving concomitant medications that increase bleeding risk.
Administration
Administer orally in conjunction with low-dose ritonavir (ritonavir-boosted tipranavir). Do not use without low-dose ritonavir.
Take tipranavir and low-dose ritonavir at same time with a meal.
Swallow tipranavir capsules whole; do not open or chew. Assess children for ability to swallow capsules before prescribing.
Dosage
Pediatric Patients
Treatment of HIV Infection
Oral
Antiretroviral-experienced children weighing ≥36 kg: 500 mg twice daily with low-dose ritonavir (200 mg twice daily).
Adults
Treatment of HIV Infection
Oral
Antiretroviral-experienced: 500 mg twice daily with low-dose ritonavir (200 mg twice daily).
Special Populations
Hepatic Impairment
Mild hepatic impairment (Child-Pugh class A): Dosage adjustments not necessary. Moderate or severe hepatic impairment (Child-Pugh class B or C): Contraindicated.
Renal Impairment
No specific dosage recommendations.
Geriatric Patients
No specific dosage recommendations. Select dosage with caution.
Cautions for Tipranavir
Contraindications
-
Moderate or severe hepatic impairment (Child-Pugh class B or C).
-
Concomitant use with drugs highly dependent on CYP3A for metabolism and for which elevated plasma concentrations are associated with serious and/or life-threatening events (e.g., alfuzosin, certain antiarrhythmics, cisapride, ergot alkaloids, lurasidone, pimozide, sildenafil used for treatment of pulmonary arterial hypertension [PAH], oral midazolam, triazolam, lovastatin, simvastatin).
-
Concomitant use with potent CYP3A inducers (e.g., rifampin, St. John’s wort [Hypericum perforatum]) since such use may result in decreased plasma concentrations of tipranavir and possible loss of virologic response.
Warnings/Precautions
Warnings
Hepatotoxicity
Hepatitis and hepatic decompensation (including some fatalities) reported; causal relationship not established (see Boxed Warning). Hepatotoxicity generally has occurred in patients with advanced HIV infection receiving multiple concomitant drugs. Increased concentrations of serum hepatic transaminases (grade 3 and 4) reported.
Evaluate hepatic function prior to and frequently during treatment. HIV-infected patients with coexisting HBV or HCV infection or elevated serum transaminases prior to therapy may be at increased risk for hepatotoxicity.
Discontinue if signs or symptoms of hepatitis develop, if asymptomatic increases in serum AST or ALT of >10 times the ULN occur, or if asymptomatic increases in AST or ALT of 5–10 times the ULN and increases in total bilirubin of >2.5 times the ULN develop.
Clinicians and patients should be vigilant for appearance of signs or symptoms of hepatitis (e.g., fatigue, malaise, anorexia, nausea, jaundice, bilirubinemia, acholic stools, liver tenderness, hepatomegaly).
Intracranial Hemorrhage
Intracranial hemorrhage (including some fatalities) reported (see Boxed Warning). Other medical conditions or concomitant therapy may have caused or contributed to these events. Ritonavir-boosted tipranavir therapy generally not associated with abnormal coagulation parameters; abnormal coagulation parameters have not preceded intracranial hemorrhage. Manufacturer states that routine monitoring of coagulation parameters not necessary.
Other Warnings/Precautions
Rash
Mild to moderate rash, including maculopapular rash and possible photosensitivity reactions reported. Rash accompanied by joint pain or stiffness, throat tightness, or generalized pruritus also reported.
Discontinue drug and administer appropriate treatment if severe rash occurs. Concomitant estrogen-containing oral contraceptives or estrogens for hormone replacement therapy may increase risk for developing non-serious rash.
Concomitant estrogen-containing oral contraceptives or estrogens for hormone replacement therapy may increase risk for developing non-serious rash.
Sulfonamide Allergy
Tipranavir contains a sulfonamide moiety; use with caution in patients with known sulfonamide allergy. Potential for cross-sensitivity between drugs with sulfonamide moieties and tipranavir unknown.
