Pemgarda: Package Insert / Prescribing Info
Package insert / product label
Generic name: pemivibart
Dosage form: injection
Drug class: Miscellaneous antivirals
Medically reviewed by Drugs.com. Last updated on Aug 10, 2025.
On This Page
- Indications and Usage
- Dosage and Administration
- Dosage Forms and Strengths
- Contraindications
- Warnings and Precautions
- Adverse Reactions/Side Effects
- Drug Interactions
- Use In Specific Populations
- Overdosage
- Description
- Clinical Pharmacology
- Nonclinical Toxicology
- Clinical Studies
- How Supplied/Storage and Handling
Highlights of Prescribing Information
Recent Major Changes
See 17 for FDA-approved patient labeling.
Revised: 8/2024
Full Prescribing Information
WARNING: ANAPHYLAXIS
- Anaphylaxis has been observed with PEMGARDA in 0.6% (4/623) of participants in a clinical trial.
- Anaphylaxis was reported during the first and second infusion of PEMGARDA [see Warnings and Precautions (5.1), Adverse Reactions (6.1)].
- Anaphylaxis can be life-threatening.
- Prior to administering PEMGARDA, consider the potential benefit of COVID-19 prevention along with the risk of anaphylaxis [see Warnings and Precautions (5.1), Adverse Reactions (6.1 ), and Clinical Studies (14)].
- Administer PEMGARDA only in settings in which healthcare providers have immediate access to medications to treat anaphylaxis and the ability to activate the emergency medical system (EMS), as necessary.
- Clinically monitor individuals during the infusion and for at least two hours after completion of the infusion.
- Discontinue PEMGARDA immediately if signs or symptoms of anaphylaxis or any severe systemic reaction are observed and initiate appropriate medications and/or supportive therapy.
FACT SHEET FOR HEALTHCARE PROVIDERS: EMERGENCY USE AUTHORIZATION OF PEMGARDA (PEMIVIBART)
HIGHLIGHTS OF EMERGENCY USE AUTHORIZATION (EUA)
These highlights of the EUA do not include all the information needed to use PEMGARDA under the EUA. See the FULL FACT SHEET FOR HEALTHCARE PROVIDERS for PEMGARDA.
PEMGARDA (pemivibart) injection, for intravenous use
Original EUA Authorized Date:03/2024
|
WARNING: ANAPHYLAXIS See Full Fact Sheet for Healthcare Providers for the complete boxed warning.
|
---------------------------- RECENT MAJOR CHANGES--------------------------
Microbiology (12.4): Updated pseudotyped virus-like particle
neutralization data 08/2024
--------------------------- EUA FOR PEMGARDA------------------------------------
The U.S. FDA has issued an EUA for the emergency use of the unapproved product PEMGARDA (pemivibart), a SARS-CoV-2 spike protein-directed attachment inhibitor, for the pre-exposure prophylaxis of coronavirus disease 2019 (COVID-19) in adults and adolescents (12 years of age and older weighing at least 40 kg):
- who are not currently infected with SARS-CoV-2 and who have not had a known recent exposure to an individual infected with SARS‑CoV-2 and:
- who have moderate-to-severe immune compromise due to a medical condition or receipt of immunosuppressive medications or treatments and are unlikely to mount an adequate immune response to COVID-19 vaccination.
PEMGARDA has been authorized by FDA for the emergency use described above. PEMGARDA is not FDA-approved for any use, including use for pre-exposure prophylaxis of COVID-19. ( 1)
LIMITATIONS OF AUTHORIZED USE
- PEMGARDA is not authorized for use:
-For treatment of COVID-19, or:
-For post-exposure prophylaxis of COVID-19 in individuals who have been exposed to someone infected with SARS‑CoV-2.
- PEMGARDA is authorized for use only when the combined national frequency of variants with substantially reduced susceptibility is less than or equal to 90%, based on available information including variant susceptibility to PEMGARDA and national variant frequencies.
- Pre-exposure prophylaxis with PEMGARDA is not a substitute for vaccination in individuals for whom COVID-19 vaccination is recommended. Individuals for whom COVID-19 vaccination is recommended, including individuals with moderate-to-severe immune compromise who may derive benefit from COVID-19 vaccination, should receive COVID-19 vaccination.
- In individuals who have recently received a COVID-19 vaccine, PEMGARDA should be administered at least 2 weeks after vaccination.
- PEMGARDA may only be prescribed for an individual patient by physicians, advanced practice registered nurses, and physician assistants who are licensed or authorized under State law to prescribe drugs.
- PEMGARDA is authorized only for the duration of the declaration that circumstances exist justifying the authorization of the emergency use of PEMGARDA under section 564(b)(1) of the Act, 21 U.S.C. § 360bbb 3(b)(1), unless the authorization is terminated or revoked sooner.
See Full Fact Sheet for Healthcare Providers for examples of medical conditions or treatments that may result in moderate to severe immune compromise and an inadequate immune response to COVID-19 vaccination, the justification for emergency use of drugs during the COVID-19 pandemic, information on available alternatives, and additional information on COVID‑19.
------------------------- DOSAGE AND ADMINISTRATION-----------------------
PEMGARDA must be infused over a minimum of 60 minutes. ( 2.1) The dosage of PEMGARDA for emergency use in adults and adolescents (12 years of age and older weighing at least 40 kg) is:
Initial Dose: 4500 mg administered as a single intravenous infusion. ( 2.1)
Repeat Dose: 4500 mg administered as a single intravenous infusion approximately every 3 months. Repeat dosing should be timed from the date of the most recent PEMGARDA dose. ( 2.1)
See Full Fact Sheet for Healthcare Providers for details on preparation and administration. ( 2.3)
--------------------- DOSAGE FORMS AND STRENGTHS------------------------
Injection: PEMGARDA 500 mg/4 mL (125 mg/mL) in a single-dose vial. ( 3)
-------------------------- CONTRAINDICATIONS------------------------------------
PEMGARDA is contraindicated in individuals with previous severe hypersensitivity reactions, including anaphylaxis, to any component of PEMGARDA. ( 4)
----------------------- WARNINGS AND PRECAUTIONS--------------------------
- Anaphylaxis:Anaphylaxis has been observed with PEMGARDA in 4 of 623 (0.6%) participants in a clinical trial. Administer PEMGARDA only in settings in which healthcare providers have immediate access to medications to treat anaphylaxis and the ability to activate the emergency medical system (EMS), as necessary. If signs or symptoms of an anaphylactic reaction occur, immediately discontinue administration, and initiate appropriate medications and/or supportive therapy. Discontinue PEMGARDA use permanently in individuals who experience signs or symptoms of anaphylaxis. ( 5.1)
- Hypersensitivity and Infusion-Related Reactions: Hypersensitivity and infusion-related reactions occurring during the infusion and up to 24 hours after the infusion have been observed with PEMGARDA and may be severe or life-threatening. If signs or symptoms of a clinically significant hypersensitivity reaction or infusion-related reaction occur, immediately discontinue administration, and initiate appropriate medications and/or supportive therapy. Clinically monitor individuals during infusion and for at least 2 hours after infusion is complete. ( 5.2)
- Risk of Cross-Hypersensitivity with COVID-19 Vaccines:PEMGARDA contains polysorbate 80, which is in some COVID‑19 vaccines and is structurally similar to polyethylene glycol (PEG), an ingredient in other COVID-19 vaccines. For individuals with a history of severe hypersensitivity reaction to a COVID-19 vaccine, consider consultation with an allergist-immunologist prior to PEMGARDA administration. ( 5.3)
- Risk for COVID-19 Due to SARS-CoV-2 Viral Variants with Substantially Reduced Susceptibility to PEMGARDA: Certain SARS-CoV-2 viral variants may have substantially reduced susceptibility to PEMGARDA. PEMGARDA may not be effective at preventing COVID-19 caused by these SARS-CoV-2 viral variants. Inform individuals of the increased risk, compared to other variants, for COVID-19 due to SARS-CoV-2 viral variants that exhibit significantly reduced susceptibility to PEMGARDA. If signs and symptoms of COVID-19 occur, advise individuals to test for COVID-19 and seek medical attention, including starting treatment for COVID-19 as appropriate. ( 5.4)
---------------------------------ADVERSE REACTIONS------------------------------
The most common adverse events (all grades, incidence ≥2%) observed in participants who have moderate-to-severe immune compromise treated with PEMGARDA included systemic and local infusion-related or hypersensitivity reactions, upper respiratory tract infection, viral infection, influenza-like illness, fatigue, headache, and nausea.
