Covid-19 (Coronavirus Disease 2019)
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
AMBULATORY CARE:
What you need to know about COVID-19:
COVID-19 is the disease caused by a coronavirus first discovered in December 2019. The virus has changed into several new forms (called variants) since it was discovered. A variant may be more easily spread or cause more severe illness than the original form.
Signs and symptoms of COVID-19
Signs and symptoms usually start about 5 days after infection but can take 2 to 14 days. You may feel like you have the flu or a bad cold. Some signs and symptoms go away in a few days. Others can last weeks, months, or possibly years. You may have any of the following:
- A cough or sore throat
- Shortness of breath or trouble breathing that may become severe
- A fever, possibly with chills and shaking
- Muscle pain, body aches, or a headache
- Sudden changes in or loss of your taste or smell
- Feeling mentally and physically tired (fatigue)
- Congestion (stuffy head and nose), or a runny nose
- Diarrhea, nausea, or vomiting
Call your local emergency number (911 in the US) if:
- You have trouble breathing or shortness of breath at rest.
- You have chest pain or pressure that lasts longer than 5 minutes.
- You become confused or hard to wake.
Seek care immediately if:
- You have trouble staying awake during the day.
- Your nail beds, face, fingers, or toes look blue or darker than usual.
Call your doctor if:
- You have a fever.
- You have questions or concerns about your condition or care.
How COVID-19 is diagnosed:
Your healthcare provider will examine you and ask about your symptoms. Tell your provider if you have any health conditions or are taking any medicines. Your provider can help you create a COVID-19 plan if you are at high risk for severe illness. Some tests are available for you to do at home. Most use a nasal swab and give the result within 15 minutes. Testing sites may also be available. Test immediately if you have symptoms. Wait 5 days after exposure if you do not have symptoms. Any of the following tests may be used:
- A PCR test shows if you have a current infection. A sample is taken from your nose or throat with a swab. You may need to quarantine until you get the results from a testing site.
- An antigen test shows if you have a protein from the COVID-19 virus. This test is often called a rapid test because the results are available in 30 minutes or less. Without symptoms, you need 3 negative antigen results to be certain you do not have COVID-19. With symptoms, you need 2 negative results. Antigen tests should be taken 48 hours apart. A negative PCR result is considered confirmation of the first negative antigen result.
- An antibody test shows if you had a recent or past infection. Blood samples are used for this test. Antibodies are made by your immune system to fight the virus that causes COVID-19. Antibodies form 1 to 3 weeks after you are infected. This test is not used to show if you are immune to the virus.
- A CT, MRI, ultrasound, or x-ray may show complications of COVID-19, such as pneumonia or blood clots.
Treatment
may include any of the following:
- Mild symptoms may get better on their own. Some treatments have emergency use authorization (EUA). Examples include monoclonal antibodies and convalescent plasma. These may be given to help prevent worsening of your symptoms. You may also need any of the following:
- Decongestants help reduce nasal congestion and help you breathe more easily. If you take decongestant pills, they may make you feel restless or cause problems with your sleep. Do not use decongestant sprays for more than a few days.
- Cough suppressants help reduce coughing. Ask your healthcare provider which type of cough medicine is best for you.
- To soothe a sore throat, gargle with warm salt water, or use throat lozenges or a throat spray. Drink more liquids to thin and loosen mucus and to prevent dehydration.
- NSAIDs or acetaminophen can help lower a fever and relieve body aches or a headache. Follow directions. If not taken correctly, NSAIDs can cause kidney damage and acetaminophen can cause liver damage.
- Antiviral medicines may be given if you are at risk for developing severe or life-threatening symptoms.
- Severe or life-threatening symptoms are treated in the hospital. You may need any of the following:
- Medicines may be given to fight the virus or treat inflammation.
- Blood thinners help prevent or treat blood clots. If you have a deep vein thrombosis (DVT) or pulmonary embolism (PE), you may need to use blood thinners for at least 3 months.
- Extra oxygen may be given if you have respiratory failure. This means your lungs cannot get enough oxygen into your blood and out to your organs.
- A ventilator may be used to help you breathe.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
What you need to know about long COVID:
Long COVID is a term to describe health problems the virus may cause.
- Certain conditions increase your risk for long COVID. Your risk is higher if you are 65 or older or a current or former smoker. A weak immune system, obesity, diabetes, or kidney, heart, or lung disease can also increase your risk.
