Atezolizumab (Monograph)
Brand name: Tecentriq
Drug class: Antineoplastic Agents
- Programmed Death Ligand-1 Antagonist
- PD-L1 Inhibitor
Chemical name: Immunoglobulin G1-κ, anti-[Homo sapiens CD274 (programmed death ligand 1, PDL1, PD-L1, B7 homolog 1, B7H1)], humanized monoclonal antibody
Molecular formula: C6446H9902N1706O1998S42
CAS number: 1380723-44-3
Introduction
Antineoplastic agent; humanized anti-programmed-death ligand-1 (anti-PD-L1) monoclonal antibody.
Uses for Atezolizumab
Urothelial Carcinoma
Used as a single agent for the treatment of locally advanced or metastatic urothelial carcinoma in adult patients with high PD-L1 expression (defined as PD-L1 staining in tumor-infiltrating immune cells covering ≥5% of tumor area) who are not candidates for cisplatin-containing therapy. FDA-approved diagnostic test required to confirm presence of PD-L1 expression prior to initiation of therapy.
Used as a single agent for the treatment of locally advanced or metastatic urothelial carcinoma in adult patients who are not candidates for platinum-containing chemotherapy regardless of PD-L1 expression.
Accelerated approval for these indications based on objective response rate and duration of response. Continued approval may be contingent on verification and description of clinical benefit in confirmatory studies.
Decreased survival reported with atezolizumab monotherapy compared with platinum-based therapy in patients with previously untreated metastatic urothelial carcinoma with low PD-L1 expression; atezolizumab is not indicated in such patients.
Non-small Cell Lung Cancer (NSCLC)
Used as a single agent for the initial treatment of metastatic non-small cell lung cancer (NSCLC) in adult patients with high PD-L1 expression and without epidermal growth factor receptor (EGFR) or anaplastic lymphoma kinase (ALK) genomic aberrations. High PD-L1 expression defined as PD-L1 staining of ≥50% of tumor cells or PD-L1 stained tumor-infiltrating immune cells covering ≥10% of the tumor area using an FDA-approved diagnostic test.
Used in combination with bevacizumab, carboplatin, and paclitaxel for the initial treatment of metastatic nonsquamous NSCLC without EGFR or ALK genomic aberrations.
Used in combination with albumin-bound paclitaxel and carboplatin for the initial treatment of metastatic nonsquamous NSCLC without EGFR or ALK genomic aberrations.
Used as a single agent for the treatment of metastatic NSCLC that has progressed during or following platinum-based chemotherapy. Patients with EGFR- or ALK-positive tumors also should have documented disease progression during or following an FDA-labeled anti-EGFR or anti-ALK therapy prior to initiating therapy with atezolizumab.
Breast Cancer
Used in combination with albumin-bound paclitaxel for the treatment of unresectable locally advanced or metastatic triple-negative breast cancer in adult patients with PD-L1 expression (defined as PD-L1 staining in tumor-infiltrating immune cells of any intensity covering ≥1% of the tumor area). FDA-approved diagnostic test required to confirm presence of PD-L1 expression prior to initiation of therapy.
Accelerated approval for this indication based on progression-free survival. Continued approval may be contingent on verification and description of clinical benefit in confirmatory studies.
Do not use atezolizumab in combination with conventional paclitaxel for the treatment of triple-negative breast cancer.
Small Cell Lung Cancer (SCLC)
Used in combination with carboplatin and etoposide for the initial treatment of extensive-stage SCLC (designated an orphan drug by FDA for treatment of this cancer).
Hepatocellular Carcinoma (HCC)
Used in combination with bevacizumab for the treatment of patients with unresectable or metastatic HCC (designated an orphan drug by FDA for treatment of this cancer).
Melanoma
Used in combination with cobimetinib and vemurafenib for the treatment of unresectable or metastatic melanoma harboring BRAF V600 mutation (designated an orphan drug by FDA for treatment of this cancer).
Atezolizumab Dosage and Administration
General
Pretreatment Screening
-
Verify pregnancy status in females of reproductive potential.
-
Liver function tests.
-
Thyroid function.
- Biomarker Testing
-
Select patients for treatment with atezolizumab based on the presence of biomarkers. (See Table 1.)
|
Indication |
Biomarker |
|---|---|
|
Locally advanced or metastatic urothelial carcinoma in patients who are not candidates for cisplatin-containing chemotherapy |
PD-L1 expression on tumor-infiltrating immune cells (see Urothelial Carcinoma under Uses) |
|
Monotherapy for the treatment of metastatic NSCLC |
PD-L1 expression on tumor cells or tumor-infiltrating immune cells (see Non-small Cell Lung Cancer [NSCLC] under Uses) |
|
Locally advanced or metastatic triple-negative breast cancer (in combination with albumin-bound paclitaxel) |
PD-L1 expression on tumor-infiltrating immune cells (see Breast Cancer under Uses) |
|
Unresectable or metastatic melanoma (in combination with cobimetinib and vemurafenib) |
BRAF V600 mutation (see Melanoma under Uses) |
Patient Monitoring
-
Immune-mediated effects during and following therapy.