You or your designee must report all SERIOUS ADVERSE EVENTS or MEDICATION ERRORS potentially related to PEMGARDA (1) by submitting FDA Form 3500 online,(2) by downloading this form, and then submitting it by mail or fax, or (3) by contacting the FDA at 1-800-FDA-1088 to request this form. Please also provide a copy of this form to Invivyd, Inc. by email at: pv@invivyd.com or call 1-800-890-3385 to report adverse events. (6.4)
See PATIENT AND PARENTS/CAREGIVER FACT SHEET
TABLE OF CONTENTS*
1 EMERGENCY USE AUTHORIZATION FOR PEMGARDA
2 DOSAGE AND ADMINISTRATION
2.1 Dosage for Emergency Use of PEMGARDA
2.2 Dosage Adjustment in Specific Populations
2.3 Dose Preparation and Administration
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Anaphylaxis
5.2 Hypersensitivity and Infusion-Related Reactions
5.3 Risk of Cross-Hypersensitivity with COVID-19 Vaccines
5.4 Risk for COVID-19 Due to SARS-CoV-2 Viral Variants with Substantially Reduced Susceptibility to PEMGARDA
6 ADVERSE REACTIONS
6.1 Adverse Reactions from Clinical Studies
6.4 Required Reporting for Serious Adverse Events and Medication Errors
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
12.4 Microbiology
12.6 Immunogenicity
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
13.2 Animal Toxicology and/or Pharmacology
14 CLINICAL STUDIES
14.1 Overview of Immunobridging Approach
14.2 Pre-exposure Prophylaxis of COVID-19 (VYD222-PREV-001 [CANOPY])
14.3 Overall Benefit-Risk Assessment and Limitations of Data Supporting the Benefits of the Product
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
18 MANUFACTURER INFORMATION
*Sections or subsections omitted from the full prescribing information are not listed
1. Indications and Usage for Pemgarda
The U.S. Food and Drug Administration (FDA) has issued an Emergency Use Authorization (EUA) for the emergency use of the unapproved product PEMGARDA (pemivibart) for the pre-exposure prophylaxis of coronavirus disease 2019 (COVID-19) in adults and adolescents (12 years of age and older weighing at least 40 kg):
- Who are not currently infected with SARS-CoV-2 and who have not had a known recent exposure to an individual infected with SARS-CoV-2 and
- Who have moderate-to-severe immune compromise due to a medical condition or receipt of immunosuppressive medications or treatments and are unlikely to mount an adequate response to COVID-19 vaccination.
Medical conditions or treatments that may result in moderate to severe immune compromise and an inadequate immune response to COVID-19 vaccination include:
- Active treatment for solid tumor and hematologic malignancies
- Hematologic malignancies associated with poor responses to COVID-19 vaccines regardless of current treatment status (e.g., chronic lymphocytic leukemia, non-Hodgkin lymphoma, multiple myeloma, acute leukemia)
- Receipt of solid-organ transplant or an islet transplant and taking immunosuppressive therapy
- Receipt of chimeric antigen receptor (CAR)-T-cell or hematopoietic stem cell transplant (within 2 years of transplantation or taking immunosuppressive therapy)
- Moderate or severe primary immunodeficiency (e.g., common variable immunodeficiency disease, severe combined immunodeficiency, DiGeorge syndrome, Wiskott-Aldrich syndrome)
- Advanced or untreated HIV infection (people with HIV and CD4 cell counts <200/mm 3, history of an AIDS-defining illness without immune reconstitution, or clinical manifestations of symptomatic HIV)
- Active treatment with high-dose corticosteroids (i.e., ≥20 mg prednisone or equivalent per day when administered for ≥2 weeks), alkylating agents, antimetabolites, transplant-related immunosuppressive drugs, cancer chemotherapeutic agents classified as severely immunosuppressive, and biologic agents that are immunosuppressive or immunomodulatory (e.g., B-cell depleting agents)
Limitations of Authorized Use
- PEMGARDA is not authorized for use:
-For treatment of COVID-19, or
-For post-exposure prophylaxis of COVID-19 in individuals who have been exposed to someone infected with SARS-CoV-2.
- PEMGARDA is authorized for use only when the combined national frequency of variants with substantially reduced susceptibility to PEMGARDA is less than or equal to 90%, based on available information including variant susceptibility to PEMGARDA and national variant frequencies 1.
- Pre-exposure prophylaxis with PEMGARDA is not a substitute for vaccination in individuals for whom COVID-19 vaccination is recommended. Individuals for whom COVID-19 vaccination is recommended, including individuals with moderate-to-severe immune compromise who may derive benefit from COVID-19 vaccination, should receive COVID‑19 vaccination.
- In individuals who have recently received a COVID-19 vaccine, PEMGARDA should be administered at least 2 weeks after vaccination.
PEMGARDA may only be prescribed for an individual patient by physicians, advanced practice registered nurses, and physician assistants that are licensed or authorized under State law to prescribe drugs.
PEMGARDA has been authorized by FDA for the emergency use described above. PEMGARDA is not FDA-approved for any use, including use for pre-exposure prophylaxis of COVID-19.
PEMGARDA is authorized only for the duration of the declaration that circumstances exist justifying the authorization of the emergency use of PEMGARDA under section 564(b)(1) of the FD&C Act, 21 U.S.C. § 360bbb-3(b)(1), unless the authorization is terminated or revoked sooner.
Justification for Emergency Use of Drugs During the COVID‑19 Pandemic:
There is currently an outbreak of coronavirus disease 2019 (COVID‑19) caused by SARS‑CoV‑2, a novel coronavirus. The Secretary of the U.S. Department of Health and Human Services (HHS) has:
- Determined that there is a public health emergency, or significant potential for a public health emergency 2.
- Declared that circumstances exist justifying the authorization of emergency use of drugs and biological products for the prevention or treatment of COVID-19 3.
An EUA is an FDA authorization for the emergency use of an unapproved product or unapproved use of an approved product (i.e., drug, biological product, or device) in the United States under certain circumstances including, but not limited to, when the Secretary of HHS declares that there is a public health emergency that affects the national security or the health and security of United States citizens living abroad, and that involves biological agent(s) or a disease or condition that may be attributable to such agent(s). Criteria for issuing an EUA include:
- The biological agent(s) can cause a serious or life-threatening disease or condition.
- Based on the totality of the available scientific evidence (including data from adequate and well controlled clinical trials, if available), it is reasonable to believe that:
- the product may be effective in diagnosing, treating, or preventing the serious or life-threatening disease or condition; and
- the known and potential benefits of the product - when used to diagnose, prevent, or treat such disease or condition - outweigh the known and potential risks of the product, taking into consideration the material threat posed by the biological agent(s).
- There is no adequate, approved, and available alternative to the product for diagnosing, preventing, or treating the serious or life-threatening disease or condition.
Information Regarding Available Alternatives for the EUA Authorized Use
There are no adequate, approved, and available alternatives to PEMGARDA for the pre-exposure prophylaxis of COVID-19 in individuals who are unlikely to mount an adequate immune response to COVID-19 vaccination.
For information on clinical studies of PEMGARDA and other therapies for the pre-exposure prophylaxis of COVID-19, see www.clinicaltrials.gov.
- 1
- FDA will monitor conditions to determine whether use is consistent with the scope of authorization, referring to available information, including information on variant susceptibility (e.g., Section 12.4 of the authorized Fact Sheet for Healthcare Providers) and CDC variant frequency data available at: https://covid.cdc.gov/covid-data-tracker/#variant-proportions.
- 2
- See U.S. Department of Health and Human Services, Determination of a Public Health Emergency and Declaration that Circumstances Exist Justifying Authorizations Pursuant to Section 564(b) of the Federal Food, Drug, and Cosmetic Act, 21 U.S.C. § 360bbb-3. February 4, 2020; https://www.federalregister.gov/documents/2020/02/07/2020-02496/determination-of-public-health-emergency. See also U.S. Department of Health and Human Services, Amended Determination of a Public Health Emergency or Significant Potential for a Public Health Emergency Pursuant to Section 564(b) of the Federal Food, Drug, and Cosmetic Act, 21 U.S.C. § 360bbb-3(b). March 15, 2023 (“Amended Determination”); https://www.federalregister.gov/documents/2023/03/20/2023-05609/covid-19-emergency-use-authorization-declaration.
