Pain Management
Medically reviewed by Drugs.com. Last updated on Apr 6, 2025.
What is pain management?
Pain management includes medicines and therapies to treat pain from a surgery, injury, or illness. Pain can cause changes in your physical and emotional health, such as depression and sleep problems. Pain management may help you rest, heal, and return to your daily activities. Pain management can also help increase your appetite, sleep, and energy, and improve your mood and relationships.
What are the types of pain?
- Acute pain starts suddenly and lasts a short time. The pain usually goes away as your body heals, but may become chronic if it is not treated.
- Chronic pain lasts a long time or grows worse. It may last for months or years due to a chronic condition. It may be pain that remains after you have recovered from an injury or illness.
How is the cause of pain diagnosed?
Your healthcare provider will examine you and look for painful areas. Your provider may touch or press different places on your body and ask about your pain. Your provider may ask you to describe your pain. Tell your provider if your pain is sharp, dull, or achy. Tell your provider if you have constant pain or if it comes and goes. You may also need any of the following to check how much pain you have or to find its cause:
- A pain diary may help to find the cause of your pain. The diary can help you track pain cycles. Include when the pain started, how long it lasted, and how strong it was. Also include anything that made the pain worse or better.
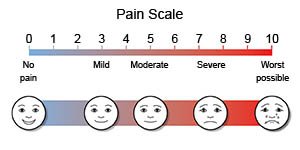
- Pain scales may help measure how much pain you feel. Pain scales may include numbers or faces. Your provider may ask you to rate the pain on a scale from 0 to 10.
- An x-ray, CT, or MRI may be used to find the cause of your pain. You may be given contrast liquid to help the pictures show up better. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid. Do not enter the MRI room with anything metal. Metal can cause serious injury. Tell the healthcare provider if you have any metal in or on your body.
- Stimulation tests may help find nerves or muscles affected by pain.
Which over-the-counter medicines may be used for pain?
- NSAIDs , such as ibuprofen, help decrease swelling, pain, and fever. This medicine is available with or without a doctor's order. NSAIDs can cause stomach bleeding or kidney problems in certain people. If you take blood thinner medicine, always ask if NSAIDs are safe for you. Always read the medicine label and follow directions. Do not give these medicines to children younger than 6 months without direction from a healthcare provider.
- Acetaminophen decreases pain and fever. It is available without a doctor's order. Ask how much to take and how often to take it. Follow directions. Read the labels of all other medicines you are using to see if they also contain acetaminophen, or ask your doctor or pharmacist. Acetaminophen can cause liver damage if not taken correctly.
- A pain cream, gel, or patch may be applied to your skin on painful areas.
Drugs used to treat this and similar conditions
Hydrocodone
Hydrocodone (Hysingla ER and Zohydro ER) is used for around-the-clock treatment of severe pain ...
Cymbalta
Cymbalta (duloxetine) is used to treat major depressive disorder, general anxiety disorder and ...
Benlysta
Benlysta infusion is used to treat active systemic lupus erythematosus (SLE) and active lupus ...
Oxycodone
Oxycodone is an opioid analgesic used to treat moderate to severe pain; it has a high potential for ...
Tylenol
Tylenol is a pain reliever and a fever reducer used to treat many conditions such as headaches ...
Acetaminophen
Acetaminophen is a widely used pain reliever and fever reducer for conditions like headaches ...
Ibuprofen
Ibuprofen (Advil, Motrin) treats minor aches and pains caused by the common cold, headaches ...
Gabapentin
Gabapentin is an anti-epileptic drug, also called an anticonvulsant. It is used to treat some types ...
Acetaminophen/hydrocodone
The combination of hydrocodone and acetaminophen is used to relieve moderate to severe pain ...
Which prescription medicines may be used for pain?
- Prescription pain medicines such as opioids, or narcotics, are only used for short-term (acute) pain. Your healthcare provider will tell you how to take your specific prescription pain medicine safely. Your provider will tell you about common and serious side effects of the medicine and what to do if they happen. Some prescription pain medicines contain acetaminophen. Do not take other medicines that contain acetaminophen without talking to your provider. Too much acetaminophen may cause liver damage.