Importance of Co-administration with Ritonavir
Tipranavir must be used with low-dose ritonavir (ritonavir-boosted tipranavir) and administered with a meal to achieve adequate antiviral response. Failure to administer with recommended low-dose ritonavir and meals will result in subtherapeutic tipranavir concentrations and inadequate antiviral response.
Consider the usual cautions, precautions, and contraindications associated with ritonavir.
Risk of Serious Adverse Reactions Due to Drug Interactions
Concomitant use with certain drugs is not recommended or requires particular caution or dosage adjustments.
Consider potential for drug interactions prior to and during ritonavir-boosted tipranavir therapy. Review all drugs patient is receiving and monitor for adverse effects.
Effects on Platelet Aggregation and Coagulation
Tipranavir inhibits platelet aggregation in vitro. Caution advised in patients who may be at risk for increased bleeding from trauma, surgery, or other medical conditions; those receiving concomitant drugs known to increase the risk of bleeding (i.e., anticoagulants, antiplatelet agents); and those receiving high-dose vitamin E.
Diabetes Mellitus/Hyperglycemia
Hyperglycemia (potentially persistent), new-onset diabetes mellitus or exacerbation of preexisting diabetes mellitus reported with use of HIV PIs; diabetic ketoacidosis has occurred. Initiate or adjust antidiabetic therapy (e.g., insulin, oral hypoglycemic agents) as needed.
Immune Reconstitution Syndrome
During initial treatment, patients who respond to antiretroviral therapy may develop an inflammatory response to indolent or residual opportunistic infections (e.g., Mycobacterium avium complex [MAC], M. tuberculosis, cytomegalovirus [CMV], Pneumocystis jirovecii [formerly P. carinii], reactivation of herpes simplex and herpes zoster); this may necessitate further evaluation and treatment.
Autoimmune disorders (e.g., Graves' disease, polymyositis, Guillain-Barré syndrome) reported in the setting of immune reconstitution; time to onset is more variable and can occur many months after initiation of antiretroviral therapy.
Fat Redistribution
Possible redistribution or accumulation of body fat, including central obesity, dorsocervical fat enlargement (buffalo hump), peripheral wasting, breast enlargement, and general cushingoid appearance with antiretroviral therapy. Mechanism and long-term consequences of fat redistribution unknown; causal relationship not established.
Elevated Lipids
Increased concentrations of total serum cholesterol and triglycerides reported. Determine serum cholesterol and triglyceride concentrations prior to and periodically during therapy; manage lipid disorders as clinically appropriate.
Patients with Hemophilia
Spontaneous bleeding reported with HIV PIs; causal relationship not established. Use with caution in patients with history of hemophilia A or B. Increased hemostatic therapy (e.g., antihemophilic factor) may be needed.
Resistance/Cross-resistance
Potential for cross-resistance with other HIV PIs not evaluated. Effect of ritonavir-boosted tipranavir therapy on subsequent therapy with other HIV PIs unknown.
Specific Populations
Pregnancy
Antiretroviral Pregnancy Registry available at 800-258-4263 or [Web]. Data insufficient to adequately assess the risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes.
Lactation
Not known whether distributed into human milk or if drug has any effects on breastfed infant or milk production; distributed into milk in rats.
The HHS perinatal HIV transmission guideline provides updated recommendations on infant feeding. The guideline states that patients with HIV should receive evidence-based, patient-centered counseling to support shared decision making about infant feeding. During counseling, patients should be informed that feeding with appropriate formula or pasteurized donor human milk from a milk bank eliminates the risk of postnatal HIV transmission to the infant. Additionally, achieving and maintaining viral suppression with antiretroviral therapy during pregnancy and postpartum reduces the risk of breastfeeding HIV transmission to <1%, but does not completely eliminate the risk. Replacement feeding with formula or banked pasteurized donor milk is recommended when patients with HIV are not on antiretroviral therapy and/or do not have a suppressed viral load during pregnancy (at a minimum throughout the third trimester), as well as at delivery.
