Bladder Diverticulectomy
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
AMBULATORY CARE:
What you need to know about bladder diverticulectomy:
Bladder diverticulectomy is surgery to repair or remove diverticula. These are pouches attached to your bladder by a piece of tissue called a neck. They form when an obstruction (block) stops urine from flowing. Pressure builds up in the bladder and pushes the lining through the bladder wall. Diverticulectomy is often done for several diverticula. It may be done if you have only one (called a diverticulum) that is large or preventing you from urinating. A diverticulum may become infected or contain cancer. Your surgeon may drain an infected diverticulum during surgery.
 |
How to prepare for surgery:
- You may need several tests before your surgery. A cystoscopy is a procedure to look inside your urethra and bladder with a cystoscope. A cystoscope is a small tube with a light and magnifying camera on the end. A sample of your urine may also be tested for signs of infection. An infection will need to be treated before you have a diverticulectomy. Ultrasound, MRI, or voiding cystourethrography pictures may be used to check the diverticula or your bladder. An obstruction (block) in your urethra found during one of these tests will need to be removed before you have a diverticulectomy.
- Your healthcare provider will tell you how to prepare for surgery. Tell your provider about all the medicines you currently take. aspirin, and ibuprofen several days before your procedure. You will be told which medicines to take or not take on the day of surgery. You may be told not to eat or drink anything after midnight on the day of your surgery.
What will happen during surgery:
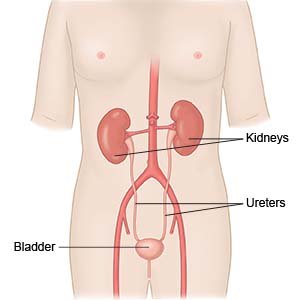
- You will be given general anesthesia to keep you asleep and pain-free during surgery. A Foley catheter will be guided into your bladder through your urethra. The catheter is used to empty urine from your bladder during surgery. Later in the surgery, it is used to fill the bladder with liquid. Stents may be placed in your ureters to help protect them from injury during surgery. A stent is a soft tube placed inside the ureter to keep it open. Your surgeon will tell you how long the stents need to stay in place. They may need to stay in for 2 weeks.
- You may have open surgery or laparoscopic surgery. For open surgery, you will have 1 longer incision in your abdomen. Your surgeon will do this surgery only through this incision. Laparoscopic means your surgeon makes small incisions near the diverticula. He or she will guide a laparoscope into one of the incisions. This is a tube with a camera on the end. Your surgeon will guide tools into the other incisions.
- Your surgeon will cut the neck of the diverticulum from the bladder. He or she will then remove the diverticulum. It may be sent to a lab to be tested for cancer. Your surgeon will close up the cut this makes in the bladder. The bladder will be filled with liquid to check for leaks and then drained. The surgery incisions on the outside of your body will be closed and covered with a bandage. A suprapubic catheter may also be left in place after surgery. This is a tube that enters the skin through the lower abdomen and goes into the bladder.
What to expect after surgery:
- The Foley catheter, and possibly the suprapubic catheter, will still be in place after surgery. These may stay in place for up to a week to help drain urine from your bladder. Your bladder may be irrigated (washed out) continuously for the first day or two after surgery.
- Healthcare providers will help you walk safely for a short time after surgery. When you walk on the same day after surgery, you help prevent blood clots.
Risks of bladder diverticulectomy:
You may bleed more than expected during surgery. You may also develop an infection. Your ureter or bowel may be injured. You may develop a fistula, urinary tract infection (UTI), or an abscess (pocket of pus). You may also leak urine.
Related medications
Seek care immediately if:
- Your surgery wound is red, swollen, or draining pus.
- You have a fever of 101°F (38°3C) or higher.
- You have side or back pain that gets worse.
Contact your healthcare provider if:
- You have bright red blood, pus, or blood clots in your urine.
- You have a mild fever.
- You have questions or concerns about your condition or care.
Medicines:
You may need any of the following:
- Antibiotics are used to prevent or treat a bacterial infection.
- Prescription pain medicine may be given. Ask your healthcare provider how to take this medicine safely. Some prescription pain medicines contain acetaminophen. Do not take other medicines that contain acetaminophen without talking to your healthcare provider. Too much acetaminophen may cause liver damage. Prescription pain medicine may cause constipation. Ask your healthcare provider how to prevent or treat constipation.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
Care for your catheter:
Keep the bag below your waist. This will prevent urine from flowing back into your bladder and causing an infection or other problems. Keep the tube straight so the urine will drain properly. Do not pull on the catheter. This can cause pain and bleeding and may cause the catheter to come out. Empty your urine drainage bag when it is ½ to ⅔ full, or every 8 hours. If you have a smaller leg bag, empty it every 3 to 4 hours. Do the following when you empty your urine drainage bag:
- Hold the urine bag over the toilet or a large container.
- Remove the drain spout from its sleeve at the bottom of the urine bag. Do not touch the tip of the drain spout. Open the slide valve on the spout.
- Let the urine flow out of the urine bag into the toilet or container. Do not let the drainage tube touch anything.
- Clean the end of the drain spout with alcohol when the bag is empty. Ask which cleaning solution is best to use.
- Close the slide valve and put the drain spout into its sleeve at the bottom of the urine bag. Write down how much urine was in your bag if you were asked to keep a record.
Self-care:
- Care for your surgery wound as directed. Ask your healthcare provider when your wound can get wet. Carefully wash around the wound with soap and water. Let soap and water run over your wound. Do not scrub your wound. Dry the area and put on new, clean bandages as directed. Change your bandages when they get wet or dirty. If you have strips of medical tape, let them fall off on their own. Check for signs of infection, such as red streaks, swelling, or pus.
- Drink liquids as directed. Your healthcare provider may recommend that you drink 6 to 8 eight-ounce cups of water every day for 2 days after your procedure.
- Ask when you can return to regular daily activities. Do not have sex until your healthcare provider tells you it is okay. Sex may increase your risk for a urinary tract infection.
Follow up with your healthcare provider as directed:
Your provider will tell you when to come in to have your Foley or suprapubic catheter removed. You may also need to have uretal stents removed. Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
