Osteoarthritis
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What is osteoarthritis?
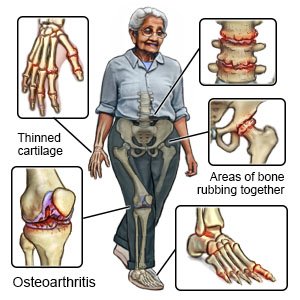
Osteoarthritis (OA) occurs when cartilage (tissue that cushions a joint) wears away slowly and causes the bones to rub together. OA is a long-term condition that often affects the hands, neck, lower back, knees, and hips. OA is also called arthrosis or degenerative joint disease.
 |
What increases my risk for OA?
- Age older than 50 years
- A family history of OA
- Obesity, high blood pressure, or high blood sugar
- A joint injury or infection
- Repetitive movements of your joints at work or during sports
What are the signs and symptoms of OA?
- Joint pain that gets worse when you move the joint
- Joint stiffness that decreases after you move the joint
- Decreased range of movement
- Hard, bony enlargement on your fingers or toes
- A grinding or cracking sound when you move your joint
How is OA diagnosed?
X-rays are pictures of the bones in your joint. Contrast liquid may be injected into your joint before the x-ray. The liquid will help your joint show up better on the x-ray. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid.
How is OA treated?
The goals of treatment are to decrease pain, increase strength, and improve movement. You may need any of the following:
- Medicines:
- Acetaminophen decreases pain and fever. It is available without a doctor's order. Ask how much to take and how often to take it. Follow directions. Read the labels of all other medicines you are using to see if they also contain acetaminophen, or ask your doctor or pharmacist. Acetaminophen can cause liver damage if not taken correctly.
- NSAIDs , such as ibuprofen, help decrease swelling, pain, and fever. This medicine is available with or without a doctor's order. NSAIDs can cause stomach bleeding or kidney problems in certain people. If you take blood thinner medicine, always ask your healthcare provider if NSAIDs are safe for you. Always read the medicine label and follow directions.
- Capsaicin cream may help decrease pain in your joint.
- Prescription pain medicine may be given. Ask your healthcare provider how to take this medicine safely. Some prescription pain medicines contain acetaminophen. Do not take other medicines that contain acetaminophen without talking to your healthcare provider. Too much acetaminophen may cause liver damage. Prescription pain medicine may cause constipation. Ask your healthcare provider how to prevent or treat constipation.
- A steroid injection may be given if your symptoms get worse.
- Physical therapy may be used to teach you exercises to help improve movement and strength, and to decrease pain. A physical therapist may move an area with his or her hands. For example, he or she may move your leg in certain ways to treat osteoarthritis in your hip.
- Ultrasound may be used to treat osteoarthritis in certain areas, such as your knee. Ultrasound produces heat that can relieve pain.
- Surgery may be needed if other treatments do not work.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
How can I manage my symptoms?
- Stay active. Physical activity may reduce your pain and improve your ability to do daily activities. Avoid activities that cause pain. Ask your healthcare provider what type of exercise would be best for you.
- Maintain a healthy weight. This helps decrease the strain on the joints in your back, hips, knees, ankles, and feet. Ask your healthcare provider what a healthy weight is for you. He or she can help you create a weight loss plan if you are overweight.
- Use heat or ice on your joints as directed. Heat and ice help decrease pain, swelling, and muscle spasms. For heat, use a heating pad on a low setting for 20 minutes, or take a warm bath. For ice, use an ice pack, or put crushed ice in a plastic bag. Cover it with a towel before you place it on your joint. Use ice for 15 minutes every hour.
- Massage the muscles around the joint. Massage helps relieve pain and stiffness. Your healthcare provider or a physical therapist can show you how to do this. If you have hip OA, another person may need to help you massage the area.
- Use a cane, crutches, or a walker if directed. These help protect and relieve pressure on your ankle, knee, and hip joints. You may also be prescribed shoe inserts to decrease pressure in your joints.
- Wear flat or low-heeled shoes. This will help decrease pain and reduce pressure on your ankle, knee, and hip joints.
When should I call my doctor?
- You have severe pain.
- You cannot move your joint.
- You have a fever.
- Your joint is red and tender.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Osteoarthritis
- Top 9 Things You Must Know About Naproxen
- What are the risks of mixing pain medications and alcohol?
Treatment options
Care guides
Symptoms and treatments
Medicine.com guides (external)
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