- 3
- See U.S. Department of Health and Human Services, Declaration that Circumstances Exist Justifying Authorizations Pursuant to Section 564(b) of the Federal Food, Drug, and Cosmetic Act, 21 U.S.C. § 360bbb-3, 85 FR 18250 (April 1, 2020); https://www.federalregister.gov/documents/2020/04/01/2020-06905/emergency-use-authorization-declaration. See also Amended Determination (“The declarations issued pursuant to section 564(b)(1) of the FD&C Act that circumstances exist justifying the authorization of emergency use of certain in vitro diagnostics, personal respiratory protective devices, other medical devices and drugs and biological products, as set forth in those declarations, and that are based on the February 4, 2020 determination, remain in effect until those declarations are terminated in accordance with section 564 of the FD&C Act.”).
2. Pemgarda Dosage and Administration
2.1 Dosage for Emergency Use of PEMGARDA
Initial Dosing:
The initial dosage of PEMGARDA in adults and adolescents (12 years of age and older weighing at least 40 kg) is 4500 mg administered as a single intravenous (IV) infusion [see Clinical Pharmacology (12.3 )].
Repeat Dose:
The repeat dosage is 4500 mg of PEMGARDA administered as a single IV infusion every 3 months. Repeat dosing should be timed from the date of the most recent PEMGARDA dose.
The recommendations for dosing are based on the totality of the scientific evidence including clinical pharmacology data, antiviral activity data, and clinical study data [seeClinical Pharmacology (12.3), Microbiology (12.4 ), and Clinical Studies (14 )].
2.2 Dosage Adjustment in Specific Populations
No dosage adjustment is recommended in pregnant or lactating individuals, in geriatrics, or in individuals with renal or hepatic impairment [seeUse in Specific Populations (8 )].
2.3Dose Preparation and Administration
General Information:
- PEMGARDA should be prepared and administered by a qualified healthcare provider using aseptic technique .
- Vials of PEMGARDA are for one-time use only.
- Visually inspect the vials for particulate matter and discoloration. PEMGARDA is a clear to slightly opalescent, colorless to yellow solution. Discard the vial if the solution is cloudy, discolored, or if visible particles are observed.
- PEMGARDA should be administered as an IV infusion diluted with 0.9% sodium chloride.
Materials Needed:
- 9 single-dose vials of PEMGARDA (125 mg/mL)
- 50 mL prefilled bag of 0.9% sodium chloride (normal saline) for IV injection
- IV extension set with inline 0.2-micron filter
- Infusion pump or gravity infusion set
- 0.9% sodium chloride injection for flushing
Preparation:
- Remove PEMGARDA vials from refrigerated storage and allow to equilibrate to room temperature (18℃ to 26℃ [64℉ to 79℉]) for 10 minutes before preparation. Do not expose to direct heat. Do not shake vials. Inspect the vials.
- Prepare IV bag by removing and discarding 36 mL from a 50 mL prefilled bag of 0.9% sodium chloride for IV injection.
- Withdraw 36 mL of PEMGARDA from nine (9) vials into appropriately sized polypropylene syringe(s) (e.g., one 40 mL syringe or two 20 mL syringes) and inject into prepared 0.9% sodium chloride IV bag.
- The final product for administration will contain 50 mL: 36 mL of PEMGARDA and 14 mL of 0.9% sodium chloride.
- This product is preservative-free and therefore should be administered immediately.
- If immediate administration is not possible, the diluted solution may be stored at room temperature under ambient light for up to 4 hours. Do not shake the diluted solution.
Administration:
- PEMGARDA should only be administered in settings in which healthcare providers have immediate access to medications to treat a severe hypersensitivity reaction, such as anaphylaxis, and the ability to activate the emergency medical system (EMS), as necessary [see Warnings and Precautions (5.1 )].
- Attach infusion set including inline 0.2-micron filter to prepared IV bag, then prime the infusion set.
- Administer the entire 50 mL infusion using infusion pump or gravity infusion set over a minimum of 60 minutes. Due to potential overfill, the entire contents of prepared IV bag should be administered to avoid underdosing.
- Once infusion is complete, flush line with 0.9% sodium chloride.
- Clinically monitor patients during infusion and observe patients for at least 2 hours after infusion is complete [see Warnings and Precautions (5.1)].
3. Dosage Forms and Strengths
PEMGARDA is a sterile, preservative-free, clear to slightly opalescent, colorless to yellow solution available as:
- Injection: 500 mg/4 mL (125 mg/mL) in a single-dose vial
4. Contraindications
PEMGARDA is contraindicated in individuals with previous severe hypersensitivity reactions, including anaphylaxis, to any component of PEMGARDA.
5. Warnings and Precautions
5.1 Anaphylaxis
Anaphylaxis has been observed with PEMGARDA in 4 of 623 (0.6%) participants in a clinical trial [see Adverse Reactions (6.1)]. Two participants had anaphylaxis during the first infusion, and two participants had anaphylaxis during the second infusion. Anaphylaxis can be life-threatening, and two of the anaphylactic reactions in the clinical trial were reported as life-threatening. Manifestations included pruritus, flushing, urticaria, erythema, angioedema, diaphoresis, dizziness, tinnitus, wheezing, dyspnea, chest discomfort, and tachycardia. In all 4 cases, PEMGARDA was permanently discontinued.
Prior to administering PEMGARDA, consider the potential benefit of COVID-19 prevention along with the risk of anaphylaxis [Adverse Reactions (6.1), and Clinical Studies (14)].
Administer PEMGARDA only in settings in which healthcare providers have immediate access to medications to treat anaphylaxis and the ability to activate the emergency medical system (EMS), as necessary.
Clinically monitor individuals during the 60-minute infusion and for at least two hours after completion of the infusion. If signs or symptoms of an anaphylactic reaction occur, immediately discontinue administration, and initiate appropriate medications and/or supportive therapy. Discontinue PEMGARDA use permanently in individuals who experience signs or symptoms of anaphylaxis [see Contraindications (4)].
5.2 Hypersensitivity and Infusion-Related Reactions
Hypersensitivity and infusion-related reactions occurring during the infusion and up to 24 hours after the infusion have been observed with administration of PEMGARDA. Hypersensitivity or infusion-related reactions may be severe or life threatening. If signs or symptoms of a clinically significant hypersensitivity or infusion-related reaction occur, immediately discontinue administration, and initiate appropriate medications and/or supportive therapy. Signs and symptoms of hypersensitivity or infusion-related reactions may include:
- Fever, difficulty breathing, reduced oxygen saturation, chills, fatigue, arrhythmia (e.g., atrial fibrillation, sinus tachycardia, bradycardia), chest pain or discomfort, weakness, altered mental status, nausea, headache, bronchospasm, hypotension, hypertension, angioedema, throat irritation, rash including urticaria, pruritus, myalgia, vasovagal reactions (e.g., pre-syncope, syncope), dizziness, and diaphoresis.
If a mild infusion-related reaction occurs, consider slowing or stopping the infusion and administer appropriate medications and/or supportive care. Clinically monitor individuals during infusion and for at least two hours after completion of the infusion for signs and symptoms of hypersensitivity.
Hypersensitivity reactions occurring more than 24 hours after the infusion have also been reported with the use of SARS-CoV-2 monoclonal antibodies under Emergency Use Authorization.
5.3 Risk of Cross-Hypersensitivity With COVID-19 Vaccines
PEMGARDA contains polysorbate 80, which is in some COVID-19 vaccines and is structurally similar to polyethylene glycol (PEG), an ingredient in other COVID-19 vaccines [seeDescription (11)]. For individuals with a history of a severe hypersensitivity reaction to a COVID-19 vaccine, consider consultation with an allergist-immunologist prior to PEMGARDA administration.
Administration of PEMGARDA should be done under the supervision of a healthcare provider with appropriate medical support to manage severe hypersensitivity reactions. If signs and symptoms of a clinically significant hypersensitivity reaction or anaphylaxis occur during administration of PEMGARDA, immediately discontinue administration and initiate appropriate medications and/or supportive care. Clinically monitor individuals after infusion and observe for at least two hours.
5.4 Risk for COVID-19 Due to SARS-CoV-2 Viral Variants with Substantially Reduced Susceptibility to PEMGARDA
Certain SARS-CoV-2 viral variants may have substantially reduced susceptibility to PEMGARDA. PEMGARDA may not be effective at preventing COVID-19 caused by these SARS‑CoV-2 viral variants. The cell culture neutralization activity of PEMGARDA against SARS-CoV-2 viral variants is described in Microbiology ( 12.4).
Inform individuals of the increased risk, compared to other variants, for COVID-19 due to emergent SARS-CoV-2 viral variants that exhibit substantially reduced susceptibility to PEMGARDA. If signs or symptoms of COVID-19 occur, advise individuals to test for COVID-19 and seek medical attention, including starting treatment for COVID-19 as appropriate. Symptoms of COVID-19 may include fever or chills, cough, shortness of breath or difficulty breathing, fatigue, muscle or body aches, headache, new loss of taste or smell, sore throat, congestion or runny nose, nausea or vomiting, or diarrhea. 4
- 4
- For additional information on the symptoms of COVID-19, please see https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html.
