Hypotension
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
Hypotension is a blood pressure (BP) that is lower than it should be. Hypotension may be mild, serious, or life-threatening.
 |
DISCHARGE INSTRUCTIONS:
Call your local emergency number (911 in the US) if:
- You become confused or cannot speak.
- You have a seizure.
- You have chest pain or trouble breathing.
Seek care immediately if:
- You urinate very little or not at all.
- You have changes in vision or cannot see.
Call your doctor or specialist if:
- You vomit several times or have diarrhea, and you cannot drink liquid.
- You have a fever.
- You have new or increased symptoms, such as dizziness, weakness, or fainting.
- Your legs, ankles, and feet are swollen, or you gain weight for no known reason.
- You have questions or concerns about your condition or care.
Related medications
Treatment options
The following list of medications are related to or used in the treatment of this condition.
Medicines:
You may need any of the following:
- Alpha-adrenoreceptor agonists may increase your BP and decrease your symptoms.
- Steroids help prevent salt loss from your body. Steroids may also help increase the amount of fluid in your body and raise your BP.
- Vasopressors help constrict (make smaller) your blood vessels and increase your BP. Vasopressor medicines may increase the blood flow to your brain and help decrease your symptoms.
- Antidiuretic hormone helps control your BP and helps decrease your need to urinate during the night.
- Antiparkinson medicine may help increase your standing BP and decrease your symptoms.
- Erythropoietin increases the amount of red blood cells you have. More red blood cells increases your blood volume, and may increase your standing BP. This medicine may also treat anemia and problems with your nervous system.
- Antibiotics may be needed to treat a bacterial infection.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
Manage hypotension:
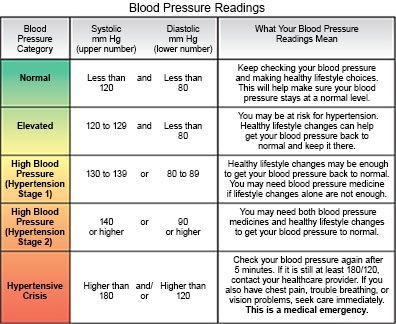
- Check your blood pressure as directed. Record the results and bring them with you to follow-up visits. Ask when and how often to check your BP. You may be given a BP monitor to wear for up to 24 hours. This will record your blood pressure during your normal daily activities. The monitor will take your BP every 15 to 30 minutes. Try to keep still while your BP is taken. Avoid heavy activity, such as exercise, while you are wearing the monitor.

- Change positions slowly. When you get out of bed, sit up first, then slowly move your legs to the side of the bed. If you are not having any symptoms, slowly stand up. If you have symptoms, sit down right away.
- Exercise and do physical counter maneuvers. Ask your healthcare provider or specialist about the best exercise plan for you. Physical counter maneuvers may help to increase your BP and increase blood flow to your heart. They include crossing your legs, squatting, and bending at the waist. You can also rise up on your toes while you are standing, and tighten your thigh muscles.
- Drink liquids as directed. Ask your provider or specialist how much liquid to drink each day and which liquids are best for you. Drink 500 milliliters (½ liter) of liquid quickly in the morning or before meals to help increase your BP. Your provider may tell you to drink 2 cups of coffee with, or after, breakfast and lunch. The caffeine in the coffee can help prevent a drop in your BP. Your provider may also give you caffeine pills.
- Change how you eat meals. If your BP drops after eating large meals, try to eat smaller meals more often. Eat foods low in carbohydrates and cholesterol to help prevent BP drops after you eat. Ask if you need to increase the amount of sodium (salt) you eat each day.
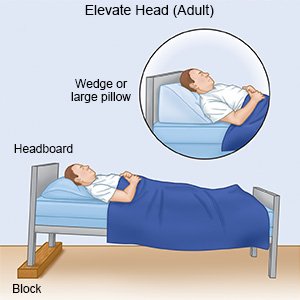
- Raise the head of your bed. Raise the head of your bed 4 to 8 inches. This may help prevent morning BP drops and decrease the need to urinate during the night.
Avoid anything that makes your hypotension worse:
- Do not drink alcohol. Alcohol can make your symptoms worse. Ask for information if you need help quitting.
- Avoid straining. Activities and movements that cause you to strain can cause a drop in your BP. Activities to avoid include lifting, coughing, and other movements that increase the feeling of pressure in your chest.
- Avoid the heat. Heat can decrease your BP. Stay inside during very hot days, or limit the amount of time you are outside. Do not take hot baths.
Follow up with your doctor or specialist as directed:
Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Hypotension
Treatment options
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
