Benztropine (Monograph)
Brand name: Cogentin
Drug class: Anticholinergic Agents
VA class: AU350
CAS number: 132-17-2
Introduction
Antimuscarinic antiparkinsonian agent.
Uses for Benztropine
Parkinsonian Syndrome
Symptomatic management of all forms of parkinsonian syndrome, including idiopathic parkinson disease and parkinsonism resulting from encephalitis (postencephalitic parkinsonism).
Has been used as monotherapy or adjunctive therapy in the treatment of parkinson disease.
Levodopa is currently the most effective drug for relieving motor symptoms of parkinson disease; however, long-term use associated with motor complications. To avoid these complications, may initiate treatment with other antiparkinsonian agents first and postpone use of levodopa. Some clinicians state that anticholinergic agents (e.g., trihexyphenidyl, benztropine) may be particularly useful for initial therapy in patients <60 years of age with resting tremors as their only or most prominent symptom.
Although main use of anticholinergic agents in parkinson disease is to control tremors, evidence of a benefit largely anecdotal.
Drug-induced Extrapyramidal Reactions
Control of extrapyramidal symptoms (EPS) induced by antipsychotic agents (e.g., phenothiazines).
Anticholinergic agents (e.g., benztropine, trihexyphenidyl) are used traditionally to restore acetylcholine and dopamine imbalance in patients with antipsychotic-induced EPS; however, evidence supporting a benefit is lacking or inconsistent and the drugs are associated with a variety of adverse effects.
In general, use cautiously and for minimum duration necessary to control EPS.
Benztropine does not alleviate symptoms of tardive dyskinesia, and in some instances may aggravate them. Use not recommended.
Related/similar drugs
diphenhydramine, Benadryl, ropinirole, pramipexole, amantadine, Sinemet, Cogentin
Benztropine Dosage and Administration
Administration
Administer orally or by IM injection.
Also may be given IV. Because onset of effect is similar with IV and IM route, manufacturer states there usually is no need to administer IV and does not provide specific instructions for IV administration.
Oral Administration
Administer as a single dose at bedtime or in divided doses 2–4 times daily.
IM Administration
Reserve for patients who cannot take oral medication or for emergency situations (e.g., acute dystonia).
Dosage
Available as benztropine mesylate; dosage is expressed in terms of the salt.
Adjust dosage carefully according to individual requirements and response. Initiate with low dosage and increase gradually to minimum effective dosage.
Dosing guidelines are the same for oral and IM administration; oral administration preferred whenever possible.
Pediatric Patients
Manufacturers make no specific dosage recommendations for children ≥3 years of age. (See Pediatric Use under Cautions.)
Adults
Parkinsonian Syndrome
May require periodic dosage adjustments to maintain optimum symptomatic relief in patients receiving concomitant levodopa-carbidopa therapy.
If used to replace or supplement other antiparkinsonian drugs, change should be gradual, with dosage of previous medication reduced as benztropine dosage is increased.
Avoid abrupt discontinuance of concomitantly administered antiparkinsonian drugs.
Idiopathic Parkinsonian Syndrome
OralInitially, 0.5–1 mg as a single daily dose at bedtime. Dosage may be increased by 0.5-mg increments at 5- or 6-day intervals based on response and tolerability up to a maximum of 6 mg daily.
Usual dosage: 1–2 mg daily (range: 0.5–6 mg daily).
IMInitially, 0.5–1 mg as a single dose at bedtime. Dosage may be increased by 0.5-mg increments at 5- or 6-day intervals based on response and tolerability up to a maximum of 6 mg daily.
Usual dosage: 1–2 mg daily (range: 0.5–6 mg daily).
For emergency situations, 1–2 mg normally will provide quick relief; repeat dose if parkinsonian symptoms return.
Postencephalitic Parkinsonian Syndrome
OralInitially, 2 mg daily, given in 1 or more divided doses. In highly sensitive patients, may give a single 0.5 mg-dose at bedtime. Dosage may be increased by 0.5-mg increments at 5- to 6-day intervals up to a maximum of 6 mg daily.