6. Adverse Reactions/Side Effects
6.1 Adverse Reactions from Clinical Studies
The following adverse reactions have been observed in the clinical study of PEMGARDA that supported the EUA [see Clinical Studies (14)]. The adverse reaction rates observed in the clinical study cannot be directly compared to rates in the clinical studies of other products and may not reflect the rates observed in clinical practice. Additional adverse reactions associated with PEMGARDA may become apparent with more widespread use.
The safety of PEMGARDA is based on exposure of 623 participants who received at least one dose of PEMGARDA 4500 mg IV in one of two cohorts in the ongoing CANOPY trial. Cohort A is a single-arm, open-label trial in adults who have moderate-to-severe immune compromise (n=306), while Cohort B is a randomized, placebo-controlled trial in which adults who do not have moderate-to-severe immune compromise received PEMGARDA (n=317) or placebo (n=162). In Cohort A, 296 participants received a second dose of PEMGARDA 4500 mg IV three months after the initial dose. In Cohort B, 450 participants received a second dose of PEMGARDA 4500 mg IV or placebo three months after the initial dose. Cumulative safety with the first two doses of PEMGARDA is assessed only in Cohort A because unblinded safety data in Cohort B were not available after Day 28.
Anaphylaxis
Anaphylaxis was observed in 4 of 623 (0.6%) participants in CANOPY, all in Cohort A.
Two participants had anaphylaxis during the first infusion, and two participants had anaphylaxis during the second infusion. All four reactions led to permanent discontinuation of PEMGARDA. Three participants had complete resolution, and one participant had acute resolution with sequelae related to a flare of an underlying condition.
Symptoms of anaphylaxis during the first dose included dyspnea, diaphoresis, erythema (face), chest discomfort, and tachycardia in one participant, and flushing, dizziness, tinnitus, and wheezing in one participant. Treatment for both included diphenhydramine.
Both instances of anaphylaxis with the second dose were reported as life-threatening. Symptoms during the second infusion and following discontinuation of the infusion in both participants included pruritus, urticaria, angioedema, dyspnea, and either erythema or flushing. One participant also experienced headache, dizziness, and chest pain; additionally, pruritus, erythema, and urticaria reoccurred in this participant within 24 hours of the initial onset of anaphylaxis. Both participants were treated with diphenhydramine and epinephrine, and one participant also received oral prednisone and metoprolol for an associated flare of an underlying condition.
Systemic Infusion-Related Reactions and Hypersensitivity Reactions
First Dose
Systemic infusion-related reactions and hypersensitivity reactions (i.e., adverse events assessed as causally related) were observed with the first dose in CANOPY in 4% (24/623) of participants who received PEMGARDA across cohorts, including:
- 7% (20/306) of participants who have moderate-to-severe immune compromise (Cohort A), and
- 1% (4/317) of participants who received PEMGARDA in Cohort B
Infusion-related reactions and hypersensitivity reactions were not observed in any participants who received placebo in Cohort B.
Systemic infusion-related or hypersensitivity reactions that started within 24 hours of the first dose of PEMGARDA treatment were reported as infusion-related reaction, infusion-related hypersensitivity, hypersensitivity, fatigue, headache, tachycardia, brain fog, dermatitis, diarrhea, myalgia, nausea, paresthesia, presyncope, and tremor. All reactions were mild or moderate, but two reactions were anaphylaxis [see Box Warnings, and Warnings and Precautions (5.1, 5.2)]. Infusion-related reactions or hypersensitivity reactions led to discontinuation of the first infusion in 1% (6/623) of participants who received PEMGARDA.
First and Second Dose, Cumulative – Moderately to Severely Immunocompromised Population
Cumulatively, infusion-related reactions and hypersensitivity reactions were observed in 9% (27/306) of participants who have moderate-to-severe immune compromise, who received PEMGARDA in Cohort A of CANOPY. The severity of the reactions was generally mild (17/27) or moderate (8/27), but two reactions were life-threatening [see Boxed Warnings and Warnings and Precautions (5.1, 5.2)]. Infusion-related reactions or hypersensitivity reactions led to discontinuation of the first or second infusion in 2% (7/306) of Cohort A participants.
Two percent (5/306) of participants who have moderate-to-severe immune compromise (Cohort A) had an infusion-related reaction or hypersensitivity reaction with both the first and second dose of PEMGARDA.
Local Infusion Site Reactions
First and Second Dose, Cumulative
Cumulatively, local infusion site reactions were observed in 2% (6/306) of participants who have moderate-to-severe immune compromise (Cohort A) with either the first or second dose. No local infusion site reactions were observed in Cohort B. Local reactions were reported as infusion site bruising, infusion site erythema, infusion site rash, and injection site reaction. All local reactions were mild, and none led to treatment discontinuation.
Cumulatively, infusion site infiltration, extravasation, or vein rupture was noted in 5% (14/306) of participants who have moderate-to-severe immune compromise (Cohort A) with either the first or second dose.
Other Common Adverse Events
First and Second Dose, Cumulative– Moderately to Severely Immunocompromised Population
In addition to systemic and local infusion-related/hypersensitivity reactions described above, the most common (≥2%) treatment-emergent adverse events, irrespective of causality, observed with PEMGARDA in participants who have moderate-to-severe immune compromise (Cohort A) in CANOPY were upper respiratory tract infection (6%), viral infection (4%), influenza-like illness (3%), fatigue (3%), headache (2%), and nausea (2%).
6.4 Required Reporting for Serious Adverse Events and Medication Errors
The prescribing healthcare provider and/or the provider’s designee is/are responsible for mandatory reporting of all serious adverse events* and medication errors potentially related to PEMGARDA within 7 calendar days from the healthcare provider’s awareness of the event, using FDA Form 3500 (for information on how to access this form, see below). The FDA requires that such reports, using FDA Form 3500, include the following:
- Patient demographics and baseline characteristics (e.g., patient identifier, age or date of birth, sex, weight, ethnicity, and race).
- A statement “PEMGARDA use for the pre-exposure prophylaxis of COVID-19 under Emergency Use Authorization (EUA)” under the “Describe Event, Problem, or Product Use/Medication Error”heading.
- Information about the serious adverse event or medication error (e.g., signs and symptoms, test/laboratory data, complications, timing of drug initiation in relation to the occurrence of the event, duration of the event, treatment required to mitigate the event, evidence of event improvement/disappearance after stopping or reducing the dosage, evidence of event reappearance after reintroduction, clinical outcomes).
- Patient’s preexisting medical conditions and use of concomitant products.
- Information about the product (e.g., dosage, route of administration, NDC #).
Submit serious adverse event and medication error reports using FDA Form 3500 to FDA MedWatch using one of the following methods:
- Complete and submit the report online: www.fda.gov/medwatch/report.htm.
- Complete and submit a postage-paid FDA Form 3500
( https://www.fda.gov/media/76299/download) and return by:- Mail to MedWatch, 5600 Fishers Lane, Rockville, MD 20852-9787, or
- Fax to 1-800-FDA (332)-0178, or
- Call 1-800-FDA (332)-1088 to request a reporting form.
In addition, please provide a copy of all FDA MedWatch forms to:
Invivyd, Inc.
Email: pv@invivyd.com
Or call Invivyd, Inc. at 1-800-890-3385 to report serious adverse events.
The prescribing healthcare provider and/or the provider’s designee is/are responsible for mandatory responses to requests from FDA for information about serious adverse events and medication errors following receipt of PEMGARDA.
*Serious adverse events are defined as:
- Death
- A life-threatening adverse event
- Inpatient hospitalization or prolongation of existing hospitalization
- A persistent or significant incapacity or substantial disruption of the ability to conduct normal life functions
- A congenital anomaly/birth defect
- Other important medical events, which may require a medical or surgical intervention to prevent death, a life-threatening event, hospitalization, disability, or congenital anomaly
Related/similar drugs
7. Drug Interactions
Drug-drug interaction studies have not been performed. PEMGARDA is not renally excreted or metabolized by cytochrome P450 enzymes; therefore, interactions with concomitant medications that are renally excreted or that are substrates, inducers, or inhibitors of cytochrome P450 enzymes are unlikely [seeClinical Pharmacology (12.3)].
8. Use In Specific Populations
8.1 Pregnancy
Risk Summary:
There are insufficient data to evaluate a drug-associated risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes. PEMGARDA should only be used during pregnancy if the potential benefit outweighs the potential risk for the mother and the fetus.