- Long COVID may cause severe or chronic health problems. The most common problem is trouble thinking, remembering, or concentrating. You may also develop shortness of breath or a serious respiratory condition such as pneumonia. Blood clots may form and lead to organ damage. You may have nerve pain, trouble sleeping, or mood changes.
- COVID-19 can lead to severe inflammation in your organs. This is also called multisymptom inflammatory syndrome in adults (MIS-A) or MIS-C in children. Inflammation may affect the heart, digestive system, skin, or brain.
What you need to know about COVID-19 vaccines:
Healthcare providers recommend vaccination, even if you already had COVID-19.
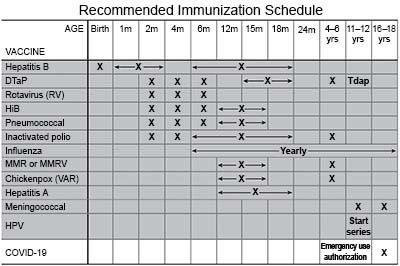
- Get a COVID-19 vaccine as directed. At least 1 dose of an updated vaccine is recommended for everyone 6 months or older. COVID-19 vaccines are given as a shot in 1 to 3 doses, depending on the age of the person who receives it. COVID-19 vaccines are updated throughout the year. Your healthcare provider can help you schedule all needed doses as updated vaccines become available.
- Continue to protect yourself and others. You can become infected even after you get the vaccine. You may also be able to pass the virus to others without knowing you are infected.
- After you get the vaccine, check local, national, and international travel rules. You may need to be tested before you travel. Some countries require proof of a negative test before you travel. You may also need to quarantine after you return.
- Medicine may be given to prevent infection. The medicine can be given if you are at high risk for infection and cannot get the vaccine. It can also be given if your immune system does not respond well to the vaccine.
How the virus spreads:
The virus can be spread starting 2 to 3 days before symptoms begin. Close personal contact with an infected person increases your risk for infection. This means being within 6 feet (2 meters) of the person for at least 15 minutes over 24 hours.
- The virus travels in droplets that form when a person talks, sings, coughs, or sneezes. The droplets can also float in the air for minutes or hours. Infection happens when you breathe in the droplets or get them in your eyes or nose.
- Person-to-person contact can spread the virus. For example, a person with the virus on his or her hands can spread it by shaking hands with someone.
- The virus can stay on objects and surfaces for hours to days. You may become infected by touching the object or surface and then touching your eyes or mouth.
Help lower your risk for COVID-19 during an active outbreak:
- Stay home if you are sick or think you may have COVID-19. It is important to stay home if you are waiting for a testing appointment or for test results.
- Wash your hands often throughout the day. Use soap and water. Rub your soapy hands together, lacing your fingers, for at least 20 seconds. Rinse with warm, running water. Dry your hands with a clean towel or paper towel. Use hand sanitizer that contains alcohol if soap and water are not available. Teach children how to wash their hands and use hand sanitizer.

- Cover sneezes and coughs. Turn your face away and cover your mouth and nose with a tissue. Throw the tissue away. Use the bend of your arm if a tissue is not available. Then wash your hands well with soap and water or use hand sanitizer. Teach children how to cover a cough or sneeze.
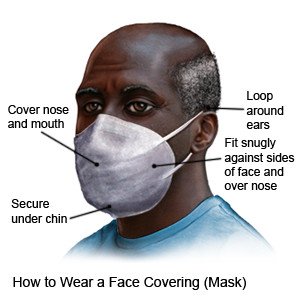
- Wear a face covering (mask) when needed. Use a cloth covering with at least 2 layers. You can also create layers by putting a cloth covering over a disposable non-medical mask. Cover your mouth and your nose.
- Try to keep space between you and others when you are out of the house. Avoid crowds as much as possible. Wear a face covering when you must be around a large group and cannot keep space between you and others.
- Clean and disinfect high-touch surfaces and objects often. Use disinfecting wipes, or make a solution of 4 teaspoons of bleach in 1 quart (4 cups) of water.
- Ask about other vaccines you may need. Get the influenza (flu) vaccine as soon as recommended each year, usually starting in September or October. Get the pneumonia and respiratory syncytial virus (RSV) vaccines, if recommended. Your healthcare provider can tell you if you should also get other vaccines, and when to get them.
 |
Follow up with your doctor as directed:
Write down your questions so you remember to ask them during your visits.
For more information:
- Centers for Disease Control and Prevention
1600 Clifton Road
Atlanta , GA 30333
Phone: 1- 800 - 232-4636
Web Address: http://www.cdc.gov
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Covid-19
Treatment options
Medicine.com guides (external)
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