Females and Males of Reproductive Potential
Potential for reduced efficacy of concomitantly administered estrogen-containing oral contraceptives.
Advise patients receiving an estrogen-based oral contraceptive to use additional or alternative nonhormonal contraceptives.
Pediatric Use
Safety and efficacy established in children weighing ≥36 kg who are antiretroviral-experienced with HIV-1 strains resistant to >1 protease inhibitor. Adverse effects reported in children ≥36 kg generally similar to those reported in adults; rash reported more frequently in children than in adults.
Safety and efficacy established in children ≥2 years of age weighing <36 kg. Not recommended in this population due to lack of suitable pediatric formulation of the drug.
Geriatric Use
Insufficient experience in patients ≥65 years of age to determine whether geriatric patients respond differently than younger adults. Use with caution and monitor because of age-related decreases in hepatic, renal, and/or cardiac function and concomitant disease and drug therapy.
Hepatic Impairment
Use with caution since tipranavir concentrations may be increased. Contraindicated in moderate or severe hepatic impairment (Child-Pugh class B or C). Risk for further elevations in hepatic enzyme concentrations or severe liver disease in HIV-infected patients with chronic HBV or HCV coinfection or increased AST or ALT concentrations prior to therapy.
Renal Impairment
Pharmacokinetics not evaluated in renal impairment. Renal clearance is negligible; decreased clearance not expected in patients with renal impairment.
Common Adverse Effects
Adverse effects (>4%) in adults receiving ritonavir-boosted tipranavir in conjunction with other antiretroviral agents: diarrhea, nausea, pyrexia, fatigue, vomiting, headache, abdominal pain.
Adverse effects reported in pediatric patients were generally similar to those observed in adults, except for the incidence of rash, which occurred more frequently in pediatric patients.
Drug Interactions
Drug interaction studies were conducted using ritonavir-boostedtipranavir.
Tipranavir metabolized principally by CYP3A4.
Tipranavir with low-dose ritonavir inhibits CYP3A and 2D6.
Tipranavir is a P-glycoprotein (P-gp) substrate and is both a weak inhibitor and potent inducer of P-gp transport system.
Drugs Affecting or Metabolized by Hepatic Microsomal Enzymes
Pharmacokinetic interactions likely with drugs that are inhibitors, inducers, or substrates of CYP3A4 with possible alteration in metabolism of tipranavir, ritonavir, and/or other drug.
Drugs Affecting or Affected by P-glycoprotein Transport
Pharmacokinetic interactions likely with drugs that are P-gp inhibitors or inducers with possible altered metabolism of tipranavir or the other drug.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Abacavir |
Decreased abacavir AUC; clinical importance unknown No antagonistic antiretroviral effects in vitro |
Appropriate dosages for concomitant use with respect to safety and efficacy not established |
|
Alfuzosin |
Increased alfuzosin concentrations expected and risk of hypotension |
Concomitant use contraindicated |
|
Antacids |
Decreased tipranavir concentrations and AUC |
|
|
Antiarrhythmic agents (amiodarone, flecainide, propafenone, quinidine) |
Amiodarone, flecainide, propafenone, quinidine: Possible increased concentrations of antiarrhythmic agents |
Concomitant use contraindicated |
|
Anticoagulants, oral |
Potential for increased risk of bleeding Warfarin: Possible altered warfarin concentrations |
Caution advised when used with any anticoagulant Warfarin: Use with caution; monitor INR, especially when initiating or discontinuing ritonavir-boosted tipranavir |
|
Anticonvulsants (carbamazepine, phenobarbital, phenytoin, valproic acid) |
Carbamazepine: Possible increased carbamazepine concentrations; possible decreased tipranavir concentrations Phenobarbital, phenytoin: Possible decreased tipranavir concentrations Valproic acid: Possible decreased valproic acid concentrations |
Carbamazepine, phenobarbital, phenytoin: Use with caution Valproic acid: Use concomitantly with caution |
|
Antifungals |