Nonclinical reproductive toxicity studies have not been performed with pemivibart. In tissue cross-reactivity studies using human fetal tissues, no off-target binding was detected for pemivibart. Human immunoglobulin G1 (IgG1) antibodies are known to cross the placental barrier; therefore, pemivibart has the potential to be transferred from the mother to the developing fetus. It is unknown whether the potential transfer of pemivibart provides any treatment benefit or risk to the developing fetus.
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the US general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
8.2 Lactation
Risk Summary:
There are no available data on the presence of PEMGARDA in human or animal milk, the effects on the breastfed infant, or the effects on milk production. Maternal IgG is known to be present in human milk. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for PEMGARDA and any potential adverse effects on the breastfed infant from PEMGARDA.
8.4 Pediatric Use
PEMGARDA is not authorized for use in pediatrics less than 12 years of age or weighing less than 40 kg. The safety and effectiveness of PEMGARDA has not been established in pediatrics.
The recommended dosing regimen is expected to result in comparable serum exposures of pemivibart in adolescents 12 years of age and older and weighing at least 40 kg as observed in adults, since adults with similar body weight have been included in the CANOPY study [seeAdverse Reactions (6.1) and Clinical Studies (14)].
8.5 Geriatric Use
Of the 623 participants who received PEMGARDA in the CANOPY trial, 156 (25%) were aged ≥65 years and 31 (5%) were aged ≥75 years. Based on population pharmacokinetic (PK) analyses, there was no clinically meaningful difference of age on the PK of pemivibart.
10. Overdosage
Doses above 4500 mg PEMGARDA (the authorized dose of pemivibart) were not administered in clinical studies. There is no specific treatment for overdose with PEMGARDA.
11. Pemgarda Description
Pemivibart is a human IgG1 mAb produced by a Chinese Hamster Ovary cell line and has a molecular weight of 147.51 kDa.
PEMGARDA (pemivibart) injection is a sterile, preservative-free, clear to slightly opalescent, colorless to yellow solution for intravenous infusion after dilution. Each 4 mL of solution contains 500 mg of pemivibart, glycine (33.03 mg), L-arginine hydrochloride (63.2 mg), L‑histidine (3.67 mg), L-histidine hydrochloride monohydrate (3.43 mg), L-methionine (5.97 mg), polysorbate 80 (1.2 mg), sterile water for injection (USP). The pH is 6.2.
12. Pemgarda - Clinical Pharmacology
12.2 Pharmacodynamics
Available data suggest a positive relationship between serum neutralizing antibody titers and COVID-19 pre-exposure-prophylactic efficacy using clinical data (completed prior to the emergence of Omicron and Omicron lineage VOCs) and drug concentration data of neutralizing human monoclonal antibodies against SARS-CoV-2.
Following single-dose administration of pemivibart 4500 mg IV, calculated geometric mean titer values (pemivibart concentration divided by the pseudotyped virus-like particle neutralization assay EC50 value against JN.1) [see Microbiology ( 12.4)] range from 2942 (on Day 90) to 19227 (end of infusion on Day 1). After the repeat dose of pemivibart 4500 mg IV every 3 months, it is anticipated that the range of titers at steady-state will be approximately 33% higher than those observed following the first dose administration.
12.3 Pharmacokinetics
A summary of PK parameters of pemivibart following administration of a single 4500 IV dose of pemivibart to adults based on population PK modeling is provided in Table 1.
Table 1: Summary Statistics of Population PK Parameters of Pemivibart Following a Single 4500 mg Intravenous Dose in Adults
| Parameter | Pemivibart |
|---|---|
|
C max (μg/mL) |
1750 (38.2) |
|
C Day 28 (μg/mL) |
460 (40.7) |
|
C Day 90 (μg/mL) |
175 (44.4) |
|
AUC0 -3 months (days × μg/mL) |
36600 (40.4) |
|
T 1/2 (days) |
44.8 (28.1-64.6) |
|
Accumulation ratio |
1.33 |
|
CL (L/d) |
0.0909 (23.3) |
|
V ss (L) |
5.54 (17.0) |
|
Metabolism |
Catabolic pathways; same manner as endogenous IgG |
|
Excretion |
Not likely to undergo renal excretion |
AUC 0-3 months= area under the serum concentration-time curve from Day 0 to Month 3; CL=renal clearance; C max=maximum concentration; PK=pharmacokinetic; T 1/2=half-life; V ss=steady state volume of distribution.
Note: All values presented as geometric mean (% covariance), except for T 1/2, which is presented as median (min, max). Numerical values are post-hoc PK parameter estimates for subjects enrolled in Phase 3 CANOPY.
Specific Populations:
The PK of pemivibart was not substantially affected by age, sex, or race based on a population PK analysis to the pooled data from VYD222-1-001 and Phase 3 CANOPY. Body weight is not expected to have a clinically relevant effect on the PK of pemivibart in individuals with body weights ranging from 43 to 190 kg through 3 months postdose.
Patients with Immune Compromise
Population PK analysis showed immune compromise status had no clinically relevant effect on the PK of pemivibart.
Pediatric Patients
The PK of pemivibart in pediatric individuals has not been evaluated. The dosing regimen is expected to result in comparable plasma exposures of pemivibart in pediatric individuals 12 years of age or older who weigh at least 40 kg as observed in adult individuals [see Use in Specific Populations(8.4)].
Patients with Renal Impairment
Renal impairment is not expected to impact the PK of pemivibart since mAbs with molecular weight >69 kDa are known not to undergo renal elimination. Similarly, dialysis is not expected to impact the PK of pemivibart.
Patients with Hepatic Impairment
Pemivibart is not anticipated to be impacted by hepatic impairment. Pemivibart is expected to be degraded into small peptides and amino acids via catabolic pathways in the same manner as other IgG mAbs and human endogenous IgG antibodies.
12.4 Microbiology
Mechanism of Action:
Pemivibart is a recombinant human monoclonal IgG1λ antibody that targets the SARS-CoV-2 spike protein receptor binding domain (RBD), thereby inhibiting virus attachment to the human ACE2 receptor on host cells. Amino acid substitutions in the Fc region (M435L/N441A) of pemivibart extend serum half-life. Pemivibart binds the spike RBD proteins of ancestral SARS‑CoV-2 B.1 (D614G) and Omicron variants BA.1, BA.2, and BA.4/5 with equilibrium dissociation constants (KD) of 2.1 nM, 18 nM, 13.5 nM, and 15.9 nM, respectively, and blocks attachment of ancestral SARS-CoV-2 and BA.2.86 variant RBD proteins to the human ACE2 receptor with IC50 values of 0.068 nM (10 ng/mL) and 23 nM (3,370 ng/mL), respectively.
Antiviral Activity:
Pemivibart neutralized authentic SARS-CoV-2 isolates in Vero E6 or Vero E6-TMPRSS2 cells with EC50 values of 0.165-0.230 nM (24.3-34 ng/mL) against B.1, and 0.075 nM (11 ng/mL) against B.1.617.2 (Delta). For Omicron variants, EC50 values were 0.096 nM (14.2 ng/mL) against BA.1, 0.039 nM (5.8 ng/mL) against BA.2, 0.175 nM (25.8 ng/mL) against BA.4.1, 0.80-4.48 nM (118-661.2 ng/mL) against XBB.1.16, 1.97-3.25 nM (290-479.9 ng/mL) against XBB.1.5, 9.8 nM (1,445 ng/mL) against EG.5.1, and 3.59 nM (529.4 ng/mL) against HV.1.
Pemivibart neutralization susceptibility of historic and contemporary SARS-CoV-2 variants was evaluated using a pseudotyped, luciferase-expressing, lentivirus virus-like particle (VLP) assay. Pemivibart neutralized SARS-CoV-2 spike protein-pseudotyped VLPs representing B.1 and pre-Omicron variants with EC50 values ranging from 0.022 to 0.083 nM (3.2 to 12.2 ng/mL), and Omicron-lineage variants with EC50 values ranging from 0.198 to 14.3 nM (29.2 to 2,112 ng/mL) (Table 2).
Preliminary, non-peer-reviewed data in the public domain 5 indicate that KP.3.1.1 may have substantially reduced susceptibility to pemivibart. The Fact Sheet will be updated as more data become available.
