Ospemifene (Monograph)
Brand name: Osphena
Drug class: Estrogen Agonists-Antagonists
Chemical name: 2-[4-[(1Z)-4-Chloro-1,2-diphenyl-1-butenyl]phenoxy]-ethanol
Molecular formula: C24H23ClO2
CAS number: 128607-22-7
Warning
-
Has estrogen agonistic effects on endometrium. Increased risk of endometrial cancer in postmenopausal women with an intact uterus who use estrogens alone. (See GU Effects under Cautions.)
-
Increased risk of stroke and DVT observed in postmenopausal women receiving daily dosages of oral conjugated estrogens alone as part of Woman's Health Initiative (WHI) study. (See Contraindications and Cardiovascular Effects under Cautions.)
-
Prescribe for shortest duration consistent with treatment goals and risks for the individual woman.
Introduction
Tissue-selective, estrogen agonist-antagonist; triphenylethylene derivative.
Uses for Ospemifene
Dyspareunia
Treatment of moderate to severe dyspareunia, a symptom of vulvar and vaginal atrophy, associated with menopause.
Ospemifene Dosage and Administration
General
-
Has estrogen agonistic effects on endometrium; consider concomitant use of progestin therapy to reduce risk of endometrial cancer in postmenopausal women with an intact uterus. (See GU Effects under Cautions.)
-
Use for shortest duration consistent with treatment goals and risks for the individual woman. Reevaluate patients periodically to determine if continued treatment is necessary.
Administration
Oral Administration
Administer orally with food.
Dosage
Adults
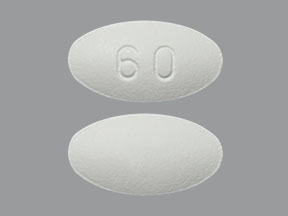
Dyspareunia
Oral
60 mg once daily.
Special Populations
Hepatic Impairment
Mild or moderate hepatic impairment (Child-Pugh class A or B): No dosage adjustments needed.
Severe hepatic impairment (Child-Pugh class C): Not studied; avoid use. (See Hepatic Impairment under Cautions.)
Renal Impairment
No dosage adjustments needed.
Cautions for Ospemifene
Contraindications
-
Undiagnosed abnormal genital bleeding.
-
Known or suspected estrogen-dependent neoplasia.
-
Active DVT, PE, or history of these conditions.
-
Active arterial thromboembolic disease (e.g., stroke, MI) or history of these conditions.
-
Women who are or may become pregnant. (See Fetal/Neonatal Morbidity and Mortality under Cautions.)
Warnings/Precautions
Warnings
Cardiovascular Effects
Increased risk of stroke and venous thromboembolism (VTE) observed in postmenopausal women receiving daily dosages of oral conjugated estrogen alone in Woman's Health Initiative (WHI) study. Increased incidence of stroke and DVT also observed in women receiving ospemifene 60 mg daily compared with those receiving placebo.
Discontinue drug immediately if VTE, thromboembolic stroke, or hemorrhagic stroke occurs or is suspected.
Discontinue at least 4–6 weeks prior to surgery associated with increased risk of thromboembolism or during periods of prolonged immobilization, if possible.
Manage risk factors appropriately for cardiovascular disorders, arterial vascular disease (e.g., hypertension, diabetes mellitus, tobacco use, hypercholesterolemia, obesity), and/or VTE (e.g., personal or family history of VTE, obesity, systemic lupus erythematosus).
GU Effects
Increased risk of endometrial cancer reported in postmenopausal women with an intact uterus who use estrogen alone. Adding progestin to estrogen reduces risk of endometrial hyperplasia; other possible risks (e.g., breast cancer) associated with combined use of progestin and estrogen compared with estrogen therapy alone. Concomitant use of progestin therapy with ospemifene not evaluated.
Endometrial cancer not reported in patients receiving ospemifene 60 mg daily (up to 52 weeks); one case of simple hyperplasia without atypia reported. Endometrial thickening, proliferative endometrium, and uterine polyps observed.
Clinical surveillance important for all women receiving ospemifene. Rule out malignancy in postmenopausal women with undiagnosed persistent or recurrent abnormal genital bleeding.
Other Warnings/Precautions
Breast Cancer
Not adequately studied in women with breast cancer; do not use in women with known or suspected breast cancer or with history of breast cancer.
Fetal/Neonatal Morbidity and Mortality
May cause fetal harm; embryofetal deaths demonstrated in animals. Reproductive effects consistent with estrogen-receptor activity of ospemifene.
If used during pregnancy or if patient becomes pregnant, apprise of potential fetal hazard.
Contraindicated in women who are or may become pregnant.
Specific Populations
Pregnancy
Category X. (See Fetal/Neonatal Morbidity and Mortality under Cautions.)
Lactation
Distributed into milk in rats; not known whether distributed into human milk.
Pediatric Use
Not indicated in pediatric patients; not studied in this age group.
Geriatric Use
No substantial differences in safety and efficacy in women ≥65 years of age relative to younger women.
Hepatic Impairment
Mild or moderate hepatic impairment (Child-Pugh class A or B): No dosage adjustments needed. (See Special Populations under Pharmacokinetics.)
Severe hepatic impairment (Child-Pugh class C): Not studied; do not use in such patients.
Renal Impairment
Dosage adjustment not required.
Common Adverse Effects
Hot flush, vaginal discharge, genital discharge, muscle spasms, hyperhidrosis.
