Vertebral Compression Fracture
Medically reviewed by Drugs.com. Last updated on Jun 30, 2025.
What is a vertebral compression fracture?
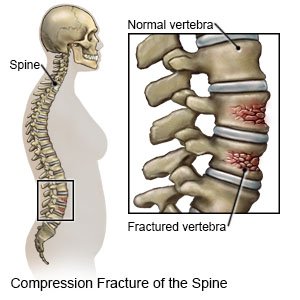
A vertebral compression fracture (VCF) is a collapse or breakdown in a bone in your spine. Compression fractures happen when there is too much pressure on the vertebra. VCFs most often occur in the thoracic (middle) and lumbar (lower) areas of your spine. Fractures may be mild to severe.
 |
What are the signs and symptoms of a VCF?
You may not have any signs and symptoms with a mild VCF. You may have any of the following with a more severe fracture:
- Sudden, severe, and sharp back pain
- Back pain that gets worse when you stand or walk
- Muscle spasms in your back
- Problems urinating or having bowel movements
- Sudden weakness in your arms or legs
How is a VCF diagnosed?
Your healthcare provider will ask you about injuries and diseases you have had in the past. Your healthcare provider will do a physical exam, and check your spine. You may need any of the following tests:
- X-rays, a CT scan, or MRI of your spine may be taken. You may be given contrast liquid before the pictures are taken to help a fracture show up better in pictures. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid. Do not enter the MRI room with anything metal. Metal can cause serious injury. Tell the provider if you have any metal in or on your body.
- A bone scan may show broken bones or other problems in the spine, such as an infection.
How is a VCF treated?
You may need any of the following, depending on how severe the fracture is:
- Bed rest may be needed for a mild fracture.
- A back brace may be needed for 8 to 12 weeks. A brace may decrease your pain, and help your vertebrae heal.
- A cane or walker can help you keep your balance when you walk. This helps prevent a fall that could cause more injury.
- Medicines may be given for pain. Bisphosphonates and calcitonin are medicines to help your bones get stronger. They can decrease the pain of a VCF caused by osteoporosis, and decrease your risk for another fracture.
- Physical or occupational therapy may be recommended. A physical therapist teaches you exercises to help improve movement and strength, and to decrease pain. An occupational therapist teaches you skills to help with your daily activities.
- Surgery may be needed if your pain, weakness, or numbness does not go away with other treatment. Surgery may make your spine more stable, and help decrease pressure on your spinal nerves caused by the fracture.
Related medications
Voltaren
Voltaren (diclofenac) is used to treat pain or inflammation caused by arthritis or ankylosing ...
Fosamax
Fosamax (alendronate) is used to treat or prevent postmenopausal osteoporosis and steroid-induced ...
Botox
Botox is used for cosmetic purposes and to treat overactive bladder symptoms, urinary incontinence ...
Advil
Advil (ibuprofen) reduces fever, pain and inflammation caused by headaches, toothaches, arthritis ...
Bayer Aspirin
Bayer Aspirin is used for angina, angina pectoris prophylaxis, ankylosing spondylitis ...
Naproxen
Naproxen is a nonsteroidal anti-inflammatory drug used to treat pain or inflammation caused by ...
Diclofenac
Diclofenac is a nonsteroidal anti-inflammatory drug used to treat pain and inflammation associated ...
Aspirin
Aspirin is used to treat mild to moderate pain and to reduce fever or inflammation. Learn about ...
Aleve
Aleve is a nonsteroidal anti-inflammatory drug (NSAID) used to treat pain and inflammation. Learn ...
How can I manage pain while I sleep?
- Do not sleep in a waterbed. Waterbeds do not provide good back support.
- Sleep on a firm mattress. You may also put a ½ to 1-inch piece of plywood between the mattress and box spring.
- Sleep on your back with a pillow under your knees. This will decrease pressure on your back. You may also sleep on your side with 1 or both of your knees bent and a pillow between them. It may also be helpful to sleep on your stomach with a pillow under you at waist level.
Call your local emergency number (911 in the US) if:
- You feel lightheaded, short of breath, and have chest pain.
- You cough up blood.
- You suddenly cannot feel your legs.
- You suddenly have trouble moving your arms or legs.
When should I seek immediate care?
- Your arm or leg feels warm, tender, and painful. It may look swollen and red.
- You have new problems urinating or having bowel movements.
- You have severe pain in your back after falling, bending forward, sneezing, or coughing strongly.
When should I call my doctor?
- You cannot sleep or rest because of back pain.
- You have pain or swelling in your back that is getting worse, or does not go away.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Vertebral Compression Fracture
Treatment options
Care guides
Symptoms and treatments
Medicine.com guides (external)
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