Table 2: Pemivibart Pseudotyped Virus-Like Particle Neutralization Data for SARS‑CoV-2 Variants
| Pango lineage | RBD substitutions relative to B.1
present in pseudotyped VLPs | Pemivibart | |
|---|---|---|---|
| Mean EC
50 values ng/mL
(SD / range) a | Fold-change from JN.1 b | ||
|
Dominant Variant Circulating at Time of Emergency Use Authorization |
|||
|
JN.1 |
I332V, G339H, K356T, S371F, S373P, S375F, T376A, R403K, D405N, R408S, K417N, N440K, V445H, G446S, N450D, L452W, L455S, N460K, S477N, T478K, N481K, V483del, E484K, F486P, Q498R, N501Y, Y505H |
74.6 (5.8) |
1 |
|
Historic and Contemporary Variants |
|||
|
B.1 |
8.4 (3) |
0.1 |
|
|
B.1.1.7 |
N501Y |
11.4 |
0.2 |
|
B.1.351 |
K417N, E484K, N501Y |
9 |
0.1 |
|
P.1 |
K417T, E484K, N501Y |
12.2 |
0.2 |
|
B.1.617.2 |
L452R, T478K |
5.2 (4.2-6.2) |
0.1 |
|
B.1.427 |
L452R |
3.2 |
0.04 |
|
P.2 |
E484K |
9.3 |
0.1 |
|
B.1.526 |
E484K |
8.6 |
0.1 |
|
B.1.621 |
R346K, E484K, N501Y |
9.5 |
0.1 |
|
BA.1 |
G339D, S371L, S373P, S375F, K417N, N440K, G446S, S477N, T478K, E484A, Q493R, G496S, Q498R, N501Y, Y505H |
121.4 |
1.6 |
|
BA.2 |
G339D, S371F, S373P, S375F, T376A, D405N, R408S, K417N, N440K, S477N, T478K, E484A, Q493R, Q498R, N501Y, Y505H |
44.6 (6.5) |
0.6 |
|
BA.4/BA.5 |
G339D, S371F, S373P, S375F, T376A, D405N, R408S, K417N, N440K, L452R, S477N, T478K, E484A, F486V, Q498R, N501Y, Y505H |
47.9 (29.7-66.2) |
0.6 |
|
BA.4.6 |
G339D, R346T, S371F, S373P, S375F, T376A, D405N, R408S, K417N, N440K, L452R, S477N, T478K, E484A, F486V, Q498R, N501Y, Y505H |
29.2 |
0.4 |
|
BF.7 |
G339D, R346T, S371F, S373P, S375F, T376A, D405N, R408S, K417N, N440K, L452R, S477N, T478K, E484A, F486V, Q498R, N501Y, Y505H |
72.7 |
1.0 |
|
BQ.1 |
G339D, R346T, S371F, S373P, S375F, T376A, D405N, R408S, K417N, N440K, K444T, L452R, S477N, T478K, E484A, F486V, Q498R, N501Y, Y505H |
164.6 |
2.2 |
|
BQ.1.1 |
G339D, R346T, S371F, S373P, S375F, T376A, D405N, R408S, K417N, N440K, K444T, L452R, N460K, S477N, T478K, E484A, F486V, Q498R, N501Y, Y505H |
102.1 |
1.4 |
|
BA.2.75 |
G339H, S371F, S373P, S375F, T376A, D405N, R408S, K417N, N440K, G446S, N460K, S477N, T478K, E484A, Q498R, N501Y, Y505H |
1,364.6 |
18.3 |
|
BN.1 |
G339H, R346T, K356T, S371F, S373P, S375F, T376A, D405N, R408S, K417N, N440K, G446S, N460K, S477N, T478K, E484A, F490S, Q498R, N501Y, Y505H |
2,112.0 |
28.3 |
|
XBB |
G339H, R346T, L368I, S371F, S373P, S375F, T376A, D405N, R408S, K417N, N440K, V445P, G446S, N460K, S477N, T478K, E484A, F486S, F490S, Q493R, Q498R, N501Y, Y505H |
152.2 |
2.0 |
|
XBB.1 |
G339H, R346T, L368I, S371F, S373P, S375F, T376A, D405N, R408S, K417N, N440K, V445P, G446S, N460K, S477N, T478K, E484A, F486S, F490S, Q493R, Q498R, N501Y, Y505H |
121.1 |
1.6 |
|
XBB.1.5 |
G339H, R346T, L368I, S371F, S373P, S375F, T376A, D405N, R408S, K417N, N440K, V445P, G446S, N460K, S477N, T478K, E484A, F486P, F490S, Q498R, N501Y, Y505H |
104.3 |
1.4 |
|
XBB.1.16 |
G339H, R346T, L368I, S371F, S373P, S375F, T376A, D405N, R408S, K417N, N440K, V445P, G446S, N460K, S477N, T478R, E484A, F486P, F490S, Q498R, N501Y, Y505H |
77.6 (18.1) |
1.0 |
|
XBB.1.5.1 |
G339H, R346T, L368I, S371F, S373P, S375F, T376A, D405N, R408S, K417N, N440K, V445P, G446S, N460K, S477N, T478K, E484A, F486P, F490S, Q498R, N501Y, Y505H |
80.0 (8.9) |
1.1 |
|
XBB.1.5.10 |
G339H, R346T, L368I, S371F, S373P, S375F, T376A, D405N, R408S, K417N, N440K, V445P, G446S, F456L, N460K, S477N, T478K, E484A, F486P, F490S, Q498R, N501Y, Y505H |
108.1 (35.5) |
1.4 |
|
EU.1.1 |
G339H, R346T, L368I, S371F, S373P, S375F, T376A, D405N, R408S, I410V, K417N, N440K, V445P, G446S, N460K, S477N, T478K, E484A, F486P, F490S, Q498R, N501Y, Y505H, P521S |
52.1 (10.6) |
0.7 |
|
JD.1.1 |
G339H, R346T, L368I, S371F, S373P, S375F, T376A, D405N, R408S, K417N, N440K, V445P, G446S, L455F, F456L, N460K, A475V, S477N, T478K, E484A, F486P, F490S, Q498R, N501Y, Y505H |
101.9 (4.9) |
1.4 |
|
XBB.2.3 |
G339H, R346T, L368I, S371F, S373P, S375F, T376A, D405N, R408S, K417N, N440K, V445P, G446S, N460K, S477N, T478K, E484A, F486P, F490S, Q498R, N501Y, Y505H, P521S |
87.0 (15.5) |
1.2 |
|
GE.1.2.1 |
G339H, R346T, L368I, S371F, S373P, S375F, T376S, D405N, R408S, K417N, N440K, V445P, G446S, N460K, S477N, E484A, F486P, F490S, Q498R, N501Y, Y505H |
72.1 (14.8) |
1.0 |
|
FL.1.5.1 |
G339H, R346T, L368I, S371F, S373P, S375F, T376A, D405N, R408S, K417N, N440K, V445P, G446S, F456L, N460K, S477N, T478R, E484A, F486P, F490S, Q498R, N501Y, Y505H |
102.1 (8.8) |
1.4 |
|
HV.1 |
G339H, R346T, L368I, S371F, S373P, S375F, T376A, D405N, R408S, K417N, N440K, V445P, G446S, L452R, F456L, N460K, S477N, T478K, E484A, F486P, F490S, Q498R, N501Y, Y505H |
41.2 (9.2) |
0.6 |
|
HK.3 |
G339H, R346T, L368I, S371F, S373P, S375F, T376A, D405N, R408S, K417N, N440K, V445P, G446S, L455F, F456L, N460K, S477N, T478K, E484A, F486P, F490S, Q498R, N501Y, Y505H |
72.3 (7.7) |
1.0 |
|
BA.2.86 |
I332V, G339H, K356T, S371F, S373P, S375F, T376A, R403K, D405N, R408S, K417N, N440K, V445H, G446S, N450D, L452W, N460K, S477N, T478K, N481K, V483del, E484K, F486P, Q498R, N501Y, Y505H |
167.7 (4.4) |
2.2 |
|
JN.1 |
I332V, G339H, K356T, S371F, S373P, S375F, T376A, R403K, D405N, R408S, K417N, N440K, V445H, G446S, N450D, L452W, L455S, N460K, S477N, T478K, N481K, V483del, E484K, F486P, Q498R, N501Y, Y505H |
74.6 (5.8) |
1.0 |
|
JN.1.11.1 |
I332V, G339H, K356T, S371F, S373P, S375F, T376A, R403K, D405N, R408S, K417N, N440K, V445H, G446S, N450D, L452W, L455S, F456L, N460K, S477N, T478K, N481K, V483del, E484K, F486P, Q498R, N501Y, Y505H |
288.0 (64.9) |
3.9 |
|
JN.1.13.1 |
I332V, G339H, R346T, K356T, S371F, S373P, S375F, T376A, R403K, D405N, R408S, K417N, N440K, V445H, G446S, N450D, L452W, L455S, N460K, S477N, T478K, N481K, V483del, E484K, F486P, Q498R, N501Y, Y505H |
220.3 (32.5) |
3.0 |
|
KQ.1 |
I332V, G339H, R346T, K356T, S371F, S373P, S375F, T376A, R403K, D405N, R408S, K417N, N440K, V445H, G446S, N450D, L452W, L455S, N460K, S477N, T478K, N481K, V483del, E484K, F486P, Q498R, N501Y, Y505H |
208.5 (30.3) |
2.8 |
|
KP.1.1 |
I332V, G339H, R346T, K356T, S371F, S373P, S375F, T376A, R403K, D405N, R408S, K417N, N440K, V445H, G446S, N450D, L452W, L455S, F456L, N460K, S477N, T478K, N481K, V483del, E484K, F486P, Q498R, N501Y, Y505H |
174.2 (28.7) |
2.3 |
|
KP.2 |
I332V, G339H, R346T, K356T, S371F, S373P, S375F, T376A, R403K, D405N, R408S, K417N, N440K, V445H, G446S, N450D, L452W, L455S, F456L, N460K, S477N, T478K, N481K, V483del, E484K, F486P, Q498R, N501Y, Y505H, |
154.1 (29.4) |
2.1 |
|
KP.3 |
I332V, G339H, K356T, S371F, S373P, S375F, T376A, R403K, D405N, R408S, K417N, N440K, V445H, G446S, N450D, L452W, L455S, F456L, N460K, S477N, T478K, N481K, V483del, E484K, F486P, Q493E, Q498R, N501Y, Y505H |
223.0 (62.6) |
3.0 |
|
KP.3.1.1 c |
(S31del) d, I332V, G339H, K356T, S371F, S373P, S375F, T376A, R403K, D405N, R408S, K417N, N440K, V445H, G446S, N450D, L452W, L455S, F456L, N460K, S477N, T478K, N481K, V483del, E484K, F486P, Q493E, Q498R, N501Y, Y505H |
Pending e, f |
|
EC 50=half-maximal inhibitory concentration; Pango=Phylogenetic Assignment of Named Global Outbreak; RBD=receptor binding domain; SARS-CoV-2=severe acute respiratory syndrome coronavirus 2; WT=wild-type.
