C1 Inhibitor (Recombinant)
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
Pronunciation
(cee won in HIB i ter ree KOM be nant)
Index Terms
- C1 Esterase Inhibitor
- C1-INH
- C1-Inhibitor
- Conestat Alfa
- Recombinant C1 Inhibitor
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
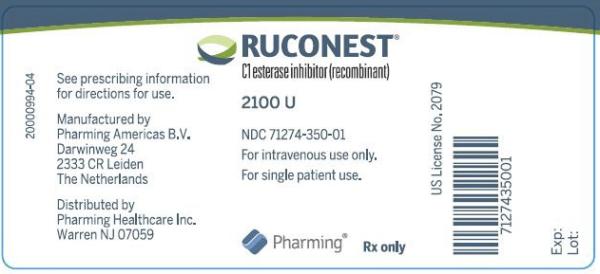
Solution Reconstituted, Intravenous [preservative free]:
Ruconest: 2100 units (1 ea) [contains rabbit protein]
Brand Names: U.S.
- Ruconest
Pharmacologic Category
- C1 Esterase Inhibitor
Pharmacology
C1 inhibitor, a serine protease inhibitor (serpin), regulates the activation of the complement and contact system pathways by irreversibly binding target proteases. Suppression of contact system activation by C1 inhibitor through the inactivation of plasma kallikrein and factor XIIa is thought to modulate vascular permeability that leads to clinical manifestations of hereditary angioedema (HAE) attacks by preventing the generation of bradykinin.
Distribution
Vss: ~3 L
Onset of Action
Onset of symptom relief: Median: 90 minutes
Time to Peak
~0.3 hours
Half-Life Elimination
~2.5 hours
Use: Labeled Indications
Hereditary angioedema (treatment): Treatment of acute attacks of hereditary angioedema (HAE) in adult and adolescent patients
Limitations of use: Effectiveness not established in HAE patients with laryngeal attacks.
Off Label Uses
Hereditary angioedema (prophylaxis)
Data from a small pilot study displayed a significant reduction in hereditary angioedema (HAE) attacks after weekly administration of C1 inhibitor (recombinant) [Reshef 2013]. Subsequently, a small international phase II multicenter randomized double-blind placebo controlled crossover trial further supported the use of C1 inhibitor (recombinant) for prophylaxis of HAE in patients with frequent attacks (defined as a history of ≥4 HAE attacks per month for at least 3 consecutive months) and C1 inhibitor levels <50% of normal. Both weekly and twice-weekly administration of C1 inhibitor (recombinant) significantly reduced the number of HAE attacks after 4 weeks of therapy compared with placebo; however, the twice-weekly regimen resulted in more consistent achievement of at least 50% reduction in attacks [Riedl 2017].
Based on the International World Allergy Organization/European/Academy of Allergy and Clinical Immunology (WAO/EAACI) guideline for the management of hereditary angioedema, C1 inhibitor (recombinant) may be considered for short-term prophylaxis before procedures that induce an attack.
Contraindications
Life-threatening immediate hypersensitivity reactions, including anaphylaxis, to C1 esterase inhibitor preparations or any component of the formulation; allergy to rabbits or rabbit-derived products. Note: Patients with a clinical history of a rabbit allergy and/or cow's milk allergy who are negative on skin testing to C1 inhibitor (recombinant) have tolerated a subcutaneous challenge of C1 inhibitor (recombinant) (van den Elzen 2016).
Dosing: Adult
Hereditary angioedema (treatment): IV:
Weight <84 kg: 50 units/kg (maximum dose: 4,200 units) as a single dose
Weight ≥84 kg: 4,200 units as a single dose
Note: If attack symptoms persist, one additional dose may be administered; no more than 2 doses may be administered per 24 hours.
Hereditary angioedema (prophylaxis) (off-label use): IV:
Weight <84 kg: 50 units/kg (maximum dose: 4,200 units) twice weekly (Riedl 2017)
Weight ≥84 kg: 4,200 units twice weekly (Riedl 2017)
Note: May reduce frequency of administration to once weekly, ensuring maintenance of symptom control; once-weekly dosing was shown to be more effective than placebo but with the potential for more frequent attacks compared with twice-weekly dosing (Reshef 2013, Riedl 2017). Dosing more than twice weekly has not been studied.