Fluconazole: Increased tipranavir concentrations and AUC; no clinically important effect on fluconazole concentrations Itraconazole, ketoconazole: Increased antifungal concentrations Voriconazole: Altered voriconazole concentration; however, due to multiple enzymes involved with voriconazole metabolism, difficult to predict the interaction |
Fluconazole: Fluconazole dosage adjustment not needed, but fluconazole dosage >200 mg daily not recommended Itraconazole: Use concomitantly with caution; itraconazole dosage >200 mg daily not recommended Ketoconazole: Use concomitantly with caution; ketoconazole dosage >200 mg daily not recommended |
|
Antimycobacterials (rifabutin, rifampin) |
Rifabutin: Increased rifabutin concentrations; no change in tipranavir concentrations Rifampin: Possible decreased tipranavir concentrations; possible decreased antiretroviral activity and increased risk of tipranavir resistance |
Rifabutin: Reduce rifabutin dosage to 150 mg every other day (further reduction may be needed); increase monitoring for adverse effects Rifampin: Concomitant use contraindicated |
|
Antiplatelet agents |
Potential for increased risk of bleeding |
Use concomitantly with caution |
|
Antipsychotics (lurasidone, pimozide, quetiapine) |
Lurasidone: Potential for serious and/or life-threatening adverse effects Pimozide: Potential for serious and/or life-threatening adverse effects (e.g., cardiac arrhythmias) Quetiapine: Increased quetiapine concentrations expected |
Lurasidone: Concomitant use contraindicated Pimozide: Concomitant use contraindicated Quetiapine: Consider alternative antiretroviral to avoid increased quetiapine exposures; if concomitant use necessary, consult quetiapine prescribing information for initial dosing; if initiating ritonavir-boosted tipranavir in patient receiving quetiapine, reduce quetiapine to one-sixth of original dosage |
|
Atazanavir |
Ritonavir-boosted tipranavir: Decreased atazanavir concentrations and AUC and increased tipranavir concentrations and AUC In vitro evidence of additive to antagonistic antiretroviral effects |
Atazanavir (with or without low-dose ritonavir): Concomitant use not recommended |
|
Benzodiazepines |
Midazolam, triazolam: Possible increased concentrations of midazolam or triazolam; potential for serious and/or life-threatening effects (e.g., prolonged or increased sedation or respiratory depression) |
Midazolam, triazolam: Concomitant use with oral midazolam or triazolam contraindicated; manufacturer states that parenteral midazolam can be used with caution in a monitored situation for procedural sedation; consider use of a reduced dose |
|
Buprenorphine, buprenorphine and naloxone |
Buprenorphine or fixed combination of buprenorphine and naloxone (buprenorphine/naloxone): Decreased tipranavir concentrations; no effect on clinical efficacy of buprenorphine/naloxone |
Buprenorphine or buprenorphine/naloxone: Dosage adjustments cannot be recommended |
|
Calcium-channel blocking agents (e.g., diltiazem, felodipine, nicardipine, nisoldipine, verapamil) |
Effect of ritonavir-boosted tipranavir on calcium channel blockers that are dual substrates of CYP3A and P-gp cannot be predicted |
Use concomitantly with caution; clinical monitoring recommended |
|
Colchicine |
Increased colchicine concentrations |
Patients with renal or hepatic impairment: Concomitant use with ritonavir-boosted tipranavir contraindicated Patients with normal renal or hepatic function: Dosage adjustments recommended when used with ritonavir-boosted tipranavir Colchicine for treatment of gout flares: In those receiving ritonavir-boosted tipranavir, use colchicine dose of 0.6 mg followed by 0.3 mg 1 hour later and repeat dose no earlier than 3 days later Colchicine for prophylaxis of gout flares: In those receiving ritonavir-boosted tipranavir, decrease colchicine dosage to 0.3 mg once daily in those originally receiving 0.6 mg twice daily or decrease dosage to 0.3 mg once every other day in those originally receiving 0.6 mg once daily Colchicine for treatment of familial Mediterranean fever (FMF): In those receiving ritonavir-boosted tipranavir, use maximum colchicine dosage of 0.6 mg daily (may be given as 0.3 mg twice daily) |
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Cisapride |
Potential for serious and/or life-threatening effects such as cardiac arrhythmias |
