Ustekinumab (Monograph)
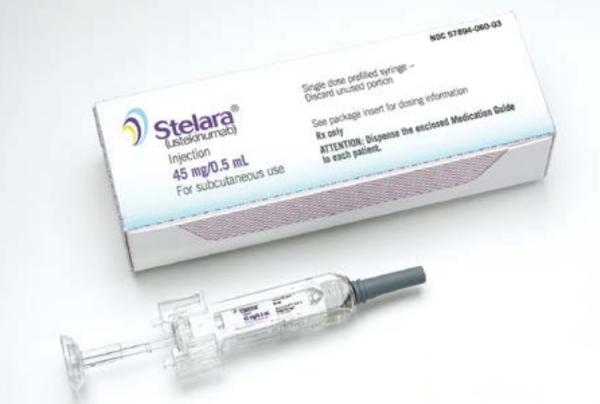
Brand names: Stelara, Wezlana
Drug class: Disease-modifying Antirheumatic Drugs
Introduction
Immunosuppressive agent; a human IgG1 kappa monoclonal antibody directed against the p40 subunit of interleukin-12 (IL-12) and interleukin-23 (IL-23).
Ustekinumab-auub is biosimilar to ustekinumab (Stelara). A biosimilar is a biological that is highly similar to an FDA-licensed reference biological with the exception of minor differences in clinically inactive components and for which there are no clinically meaningful differences in safety, purity, or potency. Biosimilars are approved through an abbreviated licensure pathway that establishes biosimilarity between proposed biological and reference biological but does not independently establish safety and effectiveness of the proposed biological. In order to be considered an interchangeable biosimilar, a biological product must meet additional requirements beyond demonstrating biosimilarity to its reference product. The currently available evidence demonstrates that the ustekinumab biosimilar (Wezlana) is interchangeable with Stelera at the pharmacy level.
In this monograph, unless otherwise stated, the term “ustekinumab products” refers to ustekinumab (the reference drug) and its biosimilar (ustekinumab-auub).
Uses for Ustekinumab
Plaque Psoriasis
Management of moderate to severe plaque psoriasis in adults and pediatric patients ≥6 years of age who are candidates for systemic therapy or phototherapy.
Guidelines generally support the use of ustekinumab in adult and pediatric patients with moderate-to-severe plaque psoriasis.
Recommendations for use and selection of psoriasis therapies vary based on patient age, disease characteristics (e.g., severity, location, presence of psoriatic arthritis), and comorbidities (e.g., inflammatory bowel disease).
Psoriatic Arthritis
Used for the management of active psoriatic arthritis in adults and pediatric patients ≥6 years of age.
Disease-modifying treatments for psoriatic arthritis include oral small molecules (OSMs; e.g., methotrexate, sulfasalazine, cyclosporine, leflunomide, apremilast), biologic DMARDs (e.g., TNF blocking agents, secukinumab, ixekizumab, ustekinumab, brodalumab, abatacept), and/or targeted synthetic DMARDs (e.g., tofacitinib).
Guidelines generally support use of ustekinumab for psoriatic arthritis, although other agents such as a TNF blocking agent, OSM, or interleukin-17 (IL-17) inhibitor are typically preferred.
Recommendations for the use and selection of disease-modifying therapies in psoriatic arthritis vary based on the presence of certain disease characteristics (e.g., psoriatic spondylitis/axial disease, enthesitis) and comorbidities (e.g., inflammatory bowel disease, diabetes).
Crohn Disease
Treatment of moderately to severely active Crohn disease in adults.
Drugs used to treat Crohn disease in adults include 5-aminosalicylates, antibiotics, corticosteroids, immunomodulators, and biologic agents including TNF blocking agents, ustekinumab, vedolizumab, and natalizumab. Guidelines generally recommend use of ustekinumab in patients with moderate-to-severe Crohn disease compared to no treatment or in those who have failed previous treatments. Specific treatments are selected according to the patient’s risk profile and disease severity.