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Hereditary angioedema (HAE), prophylaxis: Limited data available (Riedl 2017):
Adolescents ≥13 years:
<84 kg: IV: 50 units/kg twice weekly; maximum dose: 4,200 units/dose.
≥84 kg: IV: 4,200 units twice weekly.
Note: Dosing based on a small multinational phase II randomized double-blind placebo-controlled crossover trial in patients with frequent attacks (defined as a history of ≥4 HAE attacks per month for ≥3 consecutive months) and C1 inhibitor levels <50% of normal. Both weekly and twice-weekly administration of C1 inhibitor (recombinant) significantly reduced the number of HAE attacks after 4 weeks of therapy compared with placebo; however, the twice-weekly regimen resulted in more consistent achievement of ≥50% reduction in attacks (Riedl 2017). May reduce frequency of administration to once weekly, ensuring maintenance of symptom control; once-weekly dosing was shown to be more effective than placebo but with the potential for more frequent attacks compared with twice-weekly dosing (Reshef 2013; Riedl 2017).
Hereditary angioedema (HAE), treatment of acute attacks (non-laryngeal):
Children ≥5 years: Limited data available: IV: 50 units/kg as a single dose, maximum dose: 4,200 units/dose. Dosing based on a small open-label phase II multinational study (n=20 subjects accounting for 73 HAE attacks; age range: 5 to 14 years); approximately 96% (70/73) HAE attacks were treated with a single dose; time to beginning of symptom relief occurred in a median of 60 minutes and time to minimal symptoms occurred in a median of 122.5 minutes; instances of multiple doses included: 1 patient received a second dose during 1 attack and another received a second dose during 2 separate attacks for persistent symptoms; treatment was well-tolerated overall (Reshef 2019).
Adolescents: Note: Unlike human C1 inhibitors, efficacy not established in patients with laryngeal attacks due to a limited number of patients; in some trials, patients with laryngeal attacks were excluded (Valerieva 2018; manufacturer's labeling).
Initial dosing:
<84 kg: IV: 50 units/kg as a single dose, maximum dose: 4,200 units/dose.
≥84 kg: IV: 4,200 units as a single dose.
Redosing: If attack symptoms persist, 1 additional dose may be administered; no more than 2 doses may be administered per 24 hours. In trials, patients were administered a second dose 4 hours after the initial dose if relief not achieved; median time to minimal symptoms was about 5 hours (range: 4 to 12 hours) (Riedl 2014).
Reconstitution
Allow diluent and C1 inhibitor to warm to room temperature. Reconstitute with 14 mL SWFI. Slowly add SWFI and swirl slowly to mix; avoid foaming. Resulting concentration is 150 units/mL. If patient requires contents of ≥1 vial, contents of multiple vials may be pooled into a single syringe.
Administration
IV: Administer by a separate infusion line as a slow IV injection over ~5 minutes. Appropriately trained patients may self-administer upon recognition of an HAE attack.
Storage
Store intact vials at 2°C to 25°C (36°F to 77°F) for up to 48 months; do not freeze. Protect from light. Reconstituted solution may be stored at 2°C to 8°C (36°F to 46°F) for ≤8 hours; do not freeze. Discard unused portion.
Drug Interactions
Androgens: May enhance the thrombogenic effect of C1 inhibitors. Monitor therapy
Estrogen Derivatives: May enhance the thrombogenic effect of C1 inhibitors. Monitor therapy
Progestins: May enhance the thrombogenic effect of C1 inhibitors. Monitor therapy
Adverse Reactions
The following adverse drug reactions and incidences are derived from product labeling unless otherwise specified.