-
Manifestations of pneumonitis.
-
Signs and symptoms of hepatitis (e.g., liver function tests) during therapy.
-
Signs and symptoms of colitis (e.g., diarrhea, abdominal pain, lower GI bleeding).
-
Thyroid function periodically during therapy. Monitor for thyroiditis.
-
Signs and symptoms of adrenal insufficiency.
-
Signs and symptoms of diabetes mellitus (e.g., hyperglycemia).
-
Signs and symptoms of hypophysitis (e.g., headache, photophobia, visual field changes, hypopituitarism).
-
Signs and symptoms of dermatologic effects.
-
Signs and symptoms of infusion-related reactions.
Other General Considerations
-
Consider potential benefits and risks of anti-PD-1 monoclonal antibody therapy administered either before or after allogeneic stem cell transplantation. Closely monitor for early manifestations of stem cell transplantation-related complications and manage promptly if they occur.
Administration
IV Administration
For solution compatibility information, see Compatibility under Stability.
Administer by IV infusion. Do not administer by rapid IV injection (e.g., IV push or bolus).
Atezolizumab injection concentrate must be diluted prior to administration. Immediate administration recommended. (See Storage under Stability.)
Do not infuse simultaneously through the same IV line with other drugs.
Use of low-protein-binding 0.2- to 0.22-µm inline filter is optional.
Dilution
Undiluted solution should be colorless to slightly yellow. Do not use if it is cloudy or discolored or if particulate matter is present.
Do not shake vial.
Select appropriate vial size based on dosage required. Withdraw the required volume of atezolizumab injection concentrate (containing 60 mg/mL) and dilute in a PVC, polyethylene, or polyolefin infusion bag containing 0.9% sodium chloride to a final concentration of 3.2–16.8 mg/mL. Do not use any other diluent. Mix the diluted solution by gentle inversion; do not shake. Discard any partially used vial.
Rate of Administration
Initial dose: Administer over 60 minutes.
Subsequent doses: Administer over 30 minutes (if first infusion well tolerated).
Dosage
Adults
Urothelial Carcinoma
IV
840 mg every 2 weeks, 1200 mg every 3 weeks, or 1680 mg every 4 weeks. Continue therapy until disease progression or unacceptable toxicity occurs.
Selection based on presence of PD-L1 expression unless ineligible for any platinum-containing chemotherapy. (See General under Dosage and Administration.)
NSCLC
Monotherapy for Previously Untreated Metastatic NSCLC
IV840 mg every 2 weeks, 1200 mg every 3 weeks, or 1680 mg every 4 weeks. Continue therapy until disease progression or unacceptable toxicity occurs.
Selection based on presence of high PD-L1 expression. (See General under Dosage and Administration.)
Combination Therapy for Previously Untreated Metastatic Nonsquamous NSCLC
IV840 mg every 2 weeks, 1200 mg every 3 weeks, or 1680 mg every 4 weeks (use in combination with bevacizumab, carboplatin, and paclitaxel, or in combination with albumin-bound paclitaxel and carboplatin).
In the IMpower150 study, carboplatin and paclitaxel were administered for a maximum of 4–6 cycles. Continue atezolizumab and bevacizumab until disease progression or unacceptable toxicity occurs.
In the IMpower130 study, albumin-bound paclitaxel and carboplatin were administered for a maximum of 4–6 cycles. Continue atezolizumab until disease progression or unacceptable toxicity occurs.
Administer atezolizumab prior to chemotherapy, including bevacizumab, when scheduled on the same day.
Monotherapy for Previously Treated Metastatic NSCLC
IV840 mg every 2 weeks, 1200 mg every 3 weeks, or 1680 mg every 4 weeks. Continue therapy until disease progression or unacceptable toxicity occurs.
Breast Cancer
Locally Advanced or Metastatic Triple-negative Breast Cancer
IV840 mg every 2 weeks, 1200 mg every 3 weeks, or 1680 mg every 4 weeks (use in combination with albumin-bound paclitaxel). Continue therapy until disease progression or unacceptable toxicity occurs.
Selection based on presence of PD-L1 expression. (See General under Dosage and Administration.)
Administer atezolizumab prior to albumin-bound paclitaxel when scheduled on the same day.