Ulcerative Colitis
Treatment of moderately to severely active ulcerative colitis in adults.
Drugs used to treat ulcerative colitis in adults include oral and rectal 5-aminosalicylates, oral and rectal corticosteroids, immunomodulators (e.g., thiopurines, methotrexate), tofacitinib, and biologic agents, including TNF blocking agents, vedolizumab, and ustekinumab. Guidelines generally recommend ustekinumab for adult outpatients with moderate to severe ulcerative colitis. Specific treatments are selected according to disease severity, disease location/extent, disease prognosis, and previous therapies used.
Ustekinumab Dosage and Administration
General
Pretreatment Screening
-
Consider potential risks and benefits of the drug prior to initiating therapy in patients with chronic infection or history of recurrent infection. Do not administer in patients with a clinically important active infection until the infection resolves or is appropriately treated.
-
Evaluate for active or inactive tuberculosis prior to initiation of ustekinumab therapy. Do not administer to patients with active tuberculosis.
-
Administer all age-appropriate vaccines prior to starting ustekinumab therapy. Do not administer live vaccines during ustekinumab therapy. Do not administer BCG vaccine during ustekinumab therapy or for 1 year before or after ustekinumab therapy.
Patient Monitoring
-
Monitor for signs and symptoms of infection or active tuberculosis during and after treatment.
-
Monitor patients for signs and symptoms of nonmelanoma skin cancer, particularly those >60 years of age, those with a history of prolonged immunosuppressive therapy, and those with a history of psoralen and UVA radiation (PUVA).
-
Monitor all patients for signs and symptoms of posterior reversible encephalopathy syndrome (PRES), a neurologic disorder characterized by headaches, seizures, confusion, visual disturbances, and imaging changes.
Premedication and Prophylaxis
-
Administer an appropriate antimycobacterial regimen for the treatment of latent tuberculosis if indicated prior to initiating ustekinumab therapy.
Administration
Administer by sub-Q injection or IV infusion depending on indication for use.
Administer only to patients who will be closely monitored and have regular follow-up visits with a clinician.
Sub-Q Administration
For sub-Q administration, available as 90-mg/mL solution in 0.5- or 1-mL prefilled syringes and 0.5-mL single-dose vials.
The solution is colorless to light yellow and may contain a few small translucent or white particles.
Administer by sub-Q injection at a different anatomic site (e.g., upper arms, gluteal regions, thighs, any quadrant of the abdomen) than the previous injection. Do not make injections into areas where the skin is tender, bruised, erythematous, or indurated.
When using ustekinumab products in single-dose vial, use a 1-mL syringe with a 27-gauge, ½-inch needle to administer the drug.
Do not shake the injection.
Injection contains no preservative; discard any unused portion.
Intended for use under the supervision of a clinician, but may be self-administered if the clinician determines that the patient and/or their caregiver is competent to prepare and safely administer the drug by sub-Q injection after appropriate training. When used in pediatric patients, manufacturer recommends administration by a clinician.
IV Administration
For IV infusion, available as 5-mg/mL injection concentrate in 26-mL (130-mg) single-dose vials.
Administer using an inline, nonpyrogenic, low-protein-binding 0.2-µm filter.
Do not infuse simultaneously through the same IV line with any other drug.
Dilution
Dilute in 0.9% sodium chloride injection to provide a total volume of 250 mL (i.e., remove a volume of diluent equal to the total required volume of ustekinumab injection concentrate from a 250-mL infusion bag prior to adding the drug concentrate). A 250 mL bag of 0.45% sodium chloride may be used as an alternative. Mix gently.
Do not use diluted solution if visibly opaque particles, discoloration, or foreign particles are observed.
Injection contains no preservative; discard any unused portion. The diluted solution may be stored for up to 7 hours at room temperature (up to 25°C) prior to administration. Completely administer the infusion within 8 hours of dilution in the infusion bag.