a. EC 50 values are reported as the mean along with range when data were obtained from 2 independent experiments or as mean and standard deviation when data were obtained from 3 or more independent experiments. 5,000 ng/mL was the upper concentration tested. Note: The % CV for B.1 was 35.7% based on 30 replicates from 13 previous experiments performed in this pseudotyped VLP assay.
b. Fold change in EC50 value for a given variant was calculated by dividing the observed EC50 value by the average observed EC50 value for JN.1 of 74.6 ng/mL obtained from a previous experiment performed using the same pseudotyped VLP neutralization assay platform.
c. Spike substitutions are inferred based on the consensus data for KP.3.1.1 presented by Outbreak.info.
d. KP.3.1.1 spike differs from KP.3 with a deletion at S31, which is outside of the RBD.
e. Preliminary, non-peer-reviewed data in the public domain indicate that KP.3.1.1 may have substantially reduced susceptibility to pemivibart.
f. The Fact Sheet will be updated as more data become available.
Pemivibart has not been directly evaluated for Fc-mediated effector functions or antibody-dependent enhancement (ADE) of infection. The parent antibody of pemivibart, which contains an identical Fc region and targets an overlapping epitope, exhibited antibody-dependent cellular phagocytosis (ADCP) and antibody-dependent complement deposition (ADCD), but failed to exhibit detectable ADE in cell culture.
Antiviral Resistance:
There is a potential risk of prophylaxis failure due to the emergence of a pemivibart-resistant SARS-CoV-2 variant. Prescribing healthcare providers should consider the prevalence of SARS‑CoV-2 variants in their area, where data are available, when considering prophylactic treatment options.
Data are limited regarding the scope of spike substitutions in Omicron-lineage variants that may confer significantly reduced susceptibility to pemivibart. Escape variants were identified following serial passage of SARS-CoV-2 (Omicron XBB.1.5.6) in cell culture in the presence of pemivibart that contained a T500N spike substitution or a combination of R498Q, Y501N, and H505Y spike substitutions. Each of these substitutions is within 5 Å of the pemivibart binding interface.
Continuous evaluations remain ongoing of pemivibart neutralization susceptibility of variants that emerge and are identified through global surveillance.
Cross-resistance:
Cross-resistance is not expected between pemivibart and currently approved/authorized COVID‑19 therapies, including remdesivir, nirmatrelvir, or molnupiravir, since pemivibart has a distinct mechanism of action and targets a different viral protein than these drugs.
- 5
- Wang Q, Guo Y, Ho J, Ho DD. Pemivibart is less active against recent SARS-CoV-2 JN.1 sublineages. [Accessed on 19 August 2024, from https://doi.org/10.1101/2024.08.12.607496]
13. Nonclinical Toxicology
14. Clinical Studies
14.1 Overview of Immunobridging Approach
To support this EUA, an immunobridging approach was used to determine if PEMGARDA may be effective for pre-exposure prophylaxis of COVID-19. Immunobridging is based on the serum neutralization titer-efficacy relationships identified with other neutralizing human monoclonal antibodies against SARS-CoV-2. This includes adintrevimab, the parent mAb of pemivibart, and other mAbs that were previously authorized for EUA. To support immunobridging, serum neutralization titer was utilized to compare PEMGARDA to previous mAbs [see Clinical Pharmacology (12.2)].
14.2 Pre-exposure Prophylaxis of COVID-19 (VYD222-PREV-001 [CANOPY])
CANOPY [NCT06039449] is an ongoing clinical trial evaluating PEMGARDA for the pre-exposure prophylaxis of COVID-19 in adults ≥18 years of age in two cohorts.
- Cohort A: single-arm, open-label trial in adults who have moderate-to-severe immune compromise.
- Cohort B: placebo-controlled, randomized trial in adults who do not have moderate-to-severe immune compromise.
A total of 623 participants, 306 in Cohort A and 317 in Cohort B, received at least one dose of PEMGARDA 4500 mg in the trial. In Cohort A, 296 participants received a second dose of PEMGARDA 4500 mg at Month 3. In Cohort B, 162 participants received at least one dose of placebo, and a total of 450 participants received a second dose of either PEMGARDA 4500 mg or placebo (blinded) at Month 3. The trial excluded participants with known or suspected SARS‑CoV-2 infection within 120 days before randomization or a positive SARS-CoV-2 antigen test or RT-PCR at the time of screening. The primary data to support this EUA comes from Cohort A and is summarized below.
Participants in Cohort A were mostly female (61%), White (86%) or Black/African American (12%), and not Hispanic or Latino (94%).
The median age was 59 years, with 31% aged 65 years or older. All participants had underlying moderate-to-severe immune compromise, including:
- 65% taking high-dose corticosteroids/other immunosuppressive medications
- 13% acute leukemia, chronic lymphocytic leukemia, non-Hodgkin, lymphoma, or multiple myeloma (regardless of treatment)
- 12% primary immunodeficiency
- 11% solid organ transplant recipient
- 9% advanced HIV infection
- 7% actively treated for solid tumor or hematologic malignancies
Immunobridging Results
The primary efficacy objective of Cohort A was to evaluate protection against symptomatic COVID-19 based on calculated titers against SARS-CoV-2 following PEMGARDA administration by immunobridging to historical data from the EVADE study, which provided evidence of clinical efficacy of adintrevimab, the parent mAb of pemivibart. The primary immunobridging endpoint for Cohort A compared the ratio of the geometric mean titers between pemivibart against the relevant variant (JN.1) at Day 28 to the reference titer at Day 28. The reference titer at Day 28 was the extrapolated titer from the Day 90 adintrevimab titer [which was calculated based on Day 90 concentration of adintrevimab divided by the EC50 value against the B.1.617.2 (Delta) variant] using the half-life of pemivibart. Immunobridging would be established if the lower limit of the 2-sided 90% CI of the ratio of the geometric mean titer value is greater than 0.8.
The immunobridging results are as follows: the geometric mean ratio between the calculated titer for pemivibart against JN.1 (based on a pseudotyped VLP neutralization assay EC50 value of 74.6 ng/mL) and the calculated titer for adintrevimab against Delta (based on an authentic virus neutralization assay EC50 value of 7 ng/mL) was 0.70 (90% CI: 0.68-0.72). However, there are limitations of this analysis, including differences in the methodologies of the assays used to determine the EC50 values for pemivibart and adintrevimab against the respective variants. In an analysis using an identical cell-based assay (a pseudotyped VLP neutralization assay), for the calculated titer comparison between pemivibart against JN.1 (based on an EC50 value of 74.6 ng/mL) and adintrevimab against Delta (based on an EC50 value of 3.5 ng/mL), the geometric mean ratio was 0.35 (90% CI: 0.34-0.36).This analysis highlights the impact of even modest differences in EC50 values on the results of the primary endpoint.