May discontinue atezolizumab and albumin-bound paclitaxel independently of each other if toxicity occurs.
Do not use in combination with conventional paclitaxel for the treatment of triple-negative breast cancer. (See Treatment-related Mortality under Cautions.)
SCLC
IV
840 mg every 2 weeks, 1200 mg every 3 weeks, or 1680 mg every 4 weeks (use in combination with carboplatin and etoposide).
In the principal efficacy study, carboplatin and etoposide were administered for a maximum of 4 cycles. Continue atezolizumab until disease progression or unacceptable toxicity occurs.
Administer atezolizumab prior to carboplatin and etoposide when scheduled on the same day.
HCC
IV
840 mg every 2 weeks, 1200 mg every 3 weeks, or 1680 mg every 4 weeks (use in combination with bevacizumab). Continue therapy until disease progression or unacceptable toxicity occurs.
Administer atezolizumab prior to bevacizumab when scheduled on the same day.
Melanoma
IV
840 mg every 2 weeks, 1200 mg every 3 weeks, or 1680 mg every 4 weeks (use in combination with cobimetinib and vemurafenib). Continue therapy until disease progression or unacceptable toxicity occurs.
Selection based on presence of BRAF V600 mutation. (See General under Dosage and Administration.)
Initiate after completing the one 28-day cycle of cobimetinib 60 mg orally once daily on days 1–21 and vemurafenib 960 mg orally twice daily on days 1–21, followed by vemurafenib 720 mg orally twice daily on days 22–28; for subsequent cycles, administer atezolizumab in combination with cobimetinib 60 mg orally once daily on days 1–21 and vemurafenib 720 mg orally twice daily on days 1–28 of a 28-day cycle.
Therapy Interruption for Toxicity
Temporarily interrupt or permanently discontinue atezolizumab based on toxicity and severity of the reaction. Do not reduce dosage.
In general, temporarily interrupt atezolizumab therapy if severe (grade 3) immune-mediated adverse effects occur.
Permanently discontinue atezolizumab therapy in patients experiencing grade 4 immune-mediated adverse effects, recurrent grade 3 immune-mediated adverse effects requiring systemic immunosuppressive therapy, and in patients unable to reduce corticosteroid dosage to ≤10 mg of prednisone daily (or equivalent) within 12 weeks of initiating corticosteroids.
Immune-mediated Pulmonary Effects
IVIf grade 2 immune-mediated pneumonitis occurs, interrupt therapy until toxicity resolves to grade 0 or 1 and corticosteroid taper is complete. Permanently discontinue if toxicity does not resolve to grade 0 or 1 within 12 weeks of starting corticosteroids or if corticosteroid dosage cannot be reduced to ≤10 mg of prednisone daily (or equivalent) within 12 weeks of initiating corticosteroids. (See Immune-mediated Pulmonary Effects under Cautions.)
If grade 3 or 4 immune-mediated pneumonitis occurs, discontinue drug.
Immune-mediated Hepatic Effects
IVFor serum AST or ALT elevations >3 times but ≤8 times the ULN, or total bilirubin concentrations >1.5 times but ≤3 times the ULN in patients without tumor involvement of the liver, interrupt therapy until toxicity resolves to grade 0 or 1 and the corticosteroid taper is complete. Permanently discontinue drug if immune-mediated hepatitis does not resolve within 12 weeks of corticosteroid therapy or if corticosteroid dosage cannot be reduced to ≤10 mg of prednisone daily (or equivalent) within 12 weeks of initiating corticosteroids.
For serum AST or ALT elevations >8 times the ULN or total bilirubin concentrations >3 times the ULN in patients without tumor involvement of the liver, permanently discontinue drug.
For serum AST or ALT elevations >5 times but ≤10 times the ULN in patients with liver involvement and baseline AST or ALT >1 time but ≤3 times the ULN, interrupt therapy until toxicity resolves to grade 0 or 1 and the corticosteroid taper is complete. Permanently discontinue drug if immune-mediated hepatitis does not resolve within 12 weeks of corticosteroid therapy or if corticosteroid dosage cannot be reduced to ≤10 mg of prednisone daily (or equivalent) within 12 weeks of initiating corticosteroids.
For serum AST or ALT elevations >8 times but ≤10 times the ULN in patients with liver involvement and baseline ALT or AST concentrations >3 times the ULN but ≤5 times the ULN, interrupt therapy until toxicity resolves to grade 0 or 1 and the corticosteroid taper is complete. Permanently discontinue drug if immune-mediated hepatitis does not resolve within 12 weeks of corticosteroid therapy or if corticosteroid dosage cannot be reduced to ≤10 mg of prednisone daily (or equivalent) within 12 weeks of initiating corticosteroids.