Rate of Administration
Administer over at least 1 hour.
Dosage
Use patient's current weight at the time of dosing to determine weight-based doses.
Pediatric Patients
Plaque Psoriasis
Sub-Q
6–17 years of age weighing <60 kg: 0.75 mg/kg at 0 and 4 weeks, then every 12 weeks. For pediatric patients weighing <60 kg, see prescribing information for recommended injection volumes for the recommended dose (0.75 mg/kg).
6–17 years of age weighing 60–100 kg: 45 mg at 0 and 4 weeks, then every 12 weeks.
6–17 years of age weighing >100 kg: 90 mg at 0 and 4 weeks, then every 12 weeks.
Psoriatic Arthritis
Sub-Q
6–17 years of age weighing <60 kg: 0.75 mg/kg at 0 and 4 weeks, then every 12 weeks. For pediatric patients weighing <60 kg, see prescribing information for recommended injection volumes for the recommended dose (0.75 mg/kg).
6–17 years of age weighing ≥60 kg: 45 mg at 0 and 4 weeks, then every 12 weeks.
6–17 years of age weighing >100 kg with coexisting moderate-to-severe plaque psoriasis: 90 mg at 0 and 4 weeks, then every 12 weeks.
Adults
Plaque Psoriasis
Sub-Q
Body weight ≤100 kg: 45 mg at 0 and 4 weeks, then every 12 weeks.
Body weight >100 kg: 90 mg at 0 and 4 weeks, then every 12 weeks. Although 45-mg doses were effective in these patients in clinical studies, 90-mg doses were more effective.
Psoriatic Arthritis
Sub-Q
45 mg at 0 and 4 weeks, then every 12 weeks.
Body weight >100 kg with coexisting moderate-to-severe plaque psoriasis: 90 mg at 0 and 4 weeks, then every 12 weeks.
Crohn Disease or Ulcerative Colitis
IV, then Sub-Q
IV induction: Single dose of 260 mg in patients weighing ≤55 kg, 390 mg in those weighing >55 to 85 kg, and 520 mg in those weighing >85 kg.
Sub-Q maintenance therapy: 90 mg every 8 weeks by sub-Q injection; initiate 8 weeks after the IV induction dose.
Special Populations
Hepatic Impairment
Manufacturer makes no specific dosage recommendations.
Renal Impairment
Manufacturer makes no specific dosage recommendations.
Geriatric Patients
Manufacturer makes no specific dosage recommendations.
Cautions for Ustekinumab
Contraindications
-
History of clinically important hypersensitivity to ustekinumab or any ingredient in the formulation.
Warnings/Precautions
Infectious Complications
May increase risk of infection, including reactivation of latent infections. Serious bacterial, mycobacterial, fungal, and viral infections observed. Serious or clinically important infections (e.g., requiring hospitalization) including cellulitis, diverticulitis, osteomyelitis, viral infections, gastroenteritis, pneumonia, urinary tract infections, appendicitis, cholecystitis, sepsis, anal abscess, ophthalmic herpes zoster, listeriosis, and listeria meningitis reported.
Individuals genetically deficient in IL-12/IL-23 are particularly vulnerable to disseminated infections caused by mycobacteria (including nontuberculous, environmental mycobacteria), salmonella (including nontyphi strains), and BCG vaccine; serious, sometimes fatal, infections reported in such individuals. Not known whether patients with ustekinumab-induced blockade of IL-12/IL-23 are susceptible to these infections. Consider appropriate diagnostic testing for these infections (e.g., tissue culture, stool culture) as dictated by clinical circumstances.
Do not initiate ustekinumab products in patients with any clinically important active infection and do not administer until the infection resolves or is adequately treated. If a serious or clinically important infection develops, consider discontinuing ustekinumab until infection resolves or is adequately treated. Consider potential risks and benefits of the drug prior to initiating therapy in patients with chronic infection or history of recurrent infection.