- Muscle relaxers help decrease pain and muscle spasms.
- Steroids decrease inflammation that causes pain.
- Anesthetic medicines may be injected in or around a nerve to block pain signals from the nerves.
- Anxiety medicine decreases anxiety. High levels of anxiety make pain harder to manage.
- Antidepressants may be used to help decrease or prevent the symptoms of depression or anxiety. They are also used to treat nerve pain.
- Anticonvulsants are usually used to control seizures. They may also be used to decrease chronic pain.
What do I need to know about prescription pain medicine safety?
Your healthcare provider will give you specific instructions based on the medicine you are taking. Instructions will include how to dispose of medicine you did not use. The following are general guidelines:
- Take your medicine as directed. Take only the amount prescribed or recommended. If you use a pain patch, remove the old patch before you place a new one. Ask your provider before you stop taking prescription pain medicine you have been taking for longer than 2 weeks. A sudden stop may cause serious health problems.
- Follow safety guidelines. Some medicines can cause drowsiness, slowed breathing, or concentration problems. Do not drink alcohol, drive, or operate heavy machines while you use prescription medicines. Take pain medicine 30 minutes before exercise or physical therapy, or as directed.
- Manage side effects. Some food, alcohol, and other medicines may cause side effects when combined with pain medicine. Your provider will tell you what to do if you have any side effects.
What can I do to manage my pain without medicine?
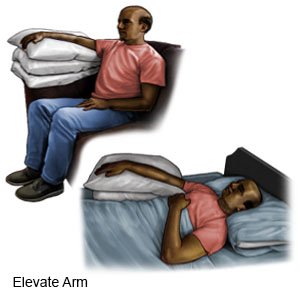
- Rest as often as needed. Rest helps your body heal. Sleep in a comfortable position. Examples include sleeping upright or on your side. Use pillows to support painful areas. Tell your healthcare provider if pain is keeping you from sleeping well.
- Apply heat or ice as directed. For heat, use a heat pack, heating pad set on low, or a warm washcloth. Apply heat for 20 to 30 minutes every 2 hours for as many days as directed. For ice, use an ice pack, or put crushed ice in a plastic bag. Cover the bag with a towel before you place it on your skin. Apply ice for 15 to 20 minutes every hour or as directed.
- Elevate the painful area above the level of your heart, if possible. This will help decrease swelling and pain. Prop your painful area on pillows or blankets to keep it elevated comfortably.
- Apply compression with an elastic bandage as directed. Wrap an elastic bandage around the area. Do not wrap the bandage tightly. You should be able to put 2 fingers between the bandage and your skin.

- Talk to your provider about your daily activities. Some activities may cause or worsen pain. Your provider can help you find ways to reduce pain. For example, you may need to change when you take your pain medicine so it is more effective during activities.
- Go to rehabilitation (rehab) as directed. Rehab may include physical or occupational therapy. A physical therapist teaches you exercises to help improve movement and strength, and to decrease pain. An occupational therapist teaches you skills to help with your daily activities. Your therapist may recommend assistive devices. For example, a splint, cane, crutches, or walker can remove pressure or provide support. Braces or orthotics help you stand or walk more easily.
- Ask about pain management techniques and devices. Meditation or aromatherapy may help you relax. Biofeedback teaches you to lower your breathing and heart rate when you are in pain. Massage therapy helps relieve tight muscles. Transcutaneous electrical stimulations (TENS) uses mild, safe electrical signals to help control muscle or nerve pain.
- Ask about surgery or other procedures to help relieve pain. Examples include radio waves, thermal (heat), ultrasound, and laser therapy. Surgery may include blocking nerves or repairing joints that are the cause of your chronic pain.
When should I call my doctor or pain specialist?
- You continue to have breakthrough pain (pain between medicine doses).
- The medicine you are taking makes you sleepier than usual or confused.
- You have pain even after you take your pain medicine.
- You have a new pain or the pain seems different than before.
- You have constipation from prescription pain medicine that is not helped with treatment.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
