EEMT Disease Interactions
There are 24 disease interactions with EEMT (esterified estrogens / methyltestosterone).
- Carcinoma (male)
- Fluid retention
- Hypercalcemia in breast cancer
- Hyperlipoproteinemia
- Liver disease
- Polycythemia
- Suppression of clotting factors
- Abnormal vaginal bleeding
- Carcinomas (estrogenic)
- Hypercalcemia in breast cancer
- Hypertension
- Thromboembolism/cardiovascular
- Hepatic neoplasms
- Diabetes
- Hypercalcemia
- Angioedema
- Gallbladder disease
- Hyperlipidemia
- Hypoparathyroidism
- Liver disease
- Fluid retention
- Glucose intolerance
- Thyroid function tests
- Thyroid function tests
Androgens (applies to EEMT) carcinoma (male)
Major Potential Hazard, High plausibility. Applicable conditions: Prostate Cancer, Breast Cancer -- Male, Benign Prostatic Hyperplasia
The use of androgenic anabolic steroids is contraindicated for male patients with carcinoma of the breast or prostate. Circulating androgens can be converted in peripheral tissues to estrogens and dihydrotestosterone, which may act as promoters of tumor growth in the breast and prostate, respectively. Likewise, androgenic agents may cause enlargement of the prostate and should be used cautiously in patients with or predisposed to prostatic hypertrophy.
Androgens (applies to EEMT) fluid retention
Major Potential Hazard, High plausibility. Applicable conditions: Liver Disease, Congestive Heart Failure, Renal Dysfunction
Androgenic anabolic steroids may cause sodium and water retention, particularly when given in high dosages or for prolonged periods. Therapy with these agents should be administered cautiously in patients who have preexisting problems with fluid overload or are at risk for developing edema. The manufacturers consider the use of androgenic agents to be contraindicated in patients with severe cardiac, renal and/or hepatic dysfunction.
Androgens (applies to EEMT) hypercalcemia in breast cancer
Major Potential Hazard, Moderate plausibility.
When treated with androgenic anabolic steroids, patients with metastatic breast cancer may develop hypercalcemia due to osteolysis. Frequent determination of urine and serum calcium levels is recommended during therapy with androgenic agents. If hypercalcemia occurs, therapy should be stopped. The development of hypercalcemia may indicate progression of metastases to the bone.
Androgens (applies to EEMT) hyperlipoproteinemia
Major Potential Hazard, Moderate plausibility. Applicable conditions: Ischemic Heart Disease, Hyperlipidemia
Androgenic anabolic steroids may adversely affect serum lipids, including lowering HDL and elevating LDL levels. These changes can be marked, particularly with the 17-alpha-alkyl derivatives (i.e., fluoxymesterone, methyltestosterone, oxandrolone, oxymetholone, and stanozolol), and may significantly impact the risk of atherosclerosis and coronary artery disease. Patients with preexisting hyperlipoproteinemia may require closer monitoring during therapy with androgenic agents, and adjustments made accordingly in their lipid-lowering regimen. Androgen therapy should be administered cautiously in patients with coronary artery disease or a history of ischemic heart disease.
Androgens (applies to EEMT) liver disease
Major Potential Hazard, Moderate plausibility.
The use of androgenic anabolic steroids may be associated with development of cholestatic hepatitis and jaundice. Other, more serious hepatotoxicities such as peliosis hepatis and hepatocellular neoplasms are rare but may occur with prolonged use or high dosages. These latter toxicities may be fatal and often not recognized until they become life-threatening. Patients with preexisting liver diseases should be monitored more closely during therapy with anabolic steroids if they are used. If liver function declines or toxicity occurs, therapy should be withdrawn and the cause investigated.
Androgens (applies to EEMT) polycythemia
Major Potential Hazard, Moderate plausibility.
Androgenic anabolic steroids may cause polycythemia when given in high dosages or for prolonged periods. Patients with preexisting polycythemia may experience worsening of their condition. Frequent monitoring of clinical status and hemoglobin and hematocrit levels is recommended if androgen therapy is administered to these patients.
Androgens (applies to EEMT) suppression of clotting factors
Major Potential Hazard, Moderate plausibility. Applicable conditions: Bleeding
Androgenic anabolic steroids may cause suppression of clotting factors II, V, VII, and X, and an increase in prothrombin time. Androgen therapy should be administered cautiously in patients with bleeding disorders.
Estrogens (applies to EEMT) abnormal vaginal bleeding
Major Potential Hazard, High plausibility. Applicable conditions: Abnormal Uterine Bleeding
The use of estrogens is contraindicated in patients with undiagnosed, abnormal vaginal bleeding. Prolonged (> 1 year), unopposed estrogen use (i.e. estrogen without concomitant progestin therapy) has been associated with a significant, dose-related risk of endometrial carcinoma. The risk may be offset substantially by the addition of a progestin but may not be completely abolished. Prior to initiating estrogen therapy, appropriate diagnostic tests should be performed in patients with abnormal vaginal bleeding to rule out endometrial malignancy. The same applies if recurrent or persistent bleeding develops during estrogen therapy.