Evaluate patients for active or latent tuberculosis prior to initiation of ustekinumab products. Do not administer to patients with active tuberculosis. When indicated, initiate appropriate antimycobacterial regimen for treatment of latent tuberculosis prior to ustekinumab therapy. Also consider antimycobacterial therapy prior to ustekinumab therapy in individuals with a history of latent or active tuberculosis in whom an adequate course of antimycobacterial treatment cannot be confirmed. Closely monitor patients for active tuberculosis during and after treatment.
Malignancies
May increase risk of malignancy.
Malignancies (e.g., nonmelanoma skin cancer, prostate cancer, melanoma, colorectal cancer, breast cancer) reported in clinical studies. Incidence of malignancies other than nonmelanoma skin cancer in ustekinumab-treated psoriasis patients similar to expected incidence in general US population.
Inhibition of the p40 subunit of IL-12/IL-23 increased the risk of malignancy in animals. Ultraviolet (UV) radiation-induced skin cancers developed earlier and more frequently in mice genetically manipulated to be deficient in both IL-12 and IL-23 or IL-12 alone. Relevance of these data to risk of malignancy in humans unknown.
Rapid appearance of multiple cutaneous squamous cell carcinomas reported in patients with preexisting risk factors for nonmelanoma skin cancer. Monitor all patients receiving ustekinumab for nonmelanoma skin cancer. Closely monitor patients >60 years of age, those with a history of prolonged immunosuppressive therapy, and those with a history of psoralen and UVA radiation (PUVA) treatment.
Safety of ustekinumab products not evaluated in patients with history of malignancy or with known malignancy.
Sensitivity Reactions
Hypersensitivity Reactions
Hypersensitivity reactions (e.g., anaphylaxis, angioedema, rash, urticaria) reported.
If anaphylactic or other clinically important hypersensitivity reaction occurs, discontinue ustekinumab and institute appropriate therapy.
Latex Sensitivity
The needle cover of the Stelarabrand prefilled syringe contains dry natural rubber and should not be handled by individuals sensitive to latex. However, the needle cover of the Wezlana brand prefilled syringe does not contain dry natural rubber.
Posterior Reversible Encephalopathy Syndrome
Posterior reversible encephalopathy syndrome (PRES), also known as reversible posterior leukoencephalopathy syndrome (RPLS), a neurologic syndrome characterized by reversible vasogenic subcortical edema, reported in clinical trials and postmarketing experience. Patients experienced headaches, seizures, confusion, visual disturbances, and imaging changes.
Signs and symptoms typically occurred within a few days to several months, although some cases reported latency of 1 year or more. Patients recovered after stopping ustekinumab and receiving supportive care.
Monitor patients. If RPLS suspected, discontinue ustekinumab and institute appropriate treatment.
Immunization
Administer all age-appropriate vaccines prior to initiation of ustekinumab therapy.
Avoid live vaccines. Do not administer BCG vaccine during, for 1 year before, or for 1 year after ustekinumab therapy.
Noninfectious Pneumonia
Interstitial pneumonia, eosinophilic pneumonia, and cryptogenic organizing pneumonia reported. Manifestations included cough, dyspnea, and interstitial infiltrates following 1–3 doses of ustekinumab; serious outcomes (e.g., respiratory failure, prolonged hospitalization) also reported. Improvement has occurred following discontinuance of ustekinumab and, in some cases, administration of corticosteroids.
If a diagnosis of interstitial pneumonia, eosinophilic pneumonia, or cryptogenic organizing pneumonia is confirmed, discontinue ustekinumab and institute appropriate treatment,
Immunogenicity
Antibodies to ustekinumab detected, generally in low titers, in 6–12.4% of patients with psoriasis or psoriatic arthritis. In psoriasis patients, anti-ustekinumab antibodies were associated with reduced or undetectable serum ustekinumab concentrations and reduced efficacy; majority of psoriasis patients with anti-ustekinumab antibodies had neutralizing antibodies.