>10%: Immunologic: Antibody development (6% to ≤17%; anti-C1INH, anti-rhC1INH, and anti-host-related impurities)
1% to 10%:
Central nervous system: Headache (10%; includes procedural headache), vertigo (3%)
Dermatologic: Burning sensation of skin (2%), erythema (2%; marginatum)
Gastrointestinal: Diarrhea (≥2%), nausea (≥2%)
Hematologic & oncologic: C-reactive protein increased (2%), increased serum fibrinogen (fibrin D-dimer: 2%), lipoma (2%)
Hypersensitivity: Angioedema (3%)
Neuromuscular & skeletal: Back pain (3%)
Respiratory: Sneezing (2%)
<1%, postmarketing and/or case reports: Anaphylaxis
Related/similar drugs
Warnings/Precautions
Concerns related to adverse effects:
• Hypersensitivity: Severe hypersensitivity reactions (eg, urticaria, hives, tightness of the chest, wheezing, hypotension, anaphylaxis) may occur during or after administration. Signs/symptoms of hypersensitivity reactions may be similar to the attacks associated with hereditary angioedema, therefore, consideration should be given to treatment methods. In the event of acute hypersensitivity reactions to C1 inhibitor therapy, treatment should be discontinued and appropriate treatment should be instituted.
• Thrombotic events: Serious arterial and venous thromboembolic events have been reported at recommended doses in patients with risk factors (eg, presence of an indwelling venous catheter/access device, prior history of thrombosis, underlying atherosclerosis, use of oral contraceptives or certain androgens, morbid obesity, immobility). Closely monitor patients with preexisting risks for thrombotic events during and after administration.
Monitoring Parameters
Monitor for signs/symptoms of hypersensitivity reactions and thrombotic events. Prior to initiation for long-term prophylaxis, test for immunoglobulin E (IgE) antibodies against rabbit antigens; repeat testing annually or after 10 treatments, whichever occurs first (Craig 2012).
Pregnancy Considerations
Information related to use of C1 inhibitor (recombinant) in pregnancy is limited (Longhurst 2018).
C1 inhibitor (human) is preferred for the treatment and prophylaxis of hereditary angioedema (HAE) during pregnancy. Women with HAE should be monitored closely during pregnancy and for at least 72 hours after delivery (WAO/EEACI [Maurer 2018]).
Patient Education
What is this drug used for?
• It is used to treat swelling attacks in people with hereditary angioedema (HAE).
All drugs may cause side effects. However, many people have no side effects or only have minor side effects. Call your doctor or get medical help if any of these side effects or any other side effects bother you or do not go away:
• Diarrhea
• Nausea
WARNING/CAUTION: Even though it may be rare, some people may have very bad and sometimes deadly side effects when taking a drug. Tell your doctor or get medical help right away if you have any of the following signs or symptoms that may be related to a very bad side effect:
• Weakness on 1 side of the body, trouble speaking or thinking, change in balance, drooping on one side of the face, or blurred eyesight
• Severe dizziness
• Passing out
• Mouth discoloration
• Fast heartbeat
• Severe headache
• Blood clots like numbness or weakness on one side of the body; pain, redness, tenderness, warmth, or swelling in the arms or legs; change in color of an arm or leg; chest pain; shortness of breath; fast heartbeat; or coughing up blood
• Signs of an allergic reaction, like rash; hives; itching; red, swollen, blistered, or peeling skin with or without fever; wheezing; tightness in the chest or throat; trouble breathing, swallowing, or talking; unusual hoarseness; or swelling of the mouth, face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a limited summary of general information about the medicine's uses from the patient education leaflet and is not intended to be comprehensive. This limited summary does NOT include all information available about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not intended to provide medical advice, diagnosis or treatment and does not replace information you receive from the healthcare provider. For a more detailed summary of information about the risks and benefits of using this medicine, please speak with your healthcare provider and review the entire patient education leaflet.
Biological Products Related to conestat alfa
Find detailed information on biosimilars for this medication.
More about conestat alfa
- Check interactions
- Compare alternatives
- Reviews (3)
- Side effects
- Dosage information
- During pregnancy
- Drug class: hereditary angioedema agents
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.