Drug Interactions
Metabolized mainly in the liver by CYP isoenzymes 3A4 and 2C9; other CYP isoenzymes (2C19, 2B6) also involved in metabolism.
Weak inhibitor of CYP2B6, 2C9, 2C19, 2C8, 2D6, and 3A4 in vitro.
Not a clinically important substrate for P-glycoprotein (P-gp) transport system in vitro.
Drugs Affecting or Metabolized by Hepatic Microsomal Enzymes
Inhibitors (potent or moderate) of CYP3A4, 2C9, and/or 2C19: Possible pharmacokinetic interaction (increased plasma concentrations and AUC of ospemifene). Concomitant use with drugs that inhibit both CYP3A4 and 2C9 may increase risk of ospemifene-related adverse reactions.
Inducers (potent or moderate) of CYP3A4, 2C9, and/or 2C19: Possible pharmacokinetic interaction (decreased plasma concentrations and AUC of ospemifene). Concomitant use may decrease efficacy of ospemifene.
Substrates of CYP2B6, 2C9, 2C19, 2C8, 2D6, and 3A4: Clinically important pharmacokinetic interactions unlikely.
Protein-bound Drugs
Concomitant use with other highly protein-bound drugs may lead to increased exposure of ospemifene or the other drug.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Antifungals, azoles (e.g., fluconazole, ketoconazole) |
Increased ospemifene exposure; may increase risk of ospemifene-related adverse reactions |
Fluconazole: Avoid concomitant use Ketoconazole: Use concomitantly with caution |
|
Antimycobacterials, rifamycins (e.g., rifampin) |
Rifampin: Decreased ospemifene exposure; may decrease efficacy of ospemifene |
|
|
Bupropion |
No clinically important effects on bupropion pharmacokinetics |
|
|
Estrogen and estrogen agonist-antagonists |
Safety of concomitant use not studied |
Avoid concomitant use |
|
Proton-pump Inhibitors (e.g., omeprazole) |
Omeprazole: No clinically important effects on omeprazole pharmacokinetics; slight increase in ospemifene exposure |
|
|
Quinidine |
No clinically important effects on ospemifene pharmacokinetics |
|
|
Warfarin |
No clinically important effects on warfarin pharmacokinetics following single 10-mg dose of warfarin Effects on PT and INR not studied |
Ospemifene Pharmacokinetics
Absorption
Bioavailability
Absolute bioavailability not evaluated; rapidly absorbed following oral administration.
Peak serum concentrations attained approximately 2.5 hours following administration of a single 60-mg dose with high-fat, high-calorie meal.
Food
Administration with food increases bioavailability twofold to threefold.
Special Populations
Mild or moderate hepatic impairment (Child-Pugh class A or B) does not substantially alter peak concentration and AUC. Pharmacokinetics not studied in patients with severe hepatic impairment (Child-Pugh class C). (See Hepatic Impairment under Cautions.)
Severe renal impairment (i.e., Clcr <30 mL/minute) does not substantially alter peak concentration and AUC.
Distribution
Extent
Distributed into milk in rats; not known whether distributed into human milk.
Plasma Protein Binding
>99%.
Elimination
Metabolism
Metabolized mainly in the liver by CYP isoenzymes 3A4 and 2C9; other isoenzymes (CYP2C19 and 2B6) also involved in metabolism. Major metabolite is 4-hydroxyospemifene.
Elimination Route
Excreted in feces (75%) and urine (7%).
Half-life
Approximately 26 hours.
Stability
Storage
Oral
Tablets
20–25°C (may be exposed to 15–30°C).
Actions
-
Tissue-selective, estrogen agonist-antagonist; also referred to as a selective estrogen receptor modulator (SERM).
-
Binds to estrogen receptor (ER)α and ERβ; stronger binding occurs at ERα receptor.
-
Activates estrogenic pathways in some tissues and blocks estrogenic pathways in other tissues.
-
Exhibits strong estrogenic effects on vaginal epithelium (e.g., improvements in maturation index, vaginal pH, symptoms of menopause [e.g., dyspareunia, vaginal dryness]).
-
In animal studies, estrogenic effects on bone observed. In healthy postmenopausal women, reduced biochemical markers of bone turnover observed. Further studies needed to evaluate effects on bone mineral density (BMD) and fracture risk.
-
No substantial effects on serum lipoprotein concentrations (i.e., total, LDL-, or HDL-cholesterol; triglycerides).
-
Weak estrogenic effects on endometrial tissue; slight dose-related mean increase in endometrial thickness, but no cases of endometrial cancer observed. (See GU Effects under Cautions.)
-
Preclinical data show possible antiestrogenic activity in several breast cancer models; such effects not assessed in clinical trials. (See Breast Cancer under Cautions.)
Advice to Patients
-
Importance of instructing patients to read the manufacturer's patient information prior to initiation of therapy and each time the prescription is refilled.
-
Importance of advising patients that ospemifene may initiate or increase occurrence of hot flushes in some women.
-
Importance of reporting any unusual vaginal bleeding to a clinician as soon as possible.
-
Importance of informing a clinician of any current or previous occurrence of cancer, VTE, stroke, or MI.
-
Importance of informing a clinician of any impending surgery or prolonged bed rest.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed. Advise pregnant women of risk to fetus.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
60 mg |
Osphena |
Shionogi |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions May 21, 2014. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
More about ospemifene
- Check interactions
- Compare alternatives
- Reviews (45)
- Side effects
- Dosage information
- During pregnancy
- Drug class: selective estrogen receptor modulators
- En español