Concomitant use contraindicated |
|
Clarithromycin |
Increased clarithromycin concentrations; decreased hydroxyclarithromycin concentrations; increased tipranavir concentrations |
Modification of usual dosage of clarithromycin or tipranavir not necessary in patients with normal renal function; reduce clarithromycin dosage by 50% if Clcr 30–60 mL/minute and reduce by 75% if Clcr<30 mL/minute |
|
Delavirdine |
No antagonistic antiretroviral effects in vitro |
|
|
Didanosine |
Decreased didanosine concentrations when the delayed-release capsules are used No antagonistic antiretroviral effects in vitro |
For optimal absorption, administer didanosine at least 2 hours before or after tipranavir |
|
Disulfiram |
Potential pharmacokinetic interaction with alcohol contained in tipranavir capsules; possible disulfiram-like reaction |
|
|
Dolutegravir |
Decreased dolutegravir concentrations and AUC |
If used concomitantly, refer to the dolutegravir prescribing information |
|
Efavirenz |
Decreased tipranavir concentrations and no change in efavirenz concentrations using tipranavir 500 mg twice daily and ritonavir 100 mg twice daily with efavirenz 600 mg once daily No antagonistic antiretroviral effects in vitro |
|
|
Emtricitabine |
No antagonistic antiretroviral effects in vitro |
|
|
Enfuvirtide |
Increased tipranavir trough concentrations No antagonistic antiretroviral effects in vitro |
Dosage adjustments not recommended |
|
Ergot alkaloids (dihydroergotamine, ergonovine, ergotamine, methylergonovine) |
Potential for serious or life-threatening adverse effects (e.g., peripheral vasospasm, ischemia of extremities) |
Concomitant use contraindicated |
|
Estrogens and progestins |
Potential for increased risk of non-serious rash in women receiving estrogens Conjugated estrogens (equine or synthetic), estradiol: Possible decreased estrogen concentrations Oral contraceptives containing ethinyl estradiol and norethindrone: Decreased ethinyl estradiol concentrations; no effect on norethindrone concentrations |
Conjugated estrogens (equine or synthetic), estradiol: Monitor for estrogen deficiency; adjust dosage as clinically necessary Oral contraceptives containing ethinyl estradiol and norethindrone: Consider alternative nonhormonal or additional contraception methods |
|
Fosamprenavir |
Possible decreased amprenavir concentrations |
Concomitant use not recommended |
|
HMG-CoA reductase inhibitors (statins) |
Atorvastatin, lovastatin, rosuvastatin, simvastatin: Increased concentrations and AUCs of the antilipemic agent and increased risk of statin-associated adverse effects, including myopathy and rhabdomyolysis |
Atorvastatin: Avoid concomitant use Lovastatin: Concomitant use contraindicated Simvastatin: Concomitant use contraindicated |
|
Lamivudine |
No clinically important changes in lamivudine concentrations In vitro evidence of additive to antagonistic antiretroviral effects |
|
|
Loperamide |
Decreased loperamide concentrations; no clinically important change in tipranavir concentrations |
|
|
Lopinavir and ritonavir |
Fixed combination of lopinavir and ritonavir: Decreased lopinavir concentrations and AUC In vitro evidence of additive to antagonistic antiretroviral effects |
Lopinavir/ritonavir: Concomitant use not recommended |
|
Methadone |
Decreased methadone concentrations |
Methadone dosage adjustment may be necessary |
|
Metronidazole |
Potential interaction with alcohol present in tipranavir capsules; possible disulfiram-like reaction |
|
|
Nelfinavir |
No evidence of antagonistic antiretroviral effects in vitro |
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Nevirapine |
No clinically important effect on nevirapine concentrations; no evidence of antagonistic antiretroviral effects in vitro |
|
|
Omeprazole |
Decreased omeprazole concentrations; no change in tipranavir concentrations |
If concomitant use necessary, increased omeprazole dosage may be considered based on response |
|
Oral antidiabetic agents |
Glimepiride, glipizide, glyburide, pioglitazone, repaglinide: Potential for altered concentrations of antidiabetic agents |
Glimepiride, glipizide, glyburide, pioglitazone, repaglinide: Careful glucose monitoring warranted |
|
Raltegravir |