For serum AST or ALT elevations >10 times the ULN or total bilirubin concentration elevation >3 times the ULN in patients with liver involvement and any baseline AST or ALT, permanently discontinue drug.
For serum AST or ALT elevations >3 times but ≤8 times the ULN, or total bilirubin concentrations >1.5 times but ≤3 times the ULN in patients with tumor involvement of the liver and baseline AST and ALT less than or equal to the ULN, interrupt therapy until toxicity resolves to grade 0 or 1 and the corticosteroid taper is complete. Permanently discontinue drug if immune-mediated hepatitis resolution does not resolve within 12 weeks of corticosteroid therapy or if corticosteroid dosage cannot be reduced to ≤10 mg of prednisone daily (or equivalent) within 12 weeks of initiating corticosteroids.
For serum AST or ALT elevations >8 times the ULN or total bilirubin concentrations >3 times the ULN in patients with tumor involvement of the liver and baseline AST and ALT less than or equal to the ULN, permanently discontinue drug.
Immune-mediated GI Effects
IVIf grade 2 or 3 immune-mediated colitis occurs, interrupt therapy until toxicity resolves to grade 0 or 1 and corticosteroid taper is complete. Permanently discontinue drug if toxicity does not resolve to grade 0 or 1 within 12 weeks of starting corticosteroids or if corticosteroid dosage cannot be reduced to ≤10 mg of prednisone daily (or equivalent) within 12 weeks of initiating corticosteroids. (See Immune-mediated GI Effects under Cautions.)
If grade 4 immune-mediated colitis occurs, discontinue drug.
Immune-mediated Endocrine Effects
IVIf grade 3 or 4 immune-mediated endocrinopathies (e.g., hypophysitis, adrenal insufficiency, thyroid disorders, type 1 diabetes mellitus) occur, either interrupt therapy until patient is clinically stable or permanently discontinue drug, depending on severity. (See Immune-mediated Endocrine Effects under Cautions.)
Immune-mediated Renal Effects.
IVIf immune-mediated nephritis characterized by grade 2 or 3 Scr elevations occurs, interrupt therapy until toxicity resolves to grade 0 or 1 and corticosteroid taper is complete. Permanently discontinue if toxicity does not resolve to grade 0 or 1 within 12 weeks of starting corticosteroids or if corticosteroid dosage cannot be reduced to ≤10 mg of prednisone daily (or equivalent) within 12 weeks. (See Immune-mediated Renal Effects under Cautions.)
If immune-mediated nephritis characterized by grade 4 Scr elevations occurs, permanently discontinue drug.
Immune-mediated Dermatologic Effects.
IVIf exfoliative dermatitis (i.e., Stevens-Johnson syndrome [SJS], toxic epidermal necrolysis [TEN], drug rash with eosinophilia and systemic symptoms [DRESS]) is suspected, temporarily interrupt therapy with atezolizumab.
If diagnosis is confirmed, permanently discontinue drug. (See Immune-mediated Dermatologic Effects under Cautions.)
Immune-mediated Cardiac Effects.
IVIf grade 2–4 immune-mediated myocarditis occurs, permanently discontinue drug.
Immune-mediated Neurologic Effects
IVIf grade 2 immune-mediated neurologic toxicity (e.g., meningitis, encephalitis, myasthenia gravis, Guillain-Barré syndrome, autoimmune neuropathy) occurs, interrupt therapy until toxicity resolves to grade 0 or 1 and corticosteroid taper is complete. Permanently discontinue if toxicity does not resolve to grade 0 or 1 within 12 weeks of starting corticosteroids or if corticosteroid dosage cannot be reduced to ≤10 mg of prednisone daily (or equivalent) within 12 weeks of initiating corticosteroids. (See Other Immune-mediated Effects under Cautions.)
If grade 3 or 4 immune-mediated neurologic toxicity occurs, permanently discontinue drug.
Infusion-related Reactions
IVIf grade 1 or 2 infusion-related reactions occur, interrupt infusion or reduce infusion rate. (See Infusion-related Effects under Cautions.)
If grade 3 or 4 infusion-related reactions occur, permanently discontinue drug.
Special Populations
Hepatic Impairment
No special dosage recommendations at this time.
Renal Impairment
No special dosage recommendations at this time.
Geriatric Patients
No special dosage recommendations at this time.
Cautions for Atezolizumab
Contraindications
-
No known contraindications.
Warnings/Precautions
Severe and Fatal Immune-mediated Effects
Severe or fatal immune-mediated adverse effects in any tissue or organ system may occur; generally occurs during treatment, but also may appear after therapy is discontinued.