Estrogens (applies to EEMT) carcinomas (estrogenic)
Major Potential Hazard, High plausibility. Applicable conditions: Neoplasia -- Estrogen Dependent
The use of estrogens is generally contraindicated in patients with known or suspected estrogen-dependent neoplasia such as breast and endometrial cancer, since it may stimulate tumor proliferation. High dosages of estrogens may be used for the palliative treatment of inoperable, metastatic breast cancer, but only in appropriately selected men and postmenopausal women.
Estrogens (applies to EEMT) hypercalcemia in breast cancer
Major Potential Hazard, Moderate plausibility.
When treated with an estrogen, patients with breast cancer and bone metastases may develop severe hypercalcemia, in which case the drug should be stopped and measures be taken to reduce serum calcium levels.
Estrogens (applies to EEMT) hypertension
Major Potential Hazard, High plausibility.
The risk of myocardial infarction and strokes, including those associated with oral contraceptive use and some estrogen use, is increased in patients with hypertension. Moreover, estrogens (and progestogens) may elevate blood pressure and worsen the hypertension, thus compounding the risk. Clinically significant blood pressure increases have been reported during estrogen therapy, particularly in patients receiving high dosages or treated with oral contraceptive combinations having high progestational activity. These effects also increase with duration of therapy and patient age. Therapy with estrogens should be administered cautiously in patients with preexisting hypertension. Some estrogen-based therapies, such as combined hormonal contraceptives, may be contraindicated in patients with uncontrolled hypertension or hypertension with vascular disease. Patients should be monitored for changes in cardiovascular status, and their antihypertensive regimen adjusted or estrogen therapy withdrawn as necessary. In patients requiring contraception, alternative methods should be considered for those who are hypertensive, over age 35, and smoke.
Estrogens (applies to EEMT) thromboembolism/cardiovascular
Major Potential Hazard, High plausibility. Applicable conditions: Thrombotic/Thromboembolic Disorder, History - Thrombotic/Thromboembolic Disorder, Cerebral Vascular Disorder, Ischemic Heart Disease, Migraine
The use of estrogens is considered by manufacturers and some authorities to be contraindicated in patients with active thrombotic, thromboembolic, or thrombophilic disorders. The use of estrogen-containing oral contraceptives is additionally deemed contraindicated in patients with a history of such disorders and/or current cerebrovascular or coronary artery disease. Females with a history of migraines with aura are at an increased risk for stroke and this stroke risk may be further increased in females who have migraines with aura with use of combination oral contraceptives. Hypercoagulability and changes in various clotting factors and blood components have been observed in women receiving estrogen therapy. Known preexisting risk factors for increased thromboembolic or cardiovascular events include smoking, especially over age of 35; hypertension; hyperlipidemia; obesity; diabetes; age over 40; and lupus. Therapy with estrogens should be administered cautiously in the lowest effective dosage and only after careful consideration of risks and benefits. Estrogens should be avoided in patients with a history of thrombotic and thromboembolic disorders associated with estrogen use, except when used in the treatment of metastatic breast or prostatic malignancy.
Estrogens/progestogens (applies to EEMT) hepatic neoplasms
Major Potential Hazard, High plausibility. Applicable conditions: Hepatic Tumor
The use of oral contraceptives is contraindicated in patients with liver tumors. An increased risk of benign hepatic adenomas and hepatocellular carcinomas has been associated with long-term, oral estrogen- progestin contraceptive use of at least 4 years and 8 years, respectively. Although these tumors are rare and have not been reported with other types of estrogen or progestogen therapies, any preparation containing estrogens and/or progestogens should probably be avoided in patients with existing tumors of the liver. Hepatic hemangiomas and nodular hyperplasia of the liver have been reported with isolated estrogen therapy.
Androgens (applies to EEMT) diabetes
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Diabetes Mellitus
The metabolic effects of androgenic anabolic steroids may lower blood glucose. Decreased glucose tolerance and increased insulin resistance have also been reported. Patients with diabetes mellitus should be monitored more closely during therapy with androgenic agents, and their antidiabetic regimen adjusted accordingly.
Androgens (applies to EEMT) hypercalcemia
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Hyperparathyroidism, Renal Dysfunction
Androgenic anabolic steroids decrease urinary excretion of calcium, which may result in hypercalcemia. Therapy with androgenic agents should be administered cautiously in patients with hypercalcemia, disorders of bone metabolism such as hyperparathyroidism, or renal dysfunction. Some manufacturers consider the use of androgenic anabolic steroids to be contraindicated in patients with hypercalcemia.
Estrogens (applies to EEMT) angioedema
Moderate Potential Hazard, Moderate plausibility.
The use of exogenous estrogens may induce or exacerbate symptoms of angioedema, particularly in women with hereditary angioedema. Close monitoring is recommended when prescribing these agents to patients predisposed to angioedema.
Estrogens (applies to EEMT) gallbladder disease
Moderate Potential Hazard, Moderate plausibility.