Decreased raltegravir concentrations and AUC |
Raltegravir 400 mg 2 times daily: Dosage adjustments not needed Other raltegravir regimens: Refer to prescribing information |
|
Rilpivirine |
Possible increased rilpivirine concentrations; not expected to affect tipranavir concentrations |
|
|
Ritonavir |
Increased tipranavir concentrations and AUC; concomitant low-dose ritonavir used to therapeutic advantage (ritonavir-boosted tipranavir) |
|
|
St. John’s wort (Hypericum perforatum) |
Potential decreased tipranavir concentrations; possible decreased antiretroviral efficacy and increased risk of antiretroviral resistance |
Concomitant use contraindicated |
|
Saquinavir |
Decreased saquinavir concentrations and AUC In vitro evidence of additive to antagonistic antiretroviral effects |
Concomitant use not recommended |
|
Selective serotonin-reuptake inhibitors (SSRIs) |
Fluoxetine, paroxetine, sertraline: Possible increased SSRI concentrations |
Dosage of the SSRI may need to be adjusted when ritonavir-boosted tipranavir is initiated |
|
Sildenafil |
Possible increased sildenafil concentrations and increased risk of sildenafil-associated adverse effects (e.g., hypotension, syncope, visual disturbances, prolonged erection) |
Sildenafil for treatment of pulmonary arterial hypertension (PAH): Concomitant use with ritonavir-boosted tipranavir contraindicated Sildenafil for treatment of erectile dysfunction: Do not exceed sildenafil dosage of 25 mg once every 48 hours; closely monitor for sildenafil-associated adverse effects (e.g., hypotension, syncope, visual disturbances, prolonged erection) |
|
Tadalafil |
Possible increased tadalafil concentrations with first dose and increased risk of tadalafil-associated adverse effects (e.g., hypotension, syncope, visual disturbances, prolonged erection) |
Tadalafil for treatment of PAH in patients who have been receiving ritonavir-boosted tipranavir for ≥1 week: Use initial tadalafil dosage of 20 mg once daily; if tolerated, may increase dosage to 40 mg once daily Ritonavir-boosted tipranavir in patients receiving tadalafil for PAH: Discontinue tadalafil for at least 24 hours prior to initiating ritonavir-boostedtipranavir; after ≥1 week of the antiretroviral agent, may resume tadalafil at dosage of 20 mg once daily and, if tolerated, may increase dosage to 40 mg once daily Tadalafil for treatment of erectile dysfunction: Do not exceed tadalafil dosage of 10 mg once every 72 hours; closely monitor for tadalafil-related adverse effects (e.g., hypotension, syncope, visual disturbances, prolonged erection, syncope) |
|
Tenofovir |
Decreased tenofovir concentrations and AUC; possible decreased tipranavir concentrations and AUC No antagonistic antiretroviral effects in vitro |
|
|
Trazodone |
Possible increased trazodone concentrations and AUC Increased risk of trazodone-associated adverse effects (e.g., nausea, dizziness, hypotension, syncope) |
Use with caution; consider reduced trazodone dosage |
|
Tricyclic antidepressants (desipramine) |
Desipramine: Possible increased concentrations of the tricyclic antidepressant |
Desipramine: Use reduced desipramine dosage and monitor plasma desipramine concentrations |
|
Valacyclovir |
No clinically important effect on tipranavir or acyclovir concentrations or AUC |
|
|
Vardenafil |
Possible increased vardenafil concentrations and increased risk of vardenafil-associated adverse effects (e.g., hypotension, syncope, visual disturbances, prolonged erection) |
Vardenafil for treatment of erectile dysfunction: Do not exceed vardenafil dosage of 2.5 mg once every 72 hours; closely monitor for vardenafil-related adverse effects (e.g., hypotension, syncope, visual changes, prolonged erection) |
|
Vitamin E |
Potential for increased risk of bleeding with high-dose vitamin E |
Use concomitantly with caution |
|
Zidovudine |
Decreased zidovudine AUC; clinical importance unknown No antagonistic antiretroviral effects in vitro |
Appropriate dosage for concomitant use not established |
Tipranavir Pharmacokinetics
Absorption
Bioavailability
Tipranavir is administered concomitantly with low-dose ritonavir (ritonavir-boosted tipranavir). Ritonavir decreases metabolism of tipranavir, resulting in increased tipranavir plasma concentrations.
