Ticagrelor Side Effects
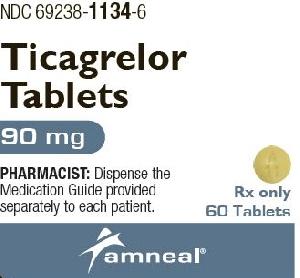
Applies to ticagrelor: oral tablet.
Important warnings
This medicine can cause some serious health issues
Oral route (tablet)
Ticagrelor can cause significant, sometimes fatal, bleeding.
Do not use in patients with active pathological bleeding or history of intracranial hemorrhage.
Do not start in patients undergoing urgent CABG.
If possible, manage bleeding without discontinuing ticagrelor.
Stopping ticagrelor increases the risk of subsequent cardiovascular events.
Maintenance doses of aspirin above 100 mg in patients with acute coronary syndrome reduce the effectiveness of ticagrelor and should be avoided.
Precautions
It is very important that your doctor check your progress at regular visits. This will allow your doctor to see if the medicine is working properly and to decide if you should continue to take it. Blood tests may be needed to check for unwanted effects.
Tell all medical doctors, dentists, nurses, and pharmacists you go to that you are taking this medicine. Ticagrelor may increase the risk of serious bleeding during a surgery, other medical procedures (eg, coronary artery bypass graft or CABG), or some kinds of dental work. You may need to stop using this medicine at least 5 days before a surgery, medical procedure, or dental work. The results of some medical tests may also be affected by this medicine.
Do not change your dose or Stop taking ticagrelor without checking first with your doctor. To do so may increase the chance of having a heart attack, blood clotting problems, or other serious conditions.
While you are using this medicine, if you have any kind of bleeding, it may take longer than usual to stop, especially if you hurt yourself. Stay away from rough sports or other situations where you could be bruised, cut, or injured. Be careful when using sharp objects, including razors and fingernail clippers.
This medicine may increase your chance of bleeding or bruising. Check with your doctor right away if you notice any unusual bleeding or bruising, black, tarry stools, blood in the urine or stools, or pinpoint red spots on your skin. Avoid picking your nose. If you need to blow your nose, blow it gently.
Tell your doctor right away if you have chest tightness, or difficult or trouble breathing when asleep or awake. These could be symptoms of a serious lung or breathing problem (eg, central sleep apnea, Cheyne-Stokes respiration).
This medicine may cause heart rhythm problems (eg, bradyarrhythmia). Check with your doctor right away if you have chest pain or discomfort, lightheadedness, dizziness, or fainting, trouble breathing, slow or irregular heartbeat, or unusual tiredness.
Do not take other medicines unless they have been discussed with your doctor. This includes prescription or nonprescription (over-the-counter [OTC]) medicines and herbal or vitamin supplements.
Serious side effects of ticagrelor
Along with its needed effects, ticagrelor may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking ticagrelor:
More common side effects
- back pain
- bleeding gums
- blurred vision
- chest pain, tightness, or discomfort
- confusion
- cough
- coughing up blood
- difficult or trouble breathing
- dizziness, faintness, or lightheadedness when getting up suddenly from a lying or sitting position
- fast, slow, or irregular heartbeat
- headache
- increased menstrual flow or vaginal bleeding
- lightheadedness, dizziness, or fainting
- loss of consciousness
- nausea or vomiting
- nervousness
- nosebleeds
- paralysis
- pounding in the ears
- prolonged bleeding from cuts
- red or black, tarry stools
- red or dark brown urine
- sweating
- unusual bleeding or bruising
- unusual tiredness or weakness
Rare side effects
- change in mental status
- difficulty in speaking
- fever
- pale skin
- pinpoint red spots on the skin
- seizures
- yellow eyes or skin
Incidence not known
- difficulty with swallowing
- large, hive-like swelling on the face, eyelids, lips, tongue, throat, hands, legs, feet, or sex organs
- rash
Other side effects of ticagrelor
Some side effects of ticagrelor may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
Less common side effects
- diarrhea
See also:
Plavix
Plavix (clopidogrel) is used to prevent blood clots after a recent heart attack or stroke. Includes ...