Monitor closely for immune-mediated effects during and following therapy. If an immune-mediated adverse effect is suspected, assess for potential alternative causes, and promptly initiate treatment; consider consultation with a specialist, if appropriate.
Interrupt or discontinue atezolizumab therapy depending on type and severity of toxicity. (See Therapy Interruption for Toxicity under Dosage and Administration.)
If interruption or discontinuance of atezolizumab is necessary, initiate systemic corticosteroid therapy (prednisone 1–2 mg/kg per day [or equivalent]), unless systemic corticosteroids are not required for the specific toxicity (e.g., mild or moderate non-exfoliative dermatologic rash, certain immune-mediated endocrine effects). Continue systemic corticosteroids until resolution to grade 1 or less, then taper over ≥1 month. If immune-mediated effects are not controlled with corticosteroids, consider other systemic immunosuppressants.
Immune-mediated Pulmonary Effects
Immune-mediated pneumonitis or interstitial lung disease, sometimes fatal, reported. Prior thoracic radiation may increase risk.
Monitor patients for manifestations of pneumonitis.
If immune-mediated pneumonitis occurs, temporarily withhold or discontinue atezolizumab. (See Immune-mediated Pulmonary Effects under Dosage and Administration and also see Severe and Fatal Immune-mediated Effects under Dosage and Administration.)
Immune-mediated Hepatic Effects
Immune-mediated hepatitis, sometimes fatal, reported.
Monitor patients for signs and symptoms of hepatitis (e.g., perform liver chemistry tests) at baseline and during therapy.
If immune-mediated hepatitis or liver function test abnormalities occur, temporarily withhold or discontinue atezolizumab. (See Immune-mediated Hepatic Effects under Dosage and Administration and also see Severe and Fatal Immune-mediated Effects under Cautions.)
Immune-mediated GI Effects
Immune-mediated colitis reported.
Monitor patients for signs and symptoms of colitis (e.g., diarrhea, abdominal pain, lower GI bleeding).
Depending on severity of immune-mediated colitis, temporarily withhold or discontinue atezolizumab. (See Immune-mediated GI Effects under Dosage and Administration and also see Severe and Fatal Immune-mediated Effects under Cautions.)
Cytomegalovirus (CMV) infection or reactivation reported in corticosteroid-refractory immune-mediated colitis; consider assessing for alternative etiologies in patients with corticosteroid-refractory colitis.
Immune-mediated Endocrine Effects
Immune-mediated endocrinopathies, such as thyroid dysfunction (i.e., thyroiditis, hypothyroidism, hyperthyroidism), adrenal insufficiency (primary or secondary), hypophysitis/hypopituitarism, and diabetes mellitus (including ketoacidosis), reported.
Thyroid Dysfunction
Evaluate thyroid function prior to initiation of and periodically during therapy; monitor for thyroiditis. Immune-mediated hyperthyroidism may be followed by hypothyroidism.
If immune-mediated hypothyroidism occurs, initiate thyroid hormone replacement therapy as clinically indicated. If immune-mediated hyperthyroidism occurs, initiate antithyroid therapy as clinically indicated.
Depending on severity of immune-mediated thyroid dysfunction, temporary interruption or permanent discontinuance of atezolizumab may be necessary. (See Immune-mediated Endocrine Effects under Dosage and Administration and also see Severe and Fatal Immune-mediated Effects under Cautions.)
Adrenal Insufficiency
Monitor for signs and symptoms of adrenal insufficiency.
Depending on severity of immune-mediated adrenal insufficiency, temporarily withhold or discontinue atezolizumab. (See Immune-mediated Endocrine Effects under Dosage and Administration and also see Severe and Fatal Immune-mediated Effects under Cautions.) If grade 2 or greater immune-mediated adrenal insufficiency occurs, initiate symptomatic treatment (e.g., hormone replacement therapy, as clinically indicated.
Hypophysitis
Monitor for signs and symptoms of hypophysitis (e.g., headache, photophobia, visual field changes, hypopituitarism).
Depending on severity of immune-mediated hypophysitis, temporarily withhold or discontinue atezolizumab. Initiate hormone replacement therapy as clinically indicated. (See Immune-mediated Endocrine Effects under Dosage and Administration and also see Severe and Fatal Immune-mediated Effects under Cautions.)
Diabetes Mellitus
Monitor for signs and symptoms of diabetes mellitus (e.g., hyperglycemia).
Depending on severity of immune-mediated type 1 diabetes mellitus, temporary interruption or discontinuance of atezolizumab may be necessary. (See Immune-mediated Endocrine Effects under Dosage and Administration and also see Severe and Fatal Immune-mediated Effects under Cautions.) If immune-mediated type 1 diabetes mellitus occurs, initiate insulin therapy as clinically indicated.
