Sotalol
Pronunciation: so-TAH-loll
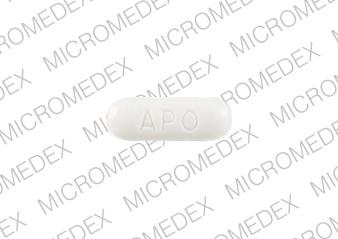
Generic name: sotalol
Brand names: Betapace, Betapace AF, Sorine, Sotalol Hydrochloride AF, Sotylize
Dosage form: intravenous solution (15 mg/mL), oral solution (5 mg/mL), oral tablet (120 mg; 160 mg; 240 mg; 80 mg; AF 120 mg; AF 160 mg; AF 80 mg)
Drug classes: Group III antiarrhythmics, Non-cardioselective beta blockers
What is sotalol?
Sotalol is a beta-blocker with antiarrhythmic properties that affects the heart and circulation within the atrium and ventricles (the upper and lower chambers of the heart that allow blood to flow into and out of the heart).
Sotalol may be used to help keep the heart beating normally in people with certain documented heart rhythm disorders, such as atrial fibrillation, atrial flutter, ventricular tachycardia, and ventricular fibrillation. Sotalol may also be used for other purposes.
Sotalol was first FDA-approved on October 30, 1992.
Warnings
You should not use sotalol if you have asthma, low potassium, or a serious heart condition such as severe heart failure, long QT syndrome, slow heartbeats that have caused you to faint, "sick sinus syndrome" or "AV block" (unless you have a pacemaker).
Monitoring in a facility that can provide cardiac resuscitation, continuous electrocardiographic monitoring, and calculations of creatinine clearance for a minimum of 3 days is recommended for patients initiating or reinitiating sotalol to minimize the risk of induced arrhythmia.
May cause life-threatening ventricular tachycardia associated with QT interval prolongation.
IV sotalol treatment should not be initiated if the baseline QTc is longer than 450ms. Reduce the dosage or discontinue if the interval extends to 500 ms or greater.
Do not substitute one brand of sotalol for another without your doctor’s advice because of potentially significant differences in labeling, dosing and administration, and safety information.
Before taking sotalol
You should not use sotalol if you are allergic to it, or any of the inactive ingredients in the tablets, or if you have:
- a serious heart condition such as "sick sinus syndrome" or "AV block" (unless you have a pacemaker)
- long QT syndrome (in you or a family member)
- severe heart failure
- slow heartbeats that have caused you to faint
- asthma or other breathing disorder
- very low levels of potassium in your blood or
- (if you take sotalol for atrial fibrillation or atrial flutter) severe kidney disease;
Do not give sotalol to a child without medical advice.
Tell your doctor if you have ever had:
- kidney disease (or if you are on dialysis)
- an electrolyte imbalance (such as low levels of potassium or magnesium in your blood)
- congestive heart failure
- coronary artery disease (hardened arteries)
- breathing problems such as bronchitis or emphysema
- a thyroid disorder
- diabetes (using sotalol can make it harder for you to tell when you have low blood sugar)
- a severe allergic reaction.
Tell your doctor about all the medications you take. Any with antiarrhythmic properties may need to be discontinued before starting sotalol.
Tell your doctor if you are pregnant. Sotalol can cross the placenta and affect the unborn baby, causing problems such as growth restriction, transient slow heartbeat in the fetus, laboratory changes, QT prolongation, uterine contractions, and other adverse effects. Talk with your doctor about using sotalol before you get pregnant. If you inadvertently become pregnant while taking sotalol, or are currently pregnant, discuss the risks vs benefits of using sotalol with your doctor.
You should not breastfeed while using sotalol.
How should I take sotalol?
Follow all directions on your prescription label and read all medication guides or instruction sheets. Your doctor may occasionally change your dose. Use the medicine exactly as directed.
- Sotalol oral is taken by mouth. Your healthcare provider may increase or decrease this dose depending on how you respond.
- The recommended initial dosage in adults is 80mg twice daily.
- Sotalol doses for children are based on age and body surface area (height and weight). Your child's dose needs may change if the child gains or loses weight, or is still growing. Use a calibrated measure to administer the correct dose if your child is prescribed sotalol oral solution.
- The first few doses of sotalol will be given in a hospital setting where your heart can be monitored in case the medicine causes serious side effects.
- If you already take heart rhythm medication, you may need to stop taking it when you start using sotalol. Carefully follow your doctor's instructions.
Call your doctor if you are sick with vomiting or diarrhea, or if you have increased thirst, decreased appetite, or are sweating more than usual. You can easily become dehydrated while taking sotalol. This can lead to very low blood pressure, a serious electrolyte imbalance, or kidney failure.