Usual dosage: 1–2 mg daily (range: 0.5–6 mg daily).
IMInitially, 2 mg daily, given in 1 or more divided doses. In highly sensitive patients, may give a single 0.5 mg-dose at bedtime. Dosage may be increased by 0.5-mg increments at 5- or 6-day intervals up to a maximum of 6 mg daily.
Usual dosage: 1–2 mg daily (range: 0.5–6 mg daily).
For emergency situations, 1–2 mg normally will provide quick relief; repeat dose if parkinsonian symptoms return.
Drug-Induced Extrapyramidal Reactions
Oral
1–4 mg once or twice daily.
For EPS that develops shortly after initiation of antipsychotic therapy, 1–2 mg 2 or 3 times daily usually provides relief within 1 or 2 days. Evaluate need for continued therapy after 1–2 weeks.
IM
1–4 mg once or twice daily.
For EPS that develops shortly after initiation of antipsychotic therapy, 1–2 mg 2 or 3 times daily usually provides relief within 1 or 2 days. Evaluate need for continued therapy after 1–2 weeks.
Acute Dystonia
IM followed by Oral1–2 mg, as a single IM dose, followed by 1–2 mg orally twice daily to prevent recurrence.
Prescribing Limits
Adults
Parkinsonian Syndrome
Oral
Maximum 6 mg daily.
IM
Maximum 6 mg daily.
Special Populations
Hepatic Impairment
No specific dosage recommendations at this time.
Renal Impairment
No specific dosage recommendations at this time.
Geriatric Patients
Geriatric patients generally cannot tolerate high dosages of the drug; select dosage with caution, starting at low end of dosing range and increasing only as needed. (See Geriatric Use under Cautions.)
Low Body Weight
Patients with less than average body weight generally cannot tolerate high dosages of the drug.
Cautions for Benztropine
Contraindications
-
Known hypersensitivity to benztropine or any ingredient in the formulation.
-
Children <3 years of age.
Warnings/Precautions
Warnings
Pregnancy
Safe use during pregnancy has not been established.
Cognitive/Physical Impairment
Risk of impaired mental alertness or physical coordination required for performing hazardous tasks (e.g., driving or operating machinery).
Drug Interactions
Concomitant use with phenothiazines or tricyclic antidepressants associated with potentially fatal paralytic ileus, hyperthermia, or heat stoke. Advise patients to promptly notify clinicians if adverse GI effects, fever, or heat intolerance occur if used concomitantly with these drugs or other drugs with anticholinergic or antidopaminergic (e.g., haloperidol) effects. (See Interactions.)
Anhidrosis
Possibly severe anhidrosis and fatal hyperthermia. Use with caution in hot weather, particularly when given concomitantly with other anticholinergic drugs to chronically ill or alcoholic patients, those who have CNS disease, and those engaged in manual labor. Decrease dosages as needed to maintain ability to perspire.
General Precautions
Adequate Patient Monitoring
Has cumulative effects; continue to monitor patients, particularly those with tendency toward tachycardia or with prostatic hypertrophy.
Musculoskeletal Effects
Possible complaints of weakness and inability to move particular muscle groups, particularly at large dosages; adjust dosage as required.
CNS Effects
Possible mental confusion and excitement, particularly with large dosages or in susceptible patients. Visual hallucinations also possible. (See Dosage under Dosage and Administration.)
Risk of intensification of mental symptoms or precipitation of toxic psychosis in patients with mental disorders receiving phenothiazines, especially at beginning of therapy or during dosage adjustment; monitor closely. (See Specific Drugs under Interactions.)
Tardive Dyskinesia
Not recommended for use in patients with tardive dyskinesia. (See Drug-induced Extrapyramidal Reactions under Uses.)
Renal Effects
Possible dysuria or urinary retention.
Glaucoma
Consider risks of glaucoma. Probably should not be used in patients with angle-closure glaucoma.