Brilinta
Brilinta (ticagrelor) is used to lower your risk of having a stroke or serious heart problems after ...
Ozempic
Learn about Ozempic (semaglutide) for type 2 diabetes treatment, weight management, cardiovascular ...
Valsartan
Valsartan is an angiotensin II receptor blocker (ARB) that may be used to treat high blood pressure ...
Atenolol
Atenolol is used to treat angina (chest pain) and hypertension (high blood pressure). Learn about ...
Warfarin
Warfarin is an anticoagulant used to prevent heart attacks, strokes, and blood clots. Learn about ...
Propranolol
Propranolol is a beta-blocker that is used to treat tremors, chest pain, high blood pressure, heart ...
Clopidogrel
Clopidogrel is used for acute coronary syndrome, acute coronary syndrome, prophylaxis, heart ...
Aspirin
Aspirin is used to treat mild to moderate pain and to reduce fever or inflammation. Learn about ...
Metoprolol
Metoprolol is used to treat angina (chest pain) and hypertension (high blood pressure). Learn about ...
For healthcare professionals
Applies to ticagrelor: oral tablet.
General adverse events
The most commonly reported side effects were bleeding and dyspnea.[Ref]
Hematologic
- Very common (10% or more): Bleeding (12%)
- Postmarketing reports: Thrombotic thrombocytopenic purpura[Ref]
In the PLATO study (PLATelet Inhibition and Patient Outcomes, n= 18,624), 9235 patients were treated with ticagrelor 90 mg orally twice a day. Patients were evaluated for non-CABG related major or minor bleeds compared to clopidogrel (n=9186). A minor bleed required medical intervention to stop or treat bleeding, whereas a major bleed included any of the following: fatal, intracranial, intrapericardial with cardiac tamponade, hypovolemic shock or severe hypotension requiring intervention, significantly disabling (e.g., intraocular with permanent vision loss), a decrease in hemoglobin of at least 3 g/dL (or a fall in hematocrit of at least 9%), or a transfusion of 2 or more units. A major bleed that was fatal/life-threatening was any of the events described as a major bleed plus a decrease in hemoglobin of more than 5 g/dL, a fall in hematocrit of at least 15%, or a transfusion of 4 or more units. A fatal bleed was a bleeding event that directly led to death within 7 days. For ticagrelor, the incidence of major and minor bleeds was 7.7% (clopidogrel 6.2%). These findings are broken down as followed: Major bleed (3.9%) major bleed fatal/life threatening (1.9%), fatal (0.2%), and intracranial hemorrhage fatal/life threatening (0.3%). Approximately half of the non-CABG major bleeding events occurred in the first 30 days.
In the PLATO study, when antiplatelet therapy was stopped 5 days prior to CABG, major bleeding occurred in 75% and 79% of patients receiving ticagrelor or clopidogrel, respectively.[Ref]
Respiratory
- Very common (10% or more): Dyspnea (up to 21%)
- Common (1% to 10%): Epistaxis, cough
- Uncommon (0.1% to 1%): Hemoptysis
- Postmarketing reports: Central sleep apnea, Cheyne-Stokes respiration[Ref]
During the PLATO study, (PLATelet Inhibition and Patient Outcomes, n= 18,624), dyspnea was reported in 13.8% of ticagrelor-treated patients, it was usually mild to moderate in intensity and often resolved during continued treatment, however, drug discontinuation was required in 0.9% of patients. In the PEGASUS study (n=21,162), 4.3% of patients taking ticagrelor 60 mg orally twice a day discontinued treatment due to dyspnea compared to 0.7% receiving aspirin alone. In a substudy of PLATO, 199 subjects underwent pulmonary function testing irrespective of whether they reported dyspnea. There was no indication of an adverse effect on pulmonary function assessed after one month or after at least 6 months of chronic treatment. During the THEMIS study (n=19,220), dyspnea was reported in 21% of ticagrelor-treated patients which led to drug discontinuation in 6.9% of patients.[Ref]
Cardiovascular