Immune-mediated Renal Effects
Immune-mediated nephritis with renal dysfunction reported.
Monitor patients for signs and symptoms of nephritis or renal dysfunction (e.g., Scr concentration) at baseline and periodically during therapy.
Depending on severity of immune-mediated nephritis or renal dysfunction, temporarily withhold or discontinue atezolizumab. (See Immune-mediated Renal Effects under Dosage and Administration and also see Severe and Fatal Immune-mediated Effects under Cautions.)
Immune-mediated Dermatologic Effects
Immune-mediated rash and dermatitis reported; may include SJS, TEN, or DRESS.
Monitor for signs and symptoms of dermatologic effects.
Mild or moderate non-exfoliative rashes may be adequately treated with topical corticosteroids and/or emollients. Temporary interruption or discontinuance of atezolizumab may be necessary for more severe dermatologic conditions. (See Immune-mediated Dermatologic Effects under Dosage and Administration and also see Severe and Fatal Immune-mediated Effects under Cautions.)
Other Immune-mediated Effects
Immune-mediated adverse effects (e.g., myocarditis, pericarditis, vasculitis, meningitis, encephalitis, myelitis and demyelination, myasthenic syndrome/myasthenia gravis, Guillain-Barré syndrome, nerve paresis, autoimmune neuropathy, uveitis, iritis, other ocular inflammatory toxicity, retinal detachment, visual impairment, blindness, pancreatitis [including elevation of serum amylase and lipase concentrations], gastritis, duodenitis, myositis/polymyositis, rhabdomyolysis [including renal failure], arthritis, polymyalgia rheumatic, hypoparathyroidism, hemolytic anemia, aplastic anemia, hemophagocytic lymphohistiocytosis, systemic inflammatory response syndrome, histiocytic necrotizing lymphadenitis [Kikuchi lymphadenitis], sarcoidosis, immune thrombocytopenic purpura, solid organ transplant rejection), sometimes fatal, reported with atezolizumab or other anti-PD-1 or anti-PD-L1 antibodies.
Depending on severity of immune-mediated adverse effect, temporarily withhold or discontinue atezolizumab. (See Severe and Fatal Immune-mediated Effects under Cautions.)
If uveitis occurs in conjunction with other immune-mediated adverse effects, consider possibility of Vogt-Koyanagi-Harada-like syndrome. Systemic corticosteroid therapy may be required to reduce risk of permanent vision loss.
Allogeneic Stem Cell Transplantation-related Complications
Complications (i.e., hyperacute, acute, or chronic graft-versus-host disease [GVHD]; febrile syndrome requiring systemic corticosteroid therapy; hepatic veno-occlusive disease following allogeneic stem cell transplantation with a reduced-intensity conditioning regimen), sometimes fatal, may occur in patients undergoing allogeneic stem cell transplantation before or after therapy with anti-PD-1 monoclonal antibodies, including atezolizumab. Complications may occur despite other intervening therapy between atezolizumab administration and transplantation.
Consider potential benefits and risks of anti-PD-1 monoclonal antibody therapy administered either before or after allogeneic stem cell transplantation. Closely monitor for early manifestations of stem cell transplantation-related complications and manage promptly if they occur.
Treatment-related Mortality
Increased mortality reported in PD-L1-positive patients with metastatic triple-negative breast cancer receiving atezolizumab in combination with conventional paclitaxel; atezolizumab is not currently FDA-labeled for use in combination with conventional paclitaxel in patients with triple-negative unresectable locally advanced or metastatic breast cancer.
Do not substitute conventional paclitaxel for albumin-bound paclitaxel in patients with metastatic triple-negative breast cancer outside of a controlled clinical trial.
Infusion-related Effects
Severe or life-threatening infusion-related reactions reported.
Monitor patients for signs and symptoms of infusion-related reactions.
If infusion-related reactions occur, interrupt infusion, reduce infusion rate, or discontinue atezolizumab. (See Infusion-related Reactions under Dosage and Administration.)
If grade 1 or 2 infusion-related reactions occur, consider premedication prior to subsequent infusions.
Fetal/Neonatal Morbidity and Mortality
May cause fetal harm. May disrupt maternal immune tolerance to the fetus and increase risk of fetal loss (abortion, stillbirth); also may increase risk of immune-mediated disorders.
Avoid pregnancy during therapy. Verify pregnancy status prior to initiation of therapy. Females of reproductive potential should use an effective contraceptive method while receiving atezolizumab and for ≥5 months after the drug is discontinued. Apprise females of reproductive potential of potential fetal hazard if used during pregnancy.
