Ulcerative Colitis
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What is ulcerative colitis?
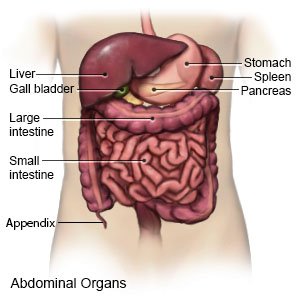
Ulcerative colitis is a chronic disease of the colon (large intestine). Inflammation and ulcers form on the inner lining of your colon. Ulcerative colitis is a type of inflammatory bowel disease.
 |
What increases my risk for ulcerative colitis?
The cause of ulcerative colitis is not known. Any of the following may increase your risk:
- Age 20 to 40 years
- A family history of ulcerative colitis
- A food allergy
- An autoimmune disorder such as rheumatoid arthritis, hemolytic anemia, and uveitis
- A bacterial infection
What are the signs and symptoms of ulcerative colitis?
Signs and symptoms of ulcerative colitis may come and go. Your symptoms may get worse at times (flare). You may have times when signs and symptoms decrease or disappear on their own or with treatment (remission). Medicines such as NSAIDs, certain foods, or emotional stress may trigger a flare. You may have any of the following:
- Blood or mucus in your bowel movements
- Bleeding from your rectum
- Feeling like you need to have a bowel movement after you just had one
- Nausea, vomiting, or diarrhea
- Abdominal tenderness and bloating
- Fever, loss of appetite, or weight loss without trying
- Feeling more mentally and physically tired than usual (fatigue)
How is ulcerative colitis diagnosed?
Your healthcare provider will ask about your symptoms and when they started. Your provider will ask what triggers your symptoms, and how long they last. You may need any of the following tests:
- A digital rectal exam means your provider will put a gloved finger inside your rectum. This may help show inflammation or blood.
- Blood tests may be used to show an infection, dehydration, or anemia (low red blood cell levels).
- A bowel movement sample may be tested for blood or infection.
- A barium enema is an x-ray of the colon. A tube is put into your anus, and a liquid called barium is put through the tube. Barium is used so that your healthcare provider can see your colon better.
- CT or MRI pictures may be used to find problems in your intestines. You may be given contrast liquid to help your colon show up better in the pictures. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid. Do not enter the MRI room with anything metal. The MRI machine uses a powerful magnet. Metal can cause serious injury from the magnet. Tell the healthcare provider if you have any metal in or on your body.
- An endoscopy is a procedure used to look for inflammation, bleeding, or ulcers in your intestines. An endoscope is a thin, flexible tube with a light and camera on the end. A tissue or bowel sample may be taken from your colon to be tested.
Related medications
How is ulcerative colitis treated?
- Medicines may be given to help decrease inflammation or control your immune system. You may need to take more than 1 medicine to treat your ulcerative colitis.
- Surgery may be needed to remove part or all of your colon. Ask about the different kinds of surgery that can be done to help your symptoms.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
How can I manage my ulcerative colitis?
- Keep a record of everything you eat and drink. Include any symptoms the food or drink causes or makes worse. You may need to avoid certain foods. Dairy, alcohol, hot spices, and high-fiber foods are examples of foods that may worsen your symptoms. Your provider may recommend that you take vitamins or mineral supplements. Always ask your provider before you take vitamins or nutritional supplements.
- Do not take NSAID medicines. NSAIDs such as aspirin and ibuprofen can cause a flare.
- Take your medicines exactly as directed. This may help to keep your disease in remission.
- Drink liquids as directed. Ask how much liquid to drink each day and which liquids are best for you. Do not drink alcohol. This can make your symptoms worse.
- Be physically active. Physical activity, such as exercise, can help prevent constipation and keep your colon healthy. Ask your provider about the best exercise plan for you.
- Manage stress. Stress may trigger your symptoms. Learn ways to relax, such as deep breathing or meditation.
Call your local emergency number (911 in the US) if:
- You have sudden trouble breathing.
- You have a fast heart rate, fast breathing, or are too dizzy to stand.
When should I seek immediate care?
- You have severe abdominal pain.
- You vomit blood, or your vomit looks like coffee grounds.
- You have tar-colored bowel movements or you see blood in your bowel movements.
When should I call my doctor?
- You have a fever, chills, a cough, or feel weak and achy.
- Your abdominal pain does not go away, even after treatment.
- Your abdomen is swollen.
- You lose weight without trying.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Ulcerative Colitis
Treatment options
Care guides
Symptoms and treatments
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
