Griseofulvin (Monograph)
Brand names: Grifulvin V, Gris-PEG
Drug class: Antifungals, Miscellaneous
VA class: AM700
CAS number: 126-07-8
Introduction
Antifungal antibiotic produced by Penicillium.
Uses for Griseofulvin
Dermatophytoses
Treatment of dermatophytoses of the skin, scalp, and nails, including tinea barbae (ringworm of bearded areas of face and neck), tinea capitis (scalp ringworm), tinea corporis (ringworm of the body), tinea cruris (jock itch; groin ringworm), tinea pedis (athlete’s foot, foot ringworm), and tinea unguium (onychomycosis; nail ringworm) caused by Trichophyton, Microsporum, or Epidermophyton floccosum.
A drug of choice for treatment of tinea capitis; prolonged therapy usually is necessary to cure the infection and poor compliance may affect response to the drug. Tinea barbae and tinea capitis generally require treatment with an oral antifungal.
Tinea corporis and tinea cruris generally can be effectively treated using a topical antifungal; an oral antifungal may be necessary if the disease is extensive, dermatophyte folliculitis is present, the infection does not respond to topical therapy, or the patient is immunocompromised or has coexisting disease (e.g., diabetes mellitus).
While topical antifungals usually are effective for treatment of acute, uncomplicated tinea manuum and tinea pedis, an oral antifungal usually is necessary for treatment of severe, chronic, or recalcitrant tinea pedis, chronic moccasin-type (dry-type) tinea pedis, and for treatment of tinea unguium (onychomycosis).
Griseofulvin Dosage and Administration
Administration
Oral Administration
Administer orally.
When microsize griseofulvin (Grifulvin V) tablets are used, absorption may be improved if given after a high-fat meal.
Dosage
Dosage varies depending on whether the drug is administered as griseofulvin microsize (Grifulvin V) or griseofulvin ultramicrosize (Gris-PEG).
Dosage and duration of treatment should be individualized according to the requirements and response of the patient. Griseofulvin generally should be continued for ≥4–12 weeks for treatment of tinea capitis; ≥2–4 weeks for treatment of tinea corporis; ≥4–8 weeks for tinea pedis; and from 4–6 months to a year or longer for tinea unguium.
Pediatric Patients
Dermatophytoses
Microsize (Grifulvin V)
Oral10–11 mg/kg daily, although dosages up to 20–25 mg/kg daily have been used.
Manufacturer suggests that those weighing approximately 14–23 kg may receive 125–250 mg daily and that those weighing >23 kg may receive 250–500 mg daily.
AAP recommends 10–20 mg/kg (maximum 1 g) daily in 1 or 2 doses. For tinea capitis, AAP recommends 15–20 mg/kg once daily.
Ultramicrosize (Gris-PEG)
OralChildren >2 years of age: Usually 7.3 mg/kg daily, although dosages up to 10–15 mg/kg daily have been used.
Manufacturer suggests that those weighing approximately 16–27 kg may receive 125–187.5 mg daily and those weighing >27 kg may receive 187.5–375 mg daily.
AAP recommends 5–10 mg/kg (maximum 750 mg) once daily.
Adults
Dermatophytoses
Microsize (Grifulvin V)
Oral500 mg daily for treatment of tinea capitis, tinea corporis, or tinea cruris. For more difficult infections (e.g., tinea pedis, tinea unguium), 1 g daily.
Ultramicrosize (Gris-PEG)
Oral375 mg once daily or in divided doses for treatment of tinea capitis, tinea corporis, or tinea cruris. For more difficult infections (e.g., tinea pedis, tinea unguium), 750 mg daily given in divided doses.
Cautions for Griseofulvin
Contraindications
-
Hypersensitivity to griseofulvin.
-
Porphyria or hepatocellular failure.
-
Pregnant women. (See Fetal/Neonatal Morbidity and Mortality under Cautions.)
Warnings/Precautions
Warnings
Fetal/Neonatal Morbidity and Mortality
May cause fetal toxicity when administered to pregnant women.
Some animal studies indicate that griseofulvin may be embryotoxic and teratogenic. There have been 2 cases of conjoined twins born to women who received griseofulvin during the first trimester of pregnancy; some women who received the drug during pregnancy reportedly have had spontaneous abortions or delivered infants with other congenital malformations.
Griseofulvin should not be used in women who are pregnant or intend to become pregnant within 1 month after treatment.
Women should use additional contraceptive precautions during griseofulvin treatment and for 1 month after the drug is discontinued. One manufacturer recommends that men wait at least 6 months after completing griseofulvin treatment before fathering a child.
