Tagamet Side Effects
Generic name: cimetidine
Medically reviewed by Drugs.com. Last updated on Oct 10, 2024.
Note: This document provides detailed information about Tagamet.
Applies to cimetidine: oral liquid and tablets, parenteral injection, parenteral injection for iv infusion only Side Effects associated with cimetidine. Some dosage forms listed on this page may not apply specifically to the brand name Tagamet.
Applies to cimetidine: oral liquid and tablets, parenteral injection, parenteral injection for iv infusion only.
Side effects include:
Headache, dizziness, somnolence, diarrhea.
With ≥1 month of therapy: gynecomastia.
With IM therapy: transient pain at injection site.
For healthcare professionals
Applies to cimetidine: compounding powder, intravenous solution, oral liquid, oral tablet.
Renal adverse events
- Very common (10% or more): Increased plasma creatinine (up to 11%)
- Rare (0.01% to 0.1%): Interstitial nephritis[Ref]
Interstitial nephritis cleared with drug withdrawal.
Creatinine elevations usually occurred during the first week of treatment and were typically non-progressive, with values returning to pretreatment levels during therapy or up to 1 week after stopping treatment.[Ref]
Gastrointestinal
- Common (1% to 10%): Constipation, diarrhea, flatulence, nausea, vomiting
- Rare (0.01% to 0.1%): Acute pancreatitis/pancreatitis[Ref]
Pancreatitis cleared with drug withdrawal.[Ref]
Musculoskeletal
- Common (1% to 10%): Musculoskeletal pain, myalgia/reversible myalgia
- Rare (0.01% to 0.1%): Arthralgia/reversible arthralgia, exacerbation of joint symptoms, polymyositis[Ref]
Nervous system
- Common (1% to 10%): Dizziness, drowsiness, headache[Ref]
Headaches occurred more frequently in patients given 1600 mg/day compared to patients given 800 mg/day.
Somnolence and dizziness were usually mild and have been reported in patients receiving 800 to 1600 mg/day.[Ref]
Dermatologic
- Common (1% to 10%): Rash/skin rashes
- Rare (0.01% to 0.1%): Hypersensitivity vasculitis
- Very rare (less than 0.01%): Epidermal necrolysis, erythema multiforme, generalized exfoliative erythroderma, reversible alopecia, severe generalized skin reactions, Stevens-Johnson syndrome
- Frequency not reported: Severe skin rash[Ref]
Hypersensitivity vasculitis usually cleared with drug withdrawal.[Ref]
Other
- Common (1% to 10%): Tiredness
- Rare (0.01% to 0.1%): Fever[Ref]
Fever cleared with drug withdrawal.[Ref]
Psychiatric
- Uncommon (0.1% to 1%): Confusional state, depression, hallucination
- Frequency not reported: Agitation, anxiety, disorientation, mental confusion, psychosis[Ref]
Confusional states occurred within 2 to 3 days of starting treatment, were reversible within 3 to 4 days of stopping treatment and were more commonly reported in elderly patients and/or ill patients (e.g., renal dysfunction, organic brain syndrome).[Ref]
Hepatic
- Uncommon (0.1% to 1%): Hepatitis, reversible liver damage
- Rare (0.01% to 0.1%): Cholestatic effects, increased serum transaminases, mixed cholestatic-hepatocellular effects
- Very rare (less than 0.01%): Fatal hepatic effects
- Frequency not reported: Periportal hepatic fibrosis, severe parenchymal injury[Ref]
Hepatitis and serum transaminase level elevations cleared with drug withdrawal.
Fatal hepatic effects have occurred with other histamine-2 receptor antagonists.
Severe parenchymal injury is considered highly unlikely due to the predominance of cholestatic features.
There was a report of biopsy-proven periportal hepatic fibrosis in a patient receiving this drug.[Ref]
Hematologic
- Uncommon (0.1% to 1%): Leukopenia
- Rare (0.01% to 0.1%): Agranulocytosis, aplastic anemia, decreased white blood cell counts, pancytopenia, thrombocytopenia
- Very rare (less than 0.01%): Immune hemolytic anemia[Ref]
Leukopenia and/or thrombocytopenia were reversible with withdrawal of treatment.
Agranulocytosis/decreased white blood cell counts have been reported, with some events recurring upon rechallenge. These events were more commonly reported in patients with serious concomitant illnesses and/or those who received drugs/treatments known to produce neutropenia.[Ref]
Cardiovascular
- Uncommon (0.1% to 1%): Tachycardia
- Rare (0.01% to 0.1%): Atrioventricular (AV) heart block/heart block, sinus bradycardia[Ref]
Genitourinary
- Uncommon (0.1% to 1%): Reversible impotence
- Rare (0.01% to 0.1%): Urinary retention
- Very rare (less than 0.01%): Galactorrhea[Ref]
Urinary retention cleared with drug withdrawal.[Ref]
Endocrine
- Uncommon (0.1% to 1%): Gynecomastia[Ref]
Hypersensitivity
- Rare (0.01% to 0.1%): Allergic reactions, anaphylaxis[Ref]
Allergic reactions and anaphylaxis usually cleared with drug withdrawal.[Ref]
Immunologic
- Very rare (less than 0.01%): Strongyloidiasis hyperinfection[Ref]
Respiratory
In a large epidemiological study, it was suggested that patients taking histamine-2-receptor antagonists had an increased adjusted relative risk of 1.63 (95% confidence interval of 1.07 to 2.48) of developing pneumonia compared to patients who stopped treatment. However, causal relationship between H2RA use and pneumonia has not been established.[Ref]
See also:
References
1. (2001) "Product Information. Tagamet (cimetidine)." SmithKline Beecham
2. (2002) "Product Information. Tagamet HB (cimetidine)." SmithKline Beecham
3. Cerner Multum, Inc. "UK Summary of Product Characteristics."
4. Cerner Multum, Inc. "Australian Product Information."
Frequently asked questions
More about Tagamet (cimetidine)
- Check interactions
- Compare alternatives
- Reviews (6)
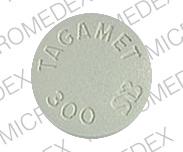
- Drug images
- Dosage information
- During pregnancy
- Drug class: H2 antagonists
- Breastfeeding
Professional resources
Other formulations
Related treatment guides
Further information
Tagamet side effects can vary depending on the individual. Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Note: Medication side effects may be underreported. If you are experiencing side effects that are not listed, submit a report to the FDA by following this guide.