Antibodies to ustekinumab also detected in 2.9 or 4.6% of patients with Crohn's disease or ulcerative colitis, respectively.
No apparent association between antibody development and injection site reactions.
Specific Populations
Pregnancy
Reproductive and developmental toxicity studies in monkeys revealed no evidence of adverse developmental effects on fetuses or neonatal offspring. Data regarding ustekinumab use in pregnant women are insufficient to inform a drug-associated risk.
Lactation
Not known whether ustekinumab distributes into human milk or affects breast-fed infants or milk production. Ustekinumab distributes into milk in monkeys, and maternal IgG distributes into human milk. Systemic exposure to ustekinumab in breast-fed infants is expected to be low since the drug is a large molecule and is degraded in the GI tract. Any effects of local exposure to ustekinumab in the GI tract are unknown.
Consider developmental and health benefits of breast-feeding along with the mother's clinical need for ustekinumab and any potential adverse effects on the breast-fed infant from either the drug or underlying maternal condition.
Pediatric Use
Safety and efficacy established in pediatric patients 6–17 years of age with moderate to severe plaque psoriasis.
Safety and efficacy established in pediatric patients 6–17 years of age with psoriatic arthritis.
Safety and efficacy not established in pediatric patients with Crohn disease or ulcerative colitis or in pediatric patients <6 years of age with psoriasis or psoriatic arthritis.
Geriatric Use
No apparent differences in safety and efficacy relative to younger adults; however, insufficient experience in patients ≥65 years of age to determine whether they respond differently than younger adults.
Common Adverse Effects
Patients with psoriasis (≥3%): Nasopharyngitis, upper respiratory tract infection, headache, fatigue.
Patients with psoriatic arthritis (≥3%): Adverse effects similar to those in patients with psoriasis.
Patients with Crohn disease (≥3%): Vomiting during induction therapy; nasopharyngitis, injection site erythema, vulvovaginal candidiasis/mycotic infection, bronchitis, pruritus, urinary tract infection, sinusitis during maintenance therapy.
Patients with ulcerative colitis (≥3%): Nasopharyngitis during induction therapy; nasopharyngitis, headache, abdominal pain, influenza, fever, diarrhea, sinusitis, fatigue, nausea during maintenance therapy.
Drug Interactions
No formal drug interaction studies to date.
Administered concomitantly with methotrexate, corticosteroids, and/or NSAIAs in clinical studies in psoriatic arthritis.
Drugs Metabolized by Hepatic Microsomal Enzymes
Because increased levels of cytokines (e.g., interleukin-1 [IL-1], interleukin-6 [IL-6], interleukin-10 [IL-10], tumor necrosis factor [TNF; TNF-α], interferon [IFN]) during chronic inflammation may suppress formation of CYP isoenzymes, ustekinumab may normalize formation of CYP enzymes. IL-12 and/or IL-23 did not alter activity of CYP isoenzymes 1A2, 2B6, 2C9, 2C19, 2D6, or 3A4 in vitro; however, clinical relevance not established.
Drugs metabolized by CYP isoenzymes, particularly those with a narrow therapeutic index: Consider monitoring therapeutic effect and serum drug concentrations following initiation of ustekinumab products; adjust dosage as needed.
Vaccines
Avoid live vaccines.
Use caution when administering live vaccines to household contacts of patients receiving ustekinumab products because of potential risk for shedding vaccine organism from household contact and transmission to patient.
Inactive vaccines administered during ustekinumab therapy may not elicit an immune response sufficient to prevent disease.