Immunogenicity
Potential for immunogenicity. Development of anti-atezolizumab antibodies reported; neutralizing capacity of the antibodies not established.
Effects on safety of atezolizumab not observed; however, clearance of atezolizumab increased by 22% and systemic exposure of the drug decreased in the presence of anti-atezolizumab antibodies. Exploratory analysis suggests reduced efficacy (overall survival) of single-agent atezolizumab in patients with locally advanced or metastatic NSCLC who develop anti-atezolizumab antibodies by week 4 and reduced efficacy of atezolizumab in combination with bevacizumab in patients with previously untreated HCC who develop anti-atezolizumab antibodies by week 6. Exploratory analysis in patients with nonsquamous NSCLC receiving atezolizumab in combination with bevacizumab, carboplatin, and paclitaxel suggests similar efficacy in those with or without development of anti-atezolizumab antibodies by week 4.
Impairment of Fertility
May impair female fertility.
Specific Populations
Pregnancy
May cause fetal harm. (See Fetal/Neonatal Morbidity and Mortality under Cautions.)
Verify pregnancy status prior to initiating atezolizumab therapy.
Lactation
Not known whether atezolizumab is distributed into milk. Discontinue nursing during therapy and for ≥5 months after drug discontinuance.
Pediatric Use
Safety and efficacy not established.
Geriatric Use
In studies of single-agent atezolizumab for the treatment of metastatic urothelial carcinoma, metastatic NSCLC, or other tumor types, 49% of patients were ≥65 years of age and 15% were ≥75 years of age. In clinical studies of atezolizumab in combination with other antineoplastic agents for the treatment of SCLC and NSCLC, 48% of patients were ≥65 years of age and 10% were ≥75 years of age. No overall differences in safety or efficacy relative to younger adults.
Hepatic Impairment
Systemic exposure and clearance not affected by mild or moderate hepatic impairment. Data lacking in patients with severe hepatic impairment. (See Special Populations under Pharmacokinetics.)
Renal Impairment
Clearance not affected by mild or moderate renal impairment. Limited data available in patients with severe renal impairment. (See Special Populations under Pharmacokinetics.)
Common Adverse Effects
Single-agent atezolizumab (≥20%): Fatigue or asthenia, nausea, cough, dyspnea, decreased appetite.
In combination with other antineoplastic agents in patients with NSCLC or SCLC (≥20%): Fatigue or asthenia, nausea, alopecia, constipation, diarrhea, decreased appetite.
In combination with albumin-bound paclitaxel in patients with triple-negative breast cancer (≥20%): Alopecia, peripheral neuropathy, fatigue, nausea, diarrhea, constipation, cough, headache, vomiting, decreased appetite; laboratory abnormalities occurring in ≥50% of patients include decreased concentrations of hemoglobin, leukocytes, neutrophils, and lymphocytes.
In combination with bevacizumab in patients with HCC (≥20%): Hypertension, fatigue, proteinuria.
In combination with cobimetinib and vemurafenib in patients with melanoma (≥20%): Rash, musculoskeletal pain, fatigue, hepatotoxicity, pyrexia, nausea, pruritus, edema, stomatitis, hypothyroidism, photosensitivity.
Drug Interactions
No formal drug interaction studies to date.
Atezolizumab Pharmacokinetics
Absorption
Bioavailability
Steady-state concentrations achieved within 6–9 weeks.
Systemic exposure is dose proportional over the dose range of 1–20 mg/kg, including fixed dosage of 1.2 g every 3 weeks; systemic accumulation is 3.3-fold when administered every 2 weeks and 1.9-fold when administered every 3 weeks.
Distribution
Extent
Not known whether atezolizumab is distributed into milk.
Elimination
Half-life
27 days.
Clearance decreases over time by approximately 17% from baseline values; difference not clinically important.
Special Populations
Mild (total bilirubin concentration not exceeding the ULN with AST concentration exceeding the ULN, or total bilirubin concentration between 1–1.5 times the ULN with any AST concentration) or moderate (total bilirubin concentration >1.5 times but ≤3 times the ULN with any AST concentration) hepatic impairment does not affect clearance and systemic exposure. Effect of severe hepatic impairment on atezolizumab pharmacokinetics not established.
Mild or moderate renal impairment (estimated GFR 30–89 mL/minute per 1.73 m2) does not affect clearance. Limited data available for severe renal impairment.
Age (range of 21–89 years), body weight, sex, serum albumin concentration, tumor burden, geographic region, race, PD-L1 expression, and performance status do not have meaningful effects on systemic exposure of atezolizumab.
Stability
Storage
Parenteral
Injection
2–8°C. Do not freeze; protect from light.