A two- to four-fold increase in risk of gallbladder disease has been noted in women receiving postmenopausal estrogen therapy. The risk for gallbladder disease may be less for premenopausal women using oral contraceptives containing low-dose estrogens and/or progestins. Therapy with estrogens should be administered cautiously in patients with preexisting gallbladder disease or a history of pregnancy-related cholestasis.
Estrogens (applies to EEMT) hyperlipidemia
Moderate Potential Hazard, Moderate plausibility.
Estrogens may cause adverse lipid changes. Use of estrogens has been associated with elevations in triglyceride levels, particularly in women with pre-existing hypertriglyceridemia. Discontinue therapy if elevated triglycerides lead to pancreatitis. Manage hypercholesterolemia appropriately as indicated.
Estrogens (applies to EEMT) hypoparathyroidism
Moderate Potential Hazard, Moderate plausibility.
Estrogens should be used with caution in individuals with severe hypocalcemia or hypoparathyroidism. Estrogen-induced hypocalcemia may occur in patients with hypoparathyroidism; consider whether the benefits of estrogen therapy outweigh the risks.
Estrogens (applies to EEMT) liver disease
Moderate Potential Hazard, High plausibility.
Estrogens are primarily metabolized by the liver. Use of estrogen therapy is contraindicated in patients with liver dysfunction or disease. Patients with impaired hepatic function may be at increased risk for adverse effects associated with estrogen administration due to decreased drug clearance. Patients with hepatic hemangiomas are at increased risk of exacerbation with use of estrogens. Therapy with estrogens should be administered cautiously in patients with cholestatic jaundice associated with past estrogen use or with pregnancy. In addition, clinicians should be aware that estrogen therapy may affect liver function tests.
Estrogens/progestogens (applies to EEMT) fluid retention
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Congestive Heart Failure, Asthma, Seizures, Renal Dysfunction, Migraine
Estrogens and progestogens may cause fluid retention, particularly when given in high dosages or for prolonged periods. Therapy with these agents should be administered cautiously in patients who have preexisting problems with excess fluid. In addition, patients with conditions that may be adversely affected by fluid accumulation, such as asthma, epilepsy, migraine, and cardiovascular or renal dysfunction, should be observed for exacerbation of their condition during estrogen and/or progestogen therapy.
Estrogens/progestogens (applies to EEMT) glucose intolerance
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Diabetes Mellitus
Impaired glucose tolerance has been observed in some patients administered oral contraceptives and appears to be related primarily to the estrogen dose. However, progestogens can increase insulin secretion and produce insulin resistance to varying degrees, depending on the agent. Caution and close monitoring are recommended in patients with diabetes mellitus during therapy with estrogens and/or progestogens, and adjustments made accordingly in their antidiabetic regimen.
Estrogens/progestogens (applies to EEMT) thyroid function tests
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Thyroid Disease
When administering estrogen and/or progestogen therapy in patients with thyroid disorders, clinicians should be aware that these hormones may affect thyroid function tests. Changes have mostly been reported with the use of combination oral contraceptives. Specifically, thyroid-binding globulin (TBG) may be increased, resulting in elevated circulating total thyroid hormone, as measured by PBI (protein-bound iodine), T4 by column or radioimmunoassay, or T3 by radioimmunoassay. Free T3 resin uptake may be decreased. On the contrary, a decrease in TBG and, consequently, thyroxine concentration, has been reported by the manufacturers of the progestin-only (norethindrone) oral contraceptives. Patients on thyroid replacement therapy may require higher doses of thyroid hormone and appropriate monitoring.
Androgens (applies to EEMT) thyroid function tests
Minor Potential Hazard, Moderate plausibility. Applicable conditions: Hyperthyroidism, Hypothyroidism
When androgenic anabolic steroids are used in patients with thyroid disorders, clinicians should be aware that these agents may affect thyroid function tests. Specifically, thyroid-binding globulin levels may be decreased, resulting in lower total T4 serum levels and increased resin uptake of T3 and T4. Free thyroid hormone levels remain unchanged, however.
Switch to professional interaction data
EEMT drug interactions
There are 275 drug interactions with EEMT (esterified estrogens / methyltestosterone).
EEMT alcohol/food interactions
There are 4 alcohol/food interactions with EEMT (esterified estrogens / methyltestosterone).
More about EEMT (esterified estrogens / methyltestosterone)
- EEMT consumer information
- Check interactions
- Compare alternatives
- Reviews (1)
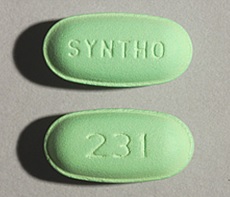
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: sex hormone combinations
- En español
Related treatment guides
Drug Interaction Classification
| Highly clinically significant. Avoid combinations; the risk of the interaction outweighs the benefit. | |
| Moderately clinically significant. Usually avoid combinations; use it only under special circumstances. | |
| Minimally clinically significant. Minimize risk; assess risk and consider an alternative drug, take steps to circumvent the interaction risk and/or institute a monitoring plan. | |
| No interaction information available. |
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.