If a patient becomes pregnant while receiving griseofulvin, they should be advised of the potential hazard to the fetus.
Sensitivity Reactions
Hypersensitivity Reactions
Hypersensitivity reactions (e.g., rash, urticaria, erythema multiforme-like reactions, angioneurotic edema) have been reported.
Because griseofulvin is derived from Penicillium, there is a possibility of cross-sensitivity with penicillin. Patients with known penicillin hypersensitivity have received griseofulvin without such reactions.
If hypersensitivity reaction occurs, discontinue griseofulvin and initiate appropriate therapy.
Photosensitivity Reactions
Photosensitivity reactions have been reported. Lupus erythematosus may be aggravated if a photosensitivity reaction occurs.
Avoid exposure to intense natural or artificial sunlight during griseofulvin treatment.
General Precautions
Selection and Use of Antifungals
Prior to administration of griseofulvin for dermatophytoses, diagnosis should be confirmed either by direct microscopic examination of scrapings from infected tissue mounted in potassium hydrochloride (KOH) or by culture.
Should not be used for treatment of minor or trivial dermatophytoses that may respond to topical antifungals alone.
General hygiene measures should be observed to control sources of infection or reinfection. Concomitant use of topical antifungals or antibacterials may be required, particularly for treatment of tinea pedis (athlete’s foot, foot ringworm). In some forms of tinea pedis, yeasts and bacteria may also be involved and griseofulvin is ineffective against these organisms.
Not effective and should not be used for treatment of pityriasis (tinea) versicolor or cutaneous Candida infections.
Not effective and should not be used for treatment of systemic fungal infections, including blastomycosis, candidiasis, chromoblastomycosis, coccidioidomycosis, cryptococcosis, histoplasmosis, or sporotrichosis. Safety and efficacy not established for prevention of fungal infections.
Not effective and should not be used for treatment of bacterial infections, including actinomycosis or nocardiosis.
Laboratory Monitoring
Periodically assess organ system functions, including renal, hepatic, and hematopoietic, during prolonged therapy.
Specific Populations
Pregnancy
Category C. (See Fetal/Neonatal Morbidity and Mortality under Cautions.)
Pediatric Use
Safety and efficacy of ultramicrosize griseofulvin not established in children ≤2 years of age. Microsize griseofulvin has been used in children as young as 3 months of age.
Hepatic Impairment
Contraindicated in patients with hepatocellular failure.
Common Adverse Effects
Hypersensitivity reactions (rash, urticaria); GI effects (oral thrush, nausea, vomiting, epigastric distress, diarrhea); CNS effects (headache, fatigue, dizziness, insomnia, mental confusion, impaired performance of routine activities).
Drug Interactions
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Alcohol |
Tachycardia, flushing, and potentiation of alcohol effects has been reported in patients receiving griseofulvin |
Although clinical importance is unclear, some clinicians suggest that patients be warned of a possible reaction and to avoid alcohol during griseofulvin therapy |
|
Anticoagulants, oral (warfarin) |
Decreased PT reported |
Use concomitantly with caution; adjust anticoagulant dosage if needed during and after griseofulvin treatment |
|
Aspirin |
Possible decreased plasma salicylate concentrations |
|
|
Barbiturates |
Possible decreased antifungal activity Phenobarbital: Possible decreased griseofulvin concentrations |
Dosage adjustment of griseofulvin may be necessary Phenobarbital: Avoid concomitant use; if concomitant use is necessary, administer griseofulvin in 3 divided doses daily to maximize absorption, monitor griseofulvin concentrations, and adjust dosage of the antifungal if necessary |
|
Cyclosporine |
Possible decreased concentrations of cyclosporine |
|
|
Hormonal contraceptives (oral contraceptives) |
Amenorrhea, increased breakthrough bleeding, and possibility of decreased contraceptive efficacy reported with concomitant use |
The possibility of decreased contraceptive efficacy should be considered if griseofulvin is used concomitantly |
|
Theophylline |
Increased clearance and decreased theophylline half-life reported in some patients; extent of this interaction appears to vary and increased clearance of theophylline is not evident in all individuals who receive the drugs concomitantly |
Griseofulvin Pharmacokinetics
Absorption
Bioavailability
Absorption of microsize griseofulvin is variable and unpredictable and ranges from 25–70% of an oral dose; peak serum concentrations attained 4 hours after a dose.
Ultramicrosize griseofulvin is almost completely absorbed following oral administration.
Food
Absorption of microsize griseofulvin may be enhanced by administration after a high-fat meal.
