Bradycardia
Medically reviewed by Drugs.com. Last updated on Sep 23, 2025.
AMBULATORY CARE:
Bradycardia
is a slow heart rate, usually fewer than 60 beats per minute. A slow heart rate is normal for some people, such as athletes, and needs no treatment. Bradycardia may also be caused by health conditions that do need treatment. Your healthcare provider will tell you what heart rate is too low for you.
 |
Other signs and symptoms that may occur with bradycardia:
- Tiredness and shortness of breath
- Dizziness
- Lightheadedness
- Confusion
- Chest pain
- Cool and pale or bluish skin
Call your local emergency number (911 in the US) or have someone call if:
- You have new or worsening dizziness, shortness of breath, chest pain, or confusion.
Call your doctor or cardiologist if:
- You feel lightheaded or faint.
- Your pulse rate is lower than healthcare providers say it should be, even with treatment.
- You are more tired than usual, even with treatment.
- You have questions or concerns about your condition or care.
How bradycardia is diagnosed:
Your healthcare provider will ask about your symptoms. Tell him or her when they started and how often they happen. Tell him or her how severe your symptoms usually are, and how long they last. He or she will ask what triggers your symptoms and if anything makes them worse or better. He or she may ask if you have a heart condition or take any medicines. Tell your provider if symptoms happen after you take certain medicines. Tell him or her if you have a family history of heart conditions. You may also need any of the following:
- Blood tests may be done to see if you have any heart damage. They may also be used to find the cause of your bradycardia.
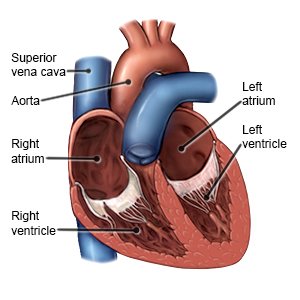
- Echocardiography is a type of ultrasound. Sound waves are used to create pictures of your heart as it beats.
- An ECG records the electrical activity of your heart. It may be used to check for heart damage from a heart attack or problems with the way electrical signals travel through your heart. You may be asked to walk on a treadmill during this test to check if exercise triggers symptoms.
- CT or MRI pictures may show problems with your heart that can cause bradycardia. Contrast liquid may be used to help your heart show up better in the pictures. Tell the healthcare provider if you had an allergic reaction to contrast liquid. Do not enter the MRI room with any metal. Metal can cause serious damage. Tell the provider if you have any metal in or on your body.
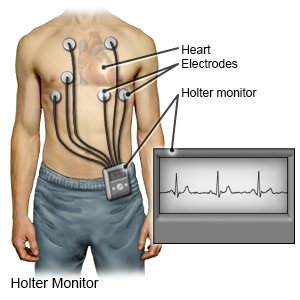
- A heart monitor will be used to track your heart rate and rhythm if you are in the hospital. You may also need to wear it for several days at home.
Treatment
may not be needed. Bradycardia is usually treated if it causes symptoms, such as dizziness or fainting. The cause of your bradycardia may need to be treated. For example, you may need treatment for sleep apnea if this is causing your symptoms. Your healthcare provider will talk with you about the benefits and risks of treatment that may be right for you:
- Heart medicines may be given to increase your heart rate. These medicines are given through an IV.
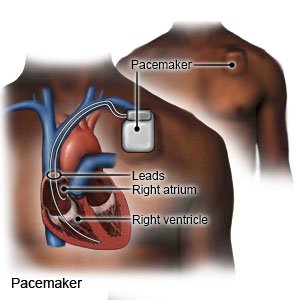
- A temporary pacemaker is a short-term treatment in the hospital. The pacemaker is applied to your skin with sticky pads or placed into a vein in your neck or chest. A small pacing device helps keep your heartbeat stable.
- A permanent pacemaker is implanted under the skin of your chest or abdomen during surgery. A tiny battery creates electrical impulses that keep your heart rate regular.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
Manage or prevent bradycardia:
- Talk to your healthcare provider about all your current medicines. He or she may change a medicine if it is causing your slow heart rate. Do not stop taking any medicine unless directed by your provider.
- Keep a record of your symptoms. Include when you have bradycardia, and what you were doing when it started. Also include anything that made your symptoms better or worse. Bring the record to follow-up visits with your healthcare providers.
- Do not smoke. Nicotine and other chemicals in cigarettes and cigars can cause heart and lung damage. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
- Reach or maintain a healthy weight. Your healthcare provider can tell you what a healthy weight is for you. He or she can help you create a weight loss plan if needed. Weight loss can help strengthen your heartbeat. If you have sleep apnea, weight loss may help you breathe more regularly while you sleep.
- Exercise as directed. Exercise can help strengthen your heart. It can also help you manage your weight and improve your sleep. Your healthcare provider can help you create an exercise plan. He or she may recommend 30 to 40 minutes of exercise most days of the week.
- Eat a variety of healthy foods. Healthy foods include fruits, vegetables, whole-grain breads and cereals, low-fat dairy products, lean meats, fish, and cooked beans. Depending on the cause of your bradycardia, your healthcare provider may recommend a heart healthy diet. This diet is low in sodium (salt) and unhealthy fats. A dietitian or your healthcare provider can help you create a heart healthy diet.

Follow up with your doctor or cardiologist as directed:
Write down your questions so you remember to ask them during your visits. You may need to see specialists for more treatment. If you have a pacemaker, your cardiologist needs to make sure that it is working as it should.
For more information:
- American Heart Association
7272 Greenville Avenue
Dallas , TX 75231-4596
Phone: 1- 800 - 242-8721
Web Address: http://www.heart.org
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Bradycardia
Treatment options
- Medications for Bradyarrhythmia
- Medications for Sinus Node Dysfunction
- Medications for Tachyarrhythmia
Care guides
Symptoms and treatments
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