Following >2 weeks of multiple oral doses given without regard to meals, peak plasma tipranavir concentrations attained approximately 3 hours after a dose.
Steady state attained in most patients after 7–10 days. Steady-state trough concentrations are 70% lower than day 1, presumably due to intestinal P-gp induction.
Food
Effect of food on administration of tipranavir with ritonavir (as tablets) not evaluated.
Distribution
Extent
Not known whether distributed into CSF or semen.
Not known whether distributed into human milk; distributed into animal milk.
Plasma Protein Binding
>99%.
Binds to albumin and α1-acid-glycoprotein.
Elimination
Metabolism
Tipranavir extensively metabolized by CYP3A4. Only minimal metabolism of tipranavir occurs when administered with ritonavir 200 mg.
Oral clearance of tipranavir decreased when administered with ritonavir; this may indicate decreased first-pass effect.
Elimination Route
Following administration of ritonavir-boosted tipranavir, eliminated principally in feces as unchanged tipranavir. Approximately 82% of tipranavir dose excreted in feces and 4% excreted in urine.
Half-life
Effective mean elimination half-life at steady-state is 4.8–6 hours following administration of ritonavir-boosted tipranavir with a light meal.
Special Populations
Renal impairment: Pharmacokinetics not studied, but decreased total body clearance not expected since renal clearance of tipranavir is negligible.
Mild hepatic impairment (Child-Pugh class A): Increased plasma concentrations, but dosage adjustments not needed.
Moderate or severe impairment (Child-Pugh class B and C): Pharmacokinetics not evaluated.
Higher tipranavir concentrations reported in females compared with males; dosage adjustments not required.
Stability
Storage
Oral
Capsules
2–8°C prior to opening bottle; after opening bottle, store at 20–25°C (excursions permitted to 15–30°C) and use within 60 days.
Actions
-
Tipranavir is administered in conjunction with low-dose ritonavir (ritonavir-boosted tipranavir). Tipranavir is extensively metabolized by CYP3A and ritonavir is a potent inhibitor of CYP3A. Concomitant use of these drugs results in decreased metabolism and increased plasma concentrations of tipranavir.
-
Antiretroviral activity is due to tipranavir.
-
Active against HIV-1.
-
Tipranavir inhibits replication of HIV-1 by interfering with HIV proteases.
-
Tipranavir-resistant HIV-1, including strains with decreased susceptibility to other HIV PIs, has been reported.
Advice to Patients
-
Advise patients of the critical nature of compliance with HIV therapy and importance of remaining under the care of a clinician. Stress importance of taking as prescribed; do not alter or discontinue antiretroviral regimen without consulting clinician.
-
Use tipranavir with low-dose ritonavir (ritonavir-boosted tipranavir); stress importance of using these 2 drugs in conjunction with other antiretrovirals.
-
Advise patients to take tipranavir at the same time as ritonavir with a meal.
-
If a dose is missed, the dose should be taken as soon as it is remembered and the next dose taken at the regularly scheduled time. If a dose is skipped, a double dose should not be taken to make up for the missed dose.
-
Stress importance of patients informing their clinician if they are allergic to sulfonamides.