Distribution
Extent
Following oral absorption, griseofulvin is concentrated in skin, hair, nails, liver, fat, and skeletal muscles. The drug can be detected in the outer layers of the stratum corneum soon after ingestion.
Griseofulvin is deposited in keratin precursor cells and has greater affinity for diseased tissue. The drug is tightly bound to new keratin.
Griseofulvin concentrations in skin are higher in warm climates than in cold, possibly because the drug is dissolved in perspiration and deposited in the horny layer of skin when perspiration evaporates. This explanation has also been used to account for the reversed concentration gradient of the drug in skin; highest concentrations are found in the outermost horny layer, while concentrations are much lower in deeper layers.
Elimination
Metabolism
Oxidatively demethylated and conjugated with glucuronic acid, principally in the liver. The major metabolite, 6-desmethylgriseofulvin, is microbiologically inactive.
Elimination Route
About 30% of a single oral dose of microsize griseofulvin is excreted in urine within 24 hours as 6-desmethylgriseofulvin and its glucuronide conjugate; 50% of the dose is excreted in urine within 5 days. Unchanged griseofulvin in the urine accounts for <1% of the administered drug. Approximately one-third of a single dose of microsize griseofulvin is excreted in feces within 5 days. Griseofulvin also is excreted in perspiration.
Half-life
9–24 hours.
Stability
Storage
Oral
Tablets
Microsize or ultramicrosize: 15–30°C in tight, light-resistant container.
Suspension
Microsize: Room temperature in tight, light-resistant container.
Actions and Spectrum
-
Structurally unrelated to other antifungals (e.g., allylamines, azoles, echinocandins, polyenes, pyrimidines).
-
Usually fungistatic in action.
-
Antifungal activity principally involves disruption of the fungal cell’s mitotic spindle structure. Although the effect on mitosis is similar to that caused by colchicine, a different mechanism is probably involved. Griseofulvin may cause production of defective DNA which is unable to replicate.
-
Griseofulvin is deposited in keratin precursor cells and is tightly bound to new keratin, resulting in an environment unfavorable for fungal invasion. Infected skin, hair, or nails are then replaced with tissue not infected with the dermatophyte.
-
Limited spectrum of antifungal activity. Active against most dermatophytes, but not active against yeasts or other fungi, including Aspergillus, Blastomyces, Candida, Cryptococcus, Coccidioides, Histoplasma, Saccharomyces, Sporotrichum, or Malassezia furfur (Pityrosporum orbiculare).
-
Dermatophytes: Active against Epidermophyton floccosum, Microsporum audouini, M. canis, M. gypseum, Trichophyton crateriform, T. gallinae, T. interdigitalis, T. megnini, T. mentagrophytes, T. rubrum, T. schoenleinii, T. sulphureum, T. tonsurans, and T. verrucosum.
Advice to Patients
-
Importance of using griseofulvin for the full, prescribed treatment period, even if symptoms improve; importance of consulting with clinician if the condition does not improve after a full course of therapy.
-
Advise patients to avoid exposure to intense natural or artificial sunlight during griseofulvin treatment since photosensitivity reactions can occur.
-
Importance of discontinuing use and contacting clinician if signs or symptoms of sensitization occur (e.g., rash, urticaria).
-
Importance of informing clinicians of existing or contemplated therapy, including prescription and OTC drugs, as well as any concomitant illnesses.
-
Importance of women informing clinicians if they are or plan to become pregnant or to breast-feed. (See Fetal/Neonatal Morbidity and Mortality under Cautions.)
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Suspension |
125 mg/5 mL |
Grifulvin V (with alcohol 0.2% parabens and propylene glycol) |
Ortho-Neutrogena |
|
Tablets |
500 mg |
Grifulvin V (scored) |
Ortho-Neutrogena |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
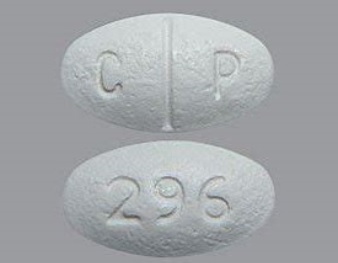
Tablets, film-coated |
125 mg |
Gris-PEG (with methylparaben; scored) |
Pedinol |
|
250 mg |
Gris-PEG (with methylparaben and povidone; scored) |
Pedinol |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions July 1, 2006. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
More about griseofulvin
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (15)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: miscellaneous antifungals
- En español
Patient resources
Professional resources
- Griseofulvin prescribing information
- Griseofulvin Tablets (FDA)
- Griseofulvin Ultramicrosize Tablets (FDA)