Strabismus in Children
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What is strabismus?
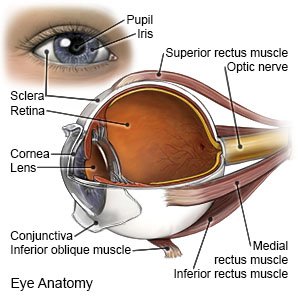
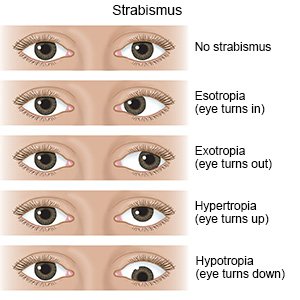
Strabismus is a condition that causes your child's eyes to look in different directions. Your child's eye muscles do not work together to control his or her eye movement. This condition may only occur sometimes, or it may be present all the time.
 |
What causes strabismus?
- Weak or paralyzed eye muscles
- Head or eye injury that damages eye function
- Tumors that press on the muscles or nerves around the eyes
- Damage or swelling of the retina in premature babies
What are the signs and symptoms of strabismus?
- Your child has an eye that wanders or turns in, out, down, or up.
- Your child says his or her eyes hurt or are tired after reading or focusing on an object.
- Your child looks at you with one eye closed or his or her head turned to the side.
- Your child has headaches.
- Your child has blurred vision, double vision, or increased sensitivity to bright lights.
How is strabismus diagnosed?
Your child's healthcare provider will ask about your child's symptoms and examine his or her eyes. Your child may need any of the following tests:
- A vision exam is done to check if strabismus has affected your child's vision. Your child will be asked to look at letters, pictures, and shapes on reading charts at a close and far distance.
- An eye exam will include a light reflex test and a fundoscopic test. A light reflex test compares how each eye reacts to the light. The pen light is flashed in front of his or her eyes and moved slowly from side to side. A fundoscopic test uses an instrument with a bright light to check for damage to the blood vessels inside your child's eyes.
- A cover test may be done by your child's healthcare provider. Your child looks at an object up close and at a distance with one eye covered. Then your child looks at the object with the other eye covered. The healthcare provider will watch your child's eyes to see how they respond.
- A refraction test measures the prescription your child needs for eyeglasses. Your child will be asked to look at a chart through a device that has lenses of different strengths. Your child will be asked if the word or picture is clear as the healthcare provider changes the lenses.
How is strabismus treated?
- An eye patch over your child's stronger eye may be needed. This will help your child's weaker eye to work more and get stronger.

- Eye exercises help improve your child's eye movement and focus. Ask the healthcare provider about the best eye exercises for him or her.
- Eyeglasses can help your child's eyes work together.
- Surgery may be done to change the length or position of your child's eye muscles. This will help to straighten his or her eyes.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
When should I call my child's eye doctor?
- Your child loses vision in one or both eyes.
- Your child has a severe headache, dizziness, or vomiting.
- Your child has a fever.
- Your child has new or worsening blurred or double vision.
- You have questions or concerns about your child's condition or care.
Care Agreement
You have the right to help plan your child's care. Learn about your child's health condition and how it may be treated. Discuss treatment options with your child's healthcare providers to decide what care you want for your child. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Strabismus
Treatment options
Care guides
Symptoms and treatments
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