-
Possibility of fatal or nonfatal intracranial hemorrhage. Stress importance of informing clinician if unusual or unexplained bleeding develops.
-
Advise patients that severe liver disease (including fatalities) has been reported. Stress importance of discontinuing ritonavir-boosted tipranavir and seeking medical attention if signs or symptoms of liver disease (fatigue, malaise, anorexia, nausea, jaundice, bilirubinuria, acholic stools, liver tenderness, hepatomegaly) occur.
-
Need for periodic clinical and laboratory monitoring, including liver function tests, prior to and during treatment. Stress importance of extra vigilance in patients with chronic HBV or HCV coinfection because of increased risk of hepatotoxicity.
-
Possibility of rash. Stress importance of discontinuing ritonavir-boosted tipranavir and seeking medical attention if rash with or without joint pain or stiffness, throat tightness, generalized itching, muscle aches, fever, redness, blisters, or skin peeling occurs.
-
Inform patients that redistribution/accumulation of body fat may occur with antiretroviral therapy and that the cause and long-term health effects of these conditions are not known at this time.
-
Stress importance of informing clinicians of existing or contemplated concomitant therapy, including prescription (e.g., PDE5 inhibitors) and over-the-counter (OTC) drugs (e.g., vitamin E supplements) and herbal products (e.g., St. John’s wort), and any concomitant illnesses.
-
Advise women to use a reliable nonhormonal (e.g., barrier) method of contraception due to the potential interaction with estrogen-based hormonal contraceptives.
-
Stress importance of women informing their clinicians if they are or plan to become pregnant or plan to breast-feed. Inform patients that an antiretroviral pregnancy registry is available that monitors fetal outcomes of infants exposed to tipranavir. Providers can register patients by calling the Antiretroviral Pregnancy Registry at 1-800-258-4263.
-
Inform patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
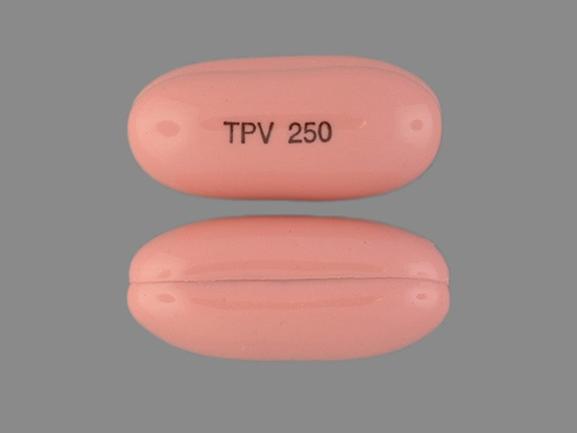
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules |
250 mg |
Aptivus |
Boehringer-Ingelheim |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions February 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
Biktarvy
Biktarvy is a complete HIV-1 treatment in a once-a-day single tablet containing three antiviral ...
Descovy
Descovy is used to treat and prevent HIV infection in adults and adolescents. When used for HIV-1 ...
Cabenuva
Cabenuva (cabotegravir and rilpivirine) injections are a long-acting HIV treatment used to keep HIV ...
Truvada
Truvada is used to prevent HIV (HIV PrEP) or treat HIV-1 infection in combination with other HIV-1 ...
Atripla
Atripla prevents the human immunodeficiency virus (HIV) from reproducing in your body. Learn about ...
Complera
Complera (emtricitabine, rilpivirine, and tenofovir) is used to treat HIV infection. Includes ...
Stribild
Stribild (cobicistat, elvitegravir, emtricitabine and tenofovir) is used to treat HIV-1 infection ...
Epzicom
Epzicom is used to treat HIV, which causes the acquired immunodeficiency syndrome (AIDS). Learn ...
Emtricitabine
Emtricitabine is used for HIV Infection, nonoccupational exposure, occupational exposure
More about tipranavir
- Check interactions
- Compare alternatives
- Side effects
- Dosage information
- During pregnancy
- Drug class: protease inhibitors
- Breastfeeding
- En español