Specific Populations
Pregnancy
Safe use during pregnancy not established.
Geriatric Use
Possibility exists of greater sensitivity to the drug in some geriatric individuals. Careful dosage selection necessary. Some experts state to avoid use in geriatric patients because of unfavorable balance of benefits and risks compared with alternative treatments.
Pediatric Use
Safety and efficacy not established in children <3 years of age. (See Cautions: Contraindications.)
Use with caution in children >3 years of age because of adverse anticholinergic effects.
Common Adverse Effects
Dry mouth, blurred vision, mydriasis, nausea, nervousness, tachycardia, paralytic ileus, constipation.
Drug Interactions
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Anticholinergic agents |
Increased risk of adverse anticholinergic effects |
|
|
Antidepressants, tricyclics |
Potentially fatal paralytic ileus, hyperthermia, or heat intolerance |
Advise patients to promptly notify clinicians if adverse GI effects, fever, or heat intolerance occurs |
|
Haloperidol |
Potentially fatal paralytic ileus, hyperthermia, or heat intolerance |
Advise patients to promptly notify clinicians if adverse GI effects, fever, or heat intolerance occurs |
|
Phenothiazines |
Potentially fatal paralytic ileus, hyperthermia, or heat intolerance Possible intensification of mental symptoms or precipitation of toxic psychosis in patients with mental disorders |
Advise patients to promptly notify clinicians if adverse GI effects, fever, or heat intolerance occurs Observe carefully, especially at beginning of therapy or during dosage adjustment |
Stability
Storage
Oral
Tablets
20–25°C.
Parenteral
Injection
20–25°C.
Compatibility
Drug Compatibility
For information on IV injection of benztropine, see Administration under Dosage and Administration.
|
Compatible |
|---|
|
Cloxacillin sodium |
|
Fluconazole |
|
Tacrolimus |
|
Compatible |
|---|
|
Chlorpromazine HCl |
|
Fluphenazine HCl |
|
Metoclopramide HCl |
|
Variable |
|
Haloperidol lactate |
Actions
-
Possesses both anticholinergic and antihistaminic effects, although only the former have been established as therapeutically important in management of parkinsonism.
Advice to Patients
-
Potential for drug to impair mental alertness or physical coordination; use caution when driving or operating machinery until effects on individual are known.
-
Risk of hyperthermia.
-
Importance of promptly notifying clinicians of adverse GI effects, fever, or heat intolerance, particularly if also receiving phenothiazines, haloperidol, or other drugs with anticholinergic or antidopaminergic activity.
-
Importance of women informing their clinician if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as concomitant illnesses.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
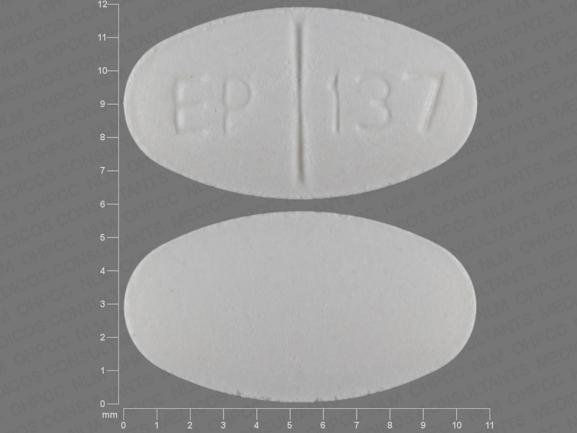
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
0.5 mg* |
Benztropine Mesylate Tablets |
|
|
1 mg* |
Benztropine Mesylate Tablets |
|||
|
2 mg* |
Benztropine Mesylate Tablets |
|||
|
Parenteral |
Injection |
1 mg/mL* |
Benztropine Mesylate Injection |
|
|
Cogentin |
Akorn |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions February 17, 2022. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
More about benztropine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (36)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Drug class: anticholinergic antiparkinson agents
- Breastfeeding
- En español