Diluted solution: Room temperature for ≤6 hours from time of preparation (including infusion time) or 2–8°C for ≤24 hours from time of preparation. Do not freeze.
Compatibility
Parenteral
Solution Compatibility1
|
Compatible |
|---|
|
Sodium chloride 0.9% |
Actions
-
An IgG1 kappa immunoglobulin that is selective for PD-L1.
-
Overexpression of PD-1 ligands on surface of tumor cells results in activation of PD-1 and B7.1 and suppression of cytotoxic T-cell activity, T-cell proliferation, and cytokine production.
-
Blocks interaction between PD-L1 and the receptors PD-1 and B7.1, resulting in activation of antitumor immune response without inducing antibody-dependent cell-mediated cytotoxicity (ADCC).
Advice to Patients
Importance of advising patients to read the manufacturer's medication guide.
Risk of immune-mediated pneumonitis. Importance of informing clinician immediately if new or worsening cough, chest pain, or shortness of breath occurs.
Risk of immune-mediated colitis. Importance of informing clinician immediately if diarrhea or severe abdominal pain occurs or if mucus or blood is present in stool.
Risk of immune-mediated hepatitis. Importance of informing clinician immediately if signs and symptoms of liver damage (e.g., jaundice, severe nausea or vomiting, abdominal pain [particularly in the right upper quadrant], lethargy, easy bruising or bleeding, lack of appetite, dark urine, drowsiness) occur.
Risk of immune-mediated endocrine effects. Importance of informing clinician immediately if manifestations of hypophysitis, hyperthyroidism, hypothyroidism, adrenal insufficiency, or diabetes mellitus (including ketoacidosis) occur.
Risk of immune-mediated nephritis. Importance of informing clinician immediately if signs or symptoms of nephritis (e.g., pelvic pain, frequent urination, unusual swelling) occur.
Risk of immune-mediated dermatologic adverse effects. Importance of informing clinician immediately if skin eruption, generalized rash, or painful lesions on the skin or mucous membranes develop.
Risk of other immune-mediated adverse effects. Importance of informing clinician immediately if manifestations of other potential immune-mediated adverse effects occur.
Risk of infusion-related reactions. Importance of informing clinician if signs and symptoms of such reactions, including dizziness, chills, fever, breathing difficulty (i.e., shortness of breath, wheezing), pruritus, flushing, feeling of faintness, back or neck pain, and angioedema, occur.
Risk of allogeneic stem cell transplantation-related complications.
Risk of fetal harm. Necessity of advising women of childbearing potential that they should use an effective method of contraception while receiving atezolizumab and for at least 5 months after discontinuance of therapy. Importance of women informing clinicians if they are or plan to become pregnant. If pregnancy occurs, advise pregnant women of potential risk to the fetus.
Importance of advising women to avoid breast-feeding while receiving atezolizumab and for at least 5 months after discontinuance of therapy.
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements, as well as any concomitant illnesses.
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
Obtain atezolizumab through a limited network of specialty distributors. Contact manufacturer for additional information.
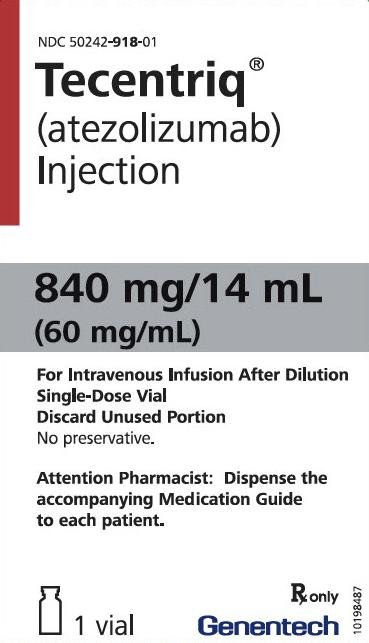
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Concentrate, for injection, for IV infusion |
60 mg/mL (840 mg and 1200 mg) |
Tecentriq |
Genentech |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions October 18, 2021. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Biological Products Related to atezolizumab
Find detailed information on biosimilars for this medication.
Frequently asked questions
- Are there cost-saving programs for Tecentriq?
- How effective is it?
- Is atezolizumab (Tecentriq) a chemotherapy or immunotherapy drug?
- Does atezolizumab (Tecentriq) cause hair loss?
- How is atezolizumab (Tecentriq) administered?
- What type of cancer is Tecentriq used to treat?
More about atezolizumab
- Check interactions
- Compare alternatives
- Reviews (6)
- Latest FDA alerts (2)
- Side effects
- Dosage information
- During pregnancy
- Drug class: anti-PD-1 and PD-L1 monoclonal antibodies (immune checkpoint inhibitors)
- Breastfeeding
- En español