You will need frequent medical tests. Your heart function may need to be checked using an electrocardiograph or ECG (sometimes called an EKG). You may also need heart function tests for 1 to 2 weeks after your last dose.
Keep using this medicine as directed, even if you feel well. You may need to take sotalol for the rest of your life.
Do not skip doses or stop using sotalol without your doctor's advice. Stopping suddenly may make your condition worse. Follow your doctor's instructions about tapering your dose.
If you need surgery, tell your surgeon you currently use this medicine.
There is an intravenous formulation of sotalol which may be substituted for oral sotalol after a dosage adjustment in people unable to take oral medications or for faster achievement of steady-state levels. A healthcare provider will give you this injection as an infusion into your vein.
What happens if I miss a dose?
Skip the missed dose and use your next dose at the regular time. Do not double the dose or shorten the dosing interval.
Try not to miss any doses. Get your prescription refilled before you run out of medicine completely.
What happens if I overdose?
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222. An overdose of sotalol can be fatal.
What are the side effects of sotalol?
Get emergency medical help if you have signs of an allergic reaction such as hives; difficulty breathing; or swelling of your face, lips, tongue, or throat.
Sotalol may cause serious side effects. Call your doctor at once if you have:
- chest pain
- fast or pounding heartbeats, fluttering in your chest
- sudden dizziness (like you might pass out)
- slow heartbeats (especially if you feel light-headed)
- swelling, rapid weight gain or
- feeling short of breath.
Common side effects of sotalol may include:
- a slow heartbeat
- nausea or vomiting
- shortness of breath
- dizziness or
- feeling weak or tired.
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.
Related/similar drugs
Xarelto
Xarelto (rivaroxaban) is a factor Xa inhibitor used to reduce the risk of blood clots and stroke in ...
Propafenone
Propafenone systemic is used for atrial fibrillation, atrial flutter, ventricular tachycardia ...
Benlysta
Benlysta infusion is used to treat active systemic lupus erythematosus (SLE) and active lupus ...
Lanoxin
Lanoxin (digoxin) is used to treat congestive heart failure and atrial fibrillation. Includes ...
Magnesium sulfate
Magnesium sulfate systemic is used for barium poisoning, hypomagnesemia, seizure prevention ...
Cardizem
Cardizem is used to treat hypertension (high blood pressure), angina (chest pain), and heart rhythm ...
Flecainide
Flecainide systemic is used for atrial fibrillation, atrial flutter, paroxysmal supraventricular ...
Rivaroxaban
Rivaroxaban systemic is used for atrial fibrillation, cardiovascular risk reduction, congenital ...
Digoxin
Digoxin is used to treat congestive heart failure and to slow the heart rate in patients with ...
What should I avoid while taking sotalol?
Avoid taking an antacid within 2 hours before or 2 hours after you take sotalol. Some antacids can make it harder for your body to absorb sotalol.
What other drugs will affect sotalol?
Tell your doctor about all your other medicines, especially:
- antacids
- albuterol or terbutaline
- clonidine
- other heart medications, particularly those that affect your heartbeat or lower your blood pressure
- blood pressure medication or
- digoxin
- insulin or other oral diabetes medicines.
This list is not complete. Other drugs may affect sotalol, including prescription and over-the-counter medicines, vitamins, and herbal products. Not all possible drug interactions are listed here.
Storage
Store at room temperature away from moisture and heat.
Keep out of reach of children.
Ingredients
Depends on the manufacturer. An example given is for sotalol USP labeled by Rebel Distributors Corp.
Active: sotalol hydrochloride 80 mg, 120 mg, 160 mg, or 240 mg
Inactive: colloidal silicon dioxide, FD&C blue No. 1 aluminum lake, hydroxypropyl cellulose, lactose anhydrous, lactose monohydrate, magnesium stearate, pregelatinized starch, and sodium starch glycolate.
Popular FAQ
What's the difference between Sotalol and Sotalol AF?
Sotalol AF is specifically used for maintenance of normal sinus rhythm [delay in time to recurrence of atrial fibrillation/atrial flutter (AFIB/AFL)] in patients with symptomatic AFIB/AFL who are currently in sinus rhythm. Plain Sotalol is not approved for AFIB/AFL indication and should not be substituted for Sotalol AF because only Sotalol AF is distributed with a patient package insert that is appropriate for patients with AFIB/AFL. Continue reading
References
More about sotalol
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (56)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Support group
- Drug class: group III antiarrhythmics
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.