Specific Drugs and Therapies
|
Drug or Therapy |
Interaction |
Comments |
|---|---|---|
|
Allergy immunotherapy |
Possible decreased protective effect of allergy immunotherapy; possible increased risk of allergic reaction to dose of allergen immunotherapy |
Not evaluated; use with caution in patients who are receiving or have received allergy immunotherapy, particularly for anaphylaxis |
|
Azathioprine |
Concomitant use does not appear to alter ustekinumab clearance or serum concentrations or affect safety or efficacy for Crohn disease or ulcerative colitis |
|
|
BCG vaccine |
Individuals with genetic IL-12/IL-23 deficiency are vulnerable to disseminated infections caused by BCG vaccine |
Do not administer BCG vaccine during, for 1 year before, or for 1 year after ustekinumab therapy |
|
Corticosteroids, oral |
Concomitant use does not appear to alter ustekinumab clearance in patients with psoriatic arthritis Concomitant use does not appear to alter ustekinumab clearance or serum concentrations or affect safety or efficacy for Crohn's disease or ulcerative colitis |
|
|
Cyclosporine |
Possible effect on cyclosporine metabolism; because increased levels of cytokines during chronic inflammation may suppress formation of CYP isoenzymes, ustekinumab may normalize formation of CYP enzymes |
Consider monitoring cyclosporine concentrations following initiation of ustekinumab; adjust dosage as needed |
|
Immunosuppressive agents |
Safety of concomitant therapy in psoriasis patients not established |
|
|
Mercaptopurine |
Concomitant use does not appear to alter ustekinumab clearance or serum concentrations or affect safety or efficacy for Crohn disease or ulcerative colitis |
|
|
Methotrexate |
Concomitant use does not appear to alter ustekinumab clearance or affect safety or efficacy for psoriatic arthritis Concomitant use does not appear to alter ustekinumab clearance or serum concentrations or affect safety or efficacy for Crohn disease or ulcerative colitis |
|
|
NSAIAs |
Concomitant use does not appear to alter ustekinumab clearance |
|
|
Phototherapy |
Increased risk of UV radiation-induced skin cancers in mice with IL-12/IL-23 or IL-12 deficiency; relevance to humans unknown |
Safety of concomitant therapy not established |
|
TNF blocking agents |
Prior TNF blocker use does not appear to alter ustekinumab clearance |
|
|
Warfarin |
Possible effect on warfarin metabolism; because increased levels of cytokines during chronic inflammation may suppress formation of CYP isoenzymes, ustekinumab may normalize formation of CYP enzymes |
Consider monitoring therapeutic effect of warfarin following initiation of ustekinumab; adjust dosage as needed |
Ustekinumab Pharmacokinetics
Absorption
Bioavailability
In psoriasis patients, peak serum concentrations achieved in a median of 13.5 or 7 days following a single sub-Q dose of 45 or 90 mg, respectively. Steady-state concentrations achieved within 28 weeks with multiple-dose sub-Q administration. No apparent accumulation in serum over time when administered sub-Q every 12 weeks.
In patients with Crohn disease or ulcerative colitis receiving recommended induction and maintenance dosages, steady-state concentrations achieved by start of second maintenance dose. No apparent accumulation in serum over time when maintenance doses administered sub-Q every 8 weeks.
Special Populations
Body weight: 90-mg dose in patients with psoriasis or psoriatic arthritis who weigh >100 kg results in median trough serum concentrations comparable to those achieved following 45-mg dose in patients weighing ≤100 kg.
Distribution
Extent
Distributed into milk in lactating monkeys.
Special Populations
Geriatric patients: No apparent change in volume of distribution in psoriasis patients >65 years of age.
Elimination
Metabolism
Metabolic pathway not characterized.
Expected to be degraded into small peptides and amino acids via catabolic pathways in same manner as endogenous IgG.
Half-life
Psoriasis patients: Mean half-life of 14.9–45.6 days following sub-Q administration.
Patients with Crohn's disease or ulcerative colitis: Estimated median terminal half-life of approximately 19 days.
Special Populations
Geriatric patients: No apparent change in clearance in individuals ≥65 years of age.