- Common (1% to 10%): Ventricular pauses, cardiovascular death, non-fatal myocardial infarction, non-fatal stroke, bradycardia, cardiac failure, atrial fibrillation, peripheral edema, hypertension, hypotension, syncope, pre-syncope
- Uncommon (0.1% to 1%): Non-cardiac chest pain
- Postmarketing reports: Atrioventricular block[Ref]
In a Holter substudy of approximately 3000 patients from the PLATelet Inhibition and Patient Outcomes study, (PLATO, n= 18,624), more patients had ventricular pauses 3 seconds or longer with ticagrelor (6%) than with clopidogrel (3.5%) in the acute phase and 2.2% and 1.6% respectively after 1 month. Patients that were at an increased risk for bradycardic events were excluded from these studies. Patients with congestive heart failure (CHF) who were taking ticagrelor experienced ventricular pauses at a higher rate (9.2%) than those without CHF (5.4).[Ref]
Renal
- Common (1% to 10%): Serum creatinine elevations[Ref]
During the PLATO study, (PLATelet Inhibition and Patient Outcomes, n= 18,624), serum creatinine levels increased by more than 50% in 7.4% of patients receiving ticagrelor 90 mg orally. Levels did not continue to increase with ongoing treatment and often decreased with continued therapy. Reversibility occurred upon discontinuation even in those patients with the greatest increase in levels during treatment. Treatment groups did not differ for renal related serious adverse events (e.g. acute renal failure, chronic renal failure, toxic nephropathy, or oliguria).[Ref]
Musculoskeletal
- Common (1% to 10%): Back pain
- Rare (0.01% to 0.1%): Hemarthrosis[Ref]
Hypersensitivity
- Postmarketing reports: Hypersensitivity reactions including angioedema[Ref]
Nervous system
- Common (1% to 10%): Dizziness, loss of consciousness
- Uncommon (0.1% to 1%): Intracranial hemorrhage, paresthesia, headache[Ref]
Gastrointestinal
- Common (1% to 10%): Abdominal pain, dyspepsia, gastrointestinal hemorrhage, nausea, diarrhea, constipation, vomiting
- Uncommon (0.1% to 1%): Retroperitoneal hemorrhage, gastritis, hematemesis, gastrointestinal ulcer hemorrhage, hemorrhoidal hemorrhage, oral hemorrhage[Ref]
Metabolic
- Uncommon (0.1% to 1%): Gout
- Rare (0.01% to 0.1%): Hyperuricemia[Ref]
In the PLATelet Inhibition and Patient Outcomes Study (PLATO, n= 18,624) the serum uric acid levels of patients taking ticagrelor 90 mg orally twice a day increased approximately 0.6 mg/dL from baseline. The difference disappeared within 30 days of stopping treatment. Gout occurred in 0.6% of patients.[Ref]
Genitourinary
- Common (1% to 10%): Urinary tract bleeding
- Uncommon (0.1% to 1%): Vaginal bleeding[Ref]
Dermatologic
- Common (1% to 10%): Rash, pruritus, subcutaneous or dermal bleeding, bruising[Ref]
Ocular
- Uncommon (0.1% to 1%): Eye hemorrhage[Ref]
Other
- Common (1% to 10%): Vertigo, post procedural hemorrhage, fatigue, pyrexia
- Uncommon (0.1% to 1%): Ear hemorrhage, wound hemorrhage, traumatic hemorrhage[Ref]
Psychiatric
- Rare (0.01% to 0.1%): Confusion[Ref]
References
1. Cerner Multum, Inc. "UK Summary of Product Characteristics."
2. Cerner Multum, Inc. "Australian Product Information."
3. (2011) "Product Information. Brilinta (ticagrelor)." Astra-Zeneca Pharmaceuticals
Frequently asked questions
- How long do I have to take Brilinta after a stent or heart attack?
- What pain medication can I take with Brilinta?
- How long should Brilinta be held/stopped before surgery?
- Brilinta vs Plavix: what's the difference?
- Is there a generic for Brilinta?
- Is ticagrelor better than clopidogrel?
- What is Brilinta (ticagrelor) used for?
- Is ticagrelor a prodrug?
More about ticagrelor
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (117)
- Drug images
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: platelet aggregation inhibitors
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Ticagrelor side effects can vary depending on the individual. Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Note: Medication side effects may be underreported. If you are experiencing side effects that are not listed, submit a report to the FDA by following this guide.