Trihexyphenidyl (Monograph)
Drug class: Anticholinergic Agents
VA class: AU350
CAS number: 52-49-3
Introduction
Antimuscarinic antiparkinsonian agent.
Uses for Trihexyphenidyl
Parkinsonian Syndrome
Symptomatic management of all forms of parkinsonian syndrome, including idiopathic parkinson disease and parkinsonism resulting from encephalitis (postencephalitic parkinsonism) or cerebral arteriosclerosis.
Has been used as monotherapy or as adjunctive therapy in the treatment of parkinson disease.
Levodopa is currently the most effective drug for relieving motor symptoms of parkinson disease; however, long-term use associated with motor complications. To avoid these complications, may initiate treatment with other antiparkinsonian agents first and postpone use of levodopa. Some clinicians state that anticholinergic agents (e.g., trihexyphenidyl, benztropine) may be particularly useful for initial therapy in patients <60 years of age with resting tremors as their only or most prominent symptom.
Although main use of anticholinergic agents in parkinson disease is to control tremors, evidence of a benefit largely anecdotal.
Drug-induced Extrapyramidal Reactions
Control of extrapyramidal symptoms (EPS) induced by antipsychotic agents (e.g., phenothiazines, thioxanthenes).
Anticholinergic agents (e.g., trihexyphenidyl, benztropine) are used traditionally to restore acetylcholine and dopamine imbalance in patients with antipsychotic-induced EPS; however, evidence supporting a benefit is lacking or inconsistent and the drugs are associated with a variety of adverse effects.
In general, use cautiously and for minimum duration necessary to control EPS.
Trihexyphenidyl Dosage and Administration
Administration
Oral Administration
Administer orally (as tablets or oral solution) before or after meals, depending on patient reaction. May be preferable to administer before meals in patients with excessive xerostomia (unless nausea is a problem) and after meals in patients prone to excessive salivation.
Tolerability may be increased if total daily dosage is administered in divided doses 3 times daily with meals; if a fourth dose is required (such as with dosages >10 mg daily), administer at bedtime.
Mint candies, chewing gum, water, or a saliva substitute may be used to relieve xerostomia that may accompany administration after meals.
Dosage
Available as trihexyphenidyl hydrochloride; dosage expressed in terms of the salt.
Adjust dosage carefully according to individual requirements and response. Initiate with low dosage and increase gradually to desired effect.
Adults
Parkinsonian Syndrome
Oral
Initially, 1 mg on first day. Dosage may be increased in 2-mg increments at 3- to 5-day intervals up to a maximum of 6–10 mg daily.
Parkinson disease: Usual maintenance dosage is 2 mg 3 times daily.
Postencephalitic patients: Dosages up to 12–15 mg daily may be required.
When used as an adjunct to levodopa, consider reducing dosage of both drugs. Generally, a dosage of 3–6 mg daily of trihexyphenidyl hydrochloride given in divided doses is adequate.
When transitioning from another antimuscarinic agent to trihexyphenidyl, increase trihexyphenidyl dosage as needed while decreasing dosage of other drug until complete replacement is achieved.
Drug-Induced Extrapyramidal Reactions
Oral
Usual total daily dosage: 2–15 mg.
Initially, 1 mg; if EPS not controlled within a few hours, progressively increase dose until control is achieved.
Alternatively, to achieve more rapid control, reduce dosage of the drug causing the reaction, then adjust dosage of both drugs to attain the desired drug effect without EPS. Once control of EPS has been maintained for several days, dosage of trihexyphenidyl may be reduced or discontinued.
Prescribing Limits
Adults
Parkinsonian Syndrome
Oral
Maximum of 6–10 mg daily in most patients; postencephalitic patients may require 12–15 mg daily.
Special Populations
Hepatic Impairment
No specific dosage recommendations at this time.
Renal Impairment
No specific dosage recommendations at this time.
Geriatric Patients
Patients ≥60 years of age: Manufacturer states to initiate with low dosage; titrate dosage gradually. (See Geriatric Use under Cautions.)
Cautions for Trihexyphenidyl
Contraindications
-
Known hypersensitivity to trihexyphenidyl or any ingredient in the formulation.
-
Some manufacturers state drug is contraindicated in patients with narrow angle glaucoma. Blindness after long-term use due to narrow angle glaucoma has been reported.
Warnings/Precautions
Warnings
Ophthalmic Effects
Possible increased ocular tension. Possible precipitation of glaucoma in patients receiving prolonged therapy.
Use with caution in patients with glaucoma.
Periodic gonioscopic evaluation and intraocular pressure monitoring recommended.
General Precautions
Tardive Dyskinesia
Antiparkinsonian agents do not alleviate symptoms of tardive dyskinesia and may aggravate these symptoms.
Cardiovascular Effects
Possible tachycardia; use with caution and carefully monitor patients with cardiac disease or hypertension.
GU Effects
Possible urinary hesitancy and retention; use with caution and carefully monitor patients with prostatic hypertrophy or obstructive disease of the GU tract.
CNS Effects
Possible mental confusion, disorientation, behavioral disturbances, agitation, hallucinations, and psychotic-like symptoms.
GI Effects
Possible decreased intestinal mobility, paralytic ileus, and constipation; use with caution in patients with obstructive diseases of the GI tract.
Specific Populations
Geriatric Use
Possibility exists of greater sensitivity to the drug in some geriatric individuals. Careful dosage selection necessary. Some experts state to avoid use in geriatric patients because of unfavorable balance of benefits and risks compared with alternative treatments.
Hepatic Impairment
Careful monitoring recommended.
Renal Impairment
Careful monitoring recommended.
Common Adverse Effects
Dry mouth, blurred vision, dizziness, nausea, nervousness.
Drug Interactions
Specific Drugs
|
Drug |
Interaction |
|
|---|---|---|
|
Anticholinergic agents |
Increased risk of adverse anticholinergic effects |
Trihexyphenidyl Pharmacokinetics
Absorption
Rapidly absorbed from the GI tract following oral administration.
Onset
Following oral administration, onset of action occurs within 1 hour.
Duration
6–12 hours.
Elimination
Elimination Route
Excreted principally in urine, probably as unchanged drug.
Stability
Storage
Oral
Oral Solution
20–25°C.
Tablets
20–25°C.
Actions
-
Exhibits atropine-like action and exerts antispasmodic effects on parasympathetic-innervated peripheral structures, including smooth muscle.
-
Exact mechanism of action in parkinsonian syndrome not understood; may result from blockade of efferent impulses and from central inhibition of cerebral motor centers.
-
Competitively inhibits acetylcholine or other cholinergic stimuli at autonomic effectors innervated by postganglionic nerves.
-
Exhibits weak mydriatic, antisialagogue, and cardiovagal blocking effects.
Advice to Patients
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements, as well as concomitant illnesses.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Solution |
2 mg/5 mL* |
Trihexyphenidyl Hydrochloride Oral Solution |
|
|
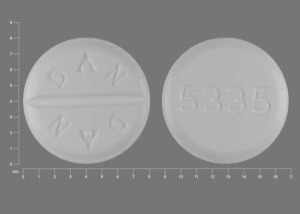
Tablets |
2 mg* |
Trihexyphenidyl Hydrochloride Tablets |
||
|
5 mg* |
Trihexyphenidyl Hydrochloride Tablets |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions March 8, 2022. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
More about trihexyphenidyl
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (24)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: anticholinergic antiparkinson agents
- Breastfeeding
- En español