Stability
Storage
Parenteral
Injection
2–8°C; do not freeze. Store in original carton to protect from light until administration. Store vials upright.
Individual prefilled syringes may be stored at room temperature (up to 30°C) for one single period that does not exceed 30 days or more. Do not return the syringe to the refrigerator following storage at room temperature. If the drug has not been used within 30 days, discard the syringe.
Injection Concentrate
2–8°C; do not freeze. Store in original carton to protect from light until administration. Store vials upright.
Diluted solution: 7 hours at room temperature (≤25°C) prior to administration. Complete administration of the infusion within 8 hours of dilution in the infusion bag.
Actions
-
Binds with high affinity and specificity to the p40 subunit of both IL-12 and IL-23.
-
IL-12 and IL-23 are naturally occurring cytokines involved in inflammatory and immune responses, such as natural killer cell activation and CD4+ T-cell differentiation and activation.
-
IL-12 and IL-23 contribute to chronic inflammation associated with Crohn's disease and ulcerative colitis; in animal models of colitis, genetic absence or antibody blockade of the p40 subunit of IL-12 and IL-23 was protective.
-
Disrupts IL-12- and IL-23-mediated signaling and cytokine cascades by disrupting the interaction of these cytokines with a shared cell-surface receptor chain, IL-12 β1.
-
Produced with a murine cell line using standard bioprocessing technology.
Advice to Patients
-
Instruct patients to read the manufacturer’s patient information (medication guide) prior to initiation of therapy and each time the prescription is refilled.
-
Instruct patient and/or caregiver regarding proper dosage and administration of ustekinumab products, including the use of aseptic technique, and proper disposal of needles and syringes if it is determined that the patient and/or caregiver is competent to safely administer the drug.
-
Inform patients that ustekinumab products may lower the ability of their immune system to fight infections. Importance of contacting clinicians if any signs or symptoms of infection develop.
-
Risk of malignancies while receiving ustekinumab products.
-
Advise patients to discontinue use of ustekinumab products and seek immediate medical attention if they experience any symptoms of serious allergic reactions.
-
Advise patients that the needle cover of the Stelara brand prefilled syringe contains dry natural rubber, which may cause allergic reactions in individuals sensitive to latex. The prefilled syringe needle cover of Wezlana brand does not contain dry natural rubber.
-
Advise patients that ustekinumab products can interfere with the usual response to immunizations and that they should avoid receiving live vaccines during ustekinumab therapy.
-
Advise patients to inform their clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements (e.g., St. John’s wort), as well as any concomitant illnesses.
-
Advise women to inform their clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Inform patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Injection concentrate, for IV infusion |
5 mg/mL |
Stelara |
Janssen Biotech |
|
Injection, for subcutaneous use |
45 mg/0.5 mL |
Stelara (available as single-use prefilled syringes and single-use vials) |
Janssen Biotech |
|
|
90 mg/mL |
Stelara (available as single-use prefilled syringes) |
Janssen Biotech |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Injection concentrate, for IV infusion |
5 mg/mL |
Wezlana |
Amgen |
|
Injection, for subcutaneous use |
45 mg/0.5 mL |
Wezlana (available as single-use prefilled syringes and single-use vials) |
Amgen |
|
|
90 mg/mL |
Wezlana (available as single-use prefilled syringes) |
Amgen |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions November 27, 2023. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Frequently asked questions
- What are the new drugs for plaque psoriasis?
- How many biosimilars have been approved in the United States?
- How quickly or how long before Stelara starts to work?
- How long can you keep Stelara in or out of the fridge?
- Can you get a flu shot or take antibiotics while on Stelara?
- How is Stelara injected or administered?
- What blood tests are needed for Stelara?
More about ustekinumab
- Check interactions
- Compare alternatives
- Reviews (256)
- Side effects
- Dosage information
- During pregnancy
- Drug class: interleukin inhibitors
- Breastfeeding
- En español