Liver Transplant
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
WHAT YOU NEED TO KNOW:
Liver transplant is surgery to replace part or all of your liver with a healthy liver from another person.
 |
HOW TO PREPARE:
Weeks and days before your surgery:
- Do not drink alcohol for at least 6 months before your transplant.
- Your healthcare provider may order medicines for you to take while you wait for your transplant. For example, you may need immune globulin or antiviral medicines if you have viral hepatitis. These medicines may help decrease the amount of virus in your body before surgery.
- You may need liver support before your transplant to decrease the level of toxins (waste) in your blood. Liver support may include plasma exchange or hemodialysis.
- You may need a CT, MRI, or abdominal ultrasound. Tests such as Doppler ultrasound and a chest x-ray may also be done.
- Arrange to have someone drive you home after surgery.
- Tell your surgeon about all medicines you currently take. He or she will tell you if you need to stop any medicine for surgery, and when to stop. He or she will tell you which medicines to take or not take on the day of surgery.
- You may need a blood transfusion if you lose a large amount of blood during surgery. You may be able to donate your own blood before surgery. This is called autologous blood donation. This must be done no later than 3 days before surgery. You may also ask a family member or friend with the same blood type to donate blood for you. This is called directed blood donation.
The night before your surgery:
You may be told not to eat or drink anything after midnight.
The day of your surgery:
- You or a close family member will be asked to sign a legal document called a consent form. It gives healthcare providers permission to do the procedure or surgery. It also explains the problems that may happen, and your choices. Make sure all your questions are answered before you sign this form.
- Take only the medicines your surgeon told you to take.
- An IV will be placed in a vein. You may be given medicine or liquids through the IV.
- An anesthesiologist will talk to you before your surgery. Tell him or her if you or anyone in your family has had a problem with anesthesia.
- You may need blood and urine tests done the day of surgery to check your organ function. The tests may also be done to check for infection, or any recent alcohol or drug use.
- Medicines may be given to prevent a bacterial infection. You may also need medicine to help prevent your body from rejecting your new liver.
- A central line (a type of IV catheter) may be placed. The central line may be used to give medicines or IV fluids. It may also be hooked up to a monitor to take certain blood pressure readings. This information helps healthcare providers check how well your heart is working.
WHAT WILL HAPPEN:
What will happen:
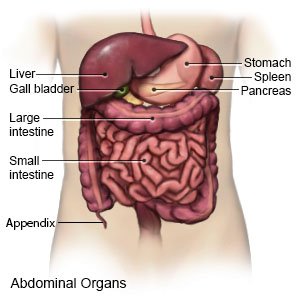
- General anesthesia will keep you asleep and free from pain during surgery. Your surgeon will make incisions under each side of your ribcage. There will also be an incision made down the middle of your abdomen. Muscles and other tissues will be moved aside to help your surgeon see your liver better. The blood vessels attached to your liver will be cut and closed to stop any bleeding. The blood flow to your liver will be stopped during surgery.
- Your surgeon will remove your liver and place the donor liver. He or she will connect the blood vessels of the donor liver to your blood vessels. Blood will then be able to flow through your new liver. Then, your surgeon will attach your bile duct to the donor liver's bile duct. He or she may use stitches, surgical glue, or a laser beam to stop any bleeding. Drains will be placed around your liver to remove any extra blood and fluid after surgery. Your incision will be closed with stitches and covered with a bandage.
After surgery:
- You will be taken to the recovery room then the intensive care unit (ICU). Healthcare providers will watch you closely to make sure you are okay. A healthcare provider may remove the bandages soon after your surgery to check your wound and drains.
- You will have several tubes in place, which might make it hard to move. All of these tubes are important to help your healthcare providers know about any problems. The drains are taken out when the incision stops draining. Do not get out of bed until your healthcare provider says it is okay.
CONTACT YOUR HEALTHCARE PROVIDER IF:
- You have a fever.
- You have a skin infection or an infected wound on or near your abdomen.
- You have questions or concerns about your surgery.
Seek Care Immediately if
- Your signs and symptoms get worse.
Risks
You may bleed more than expected or get an infection. The fluids used during your surgery may build up in your abdomen and lungs. Extra fluid may make it hard for you to breathe. Nerves, blood vessels, muscles, intestines, and other organs may get damaged. Your blood pressure may decrease, or you may have abnormal heartbeats during surgery. You may develop a life-threatening blood clot in your arm or leg. Your condition may get worse during surgery, and may become life-threatening. Your body may reject the new liver.
Related medications
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