In a supplementary immunobridging analysis, the titer values of pemivibart against JN.1 [see Clinical Pharmacology (12.2)]were compared, using published literature, to the titers associated with efficacy of three other SARS-CoV-2 targeting mAbs in prior clinical trials. The range of titers achieved with pemivibart for 3 months following administration of 4500 mg IV were consistent with the titer levels associated with clinical efficacy in prior clinical trials evaluating certain monoclonal antibodies for the prevention of COVID-19.
Exploratory Clinical Efficacy Results
An exploratory efficacy objective of Cohort B was to evaluate clinical efficacy of PEMGARDA compared to placebo in the prevention of RT-PCR-confirmed COVID-19 in randomized participants without SARS-CoV-2 infection at baseline and without moderate-to-severe immune compromise. Table 3 provides the results for the Cohort B exploratory clinical efficacy endpoint. Most infection events occurred during a period of time when JN.1 and variants with similar susceptibilities were dominant. No deaths or COVID-19-related hospitalizations occurred in either treatment arm of Cohort B through Month 6. PEMGARDA is not authorized for use in individuals who do not have moderate-to-severe immune compromise.
Table 3: Exploratory Clinical Efficacy Results in Randomized Participants without SARS CoV-2 Infection at Baseline in CANOPY Cohort B (Adults who do not have Moderate-to-Severe Immune Compromise)
| PEMGARDA
n=317 | Placebo
n=160 |
|
|---|---|---|
|
RT-PCR-confirmed symptomatic COVID-19,COVID-19-related hospitalization, or all-cause death athrough Month 3 b |
||
|
Proportion: n (%) |
1 (0.3) |
8 (5.0) |
|
Standardized Relative Risk Reduction (95% CI) |
94% (50%, 99%) |
|
|
RT-PCR-confirmed symptomatic COVID-19,COVID-19-related hospitalization, or all-cause deathathrough Month 6 c |
||
|
Proportion: n (%) |
6 (1.9) |
19 (11.9) |
|
Standardized Relative Risk Reduction (95% CI) |
84% (61%, 94%) |
|
a No COVID-19-related hospitalizations or deaths occurred in either treatment arm of Cohort B through Month 6.
b Following the initial dosing period of the trial
c Cumulative through Month 6, following the initial dosing and redosing periods of the trial
An exploratory objective of Cohort A was to collect data on RT-PCR-confirmed COVID-19, COVID-19-related hospitalizations, or all-cause death in participants who received a full initial dose of study drug. Table 4 provides these results for Cohort A. No COVID-19-related hospitalizations occurred in Cohort A through Month 6. Two all-cause deaths (one due to an unknown cause and one due to suicide) occurred in Cohort A through Month 6.
Table 4: Rates of RT-PCR-confirmed COVID-19, COVID-19-Related Hospitalizations, or All-Cause Death in Participants in CANOPY Cohort A (Adults who have Moderate-to-Severe Immune Compromise)
|
PEMGARDA
|
|
|
RT-PCR-confirmed symptomatic COVID-19,COVID-19-related hospitalization, or all-cause death athrough Month 3 b |
|
|
Proportion: n (%) |
3 (1.0) |
|
RT-PCR-confirmed symptomatic COVID-19,COVID-19-related hospitalization, or all-cause deathathrough Month 6 c |
|
|
Proportion: n (%) |
11 (3.7) |
a No COVID-19-related hospitalizations occurred in Cohort A through Month 6. Two all-cause deaths (one due to an unknown cause and one due to suicide) occurred in Cohort A through Month 6.
b Following the initial dosing period of the trial
c Cumulative through Month 6, following the initial dosing and redosing periods of the trial
14.3 Overall Benefit-Risk Assessment and Limitations of Data Supporting the Benefits of the Product
Based on the totality of scientific evidence available, it is reasonable to believe that PEMGARDA may be effective for pre-exposure prophylaxis of COVID-19 caused by susceptible SARS-CoV-2 variants in the authorized population [see Microbiology (12.4)]. The calculated pemivibart serum neutralizing antibody titers for the JN.1 variant were consistent with the titer levels associated with efficacy in prior clinical trials of adintrevimab and certain other monoclonal antibody products previously authorized for the prevention of COVID-19. The exploratory clinical results from Cohort B of CANOPY also provide support that PEMGARDA may be effective for pre-exposure prophylaxis of COVID-19 caused by the JN.1 variant and other similarly susceptible SARS-CoV-2 variants in the authorized use population.
There are limitations of the immunobridging data supporting the benefits of PEMGARDA. Evidence of clinical efficacy for other neutralizing human monoclonal antibodies against SARS-CoV-2 was based on different populations and SARS-CoV-2 variants that are no longer circulating. Additionally, the variability associated with cell-based EC50 value determinations, along with limitations related to PK data and efficacy estimates for the mAbs in prior clinical trials, impact the ability to precisely estimate protective titer ranges. The potential benefits of PEMGARDA for pre-exposure prophylaxis of COVID-19 caused by variants other than JN.1 may vary based on variant susceptibility and national variant frequencies [see Microbiology (12.4)].
16. How is Pemgarda supplied
PEMGARDA injection is a sterile, preservative-free, clear to slightly opalescent, colorless to yellow solution supplied in a single-dose 6R vial intended for intravenous infusion only.
| Antibody | Concentration | Package Size | NDC |
|---|---|---|---|
|
Pemivibart |
500 mg/4 mL vial (125 mg/mL) |
Nine vials per carton |
81960-031-03 |
Refrigerate unopened vials at 2 ℃ to 8 °C (36 ℉ to 46 °F) in the original carton to protect from light.
Do not freeze or shake. Do not use if seal is broken or missing.
17 PATIENT COUNSELING INFORMATION
As a prescribing healthcare practitioner, you must communicate to the patient, parent, and caregiver information consistent with the “FACT SHEET FOR PATIENTS, PARENTS OR CAREGIVERS” and provide them with a copy of this Fact Sheet prior to administration of PEMGARDA.
Anaphylaxis
Inform individuals that anaphylaxis has been observed with PEMGARDA. Advise individuals that they will be monitored during and for at least two hours after completion of the infusion. In those who experience signs or symptoms of anaphylaxis, PEMGARDA use will be discontinued permanently [see Boxed Warnings, and Warnings and Precautions (5.1)].
Hypersensitivity and Infusion-Related Reactions
Inform individuals that hypersensitivity and infusion-related reactions have occurred during the infusion and up to 24 hours after the infusion with PEMGARDA. These hypersensitivity or infusion-related reactions may be severe or life threatening. Inform individuals that they will be monitored during and for at least two hours after completion of the infusion for signs and symptoms of hypersensitivity [see Warnings and Precautions (5.2)].
Dosing
Inform individuals that they may need to receive additional doses of PEMGARDA every 3 months if ongoing protection is needed [see Dosage and Administration (2)and Clinical Pharmacology (12)].
Risk for COVID-19 Due to SARS-CoV-2 Viral Variants With Substantially Reduced Susceptibility to PEMGARDA
Certain SARS-CoV-2 viral variants may have substantially reduced susceptibility to PEMGARDA. PEMGARDA may not be effective at preventing COVID-19 caused by these SARS‑CoV-2 viral variants. Inform individuals of the increased risk, compared to other variants, for COVID-19 due to SARS-CoV-2 viral variants that exhibit substantially reduced susceptibility to PEMGARDA. If signs or symptoms of COVID-19 occur, advise individuals to test for COVID‑19 and seek medical attention, including starting treatment for COVID-19 as appropriate [see Warnings and Precautions (5.4)].
18 MANUFACTURER INFORMATION
For additional information, visit: http://www.pemgarda.com/or scan the code below:

Manufactured and distributed by:
Invivyd, Inc.
1601 Trapelo Road, Suite 178
Waltham, MA 02451
INVIVYD™, PEMGARDA™, and the Ribbon logos are trademarks of Invivyd, Inc.
©2024 Invivyd, Inc. All rights reserved.
Revised 08/2024
FACT SHEET FOR PATIENTS, PARENTS, AND CAREGIVERS
What is the most important information I should know about PEMGARDA?
PEMGARDA may cause serious side effects, including:
- A serious allergic reaction called anaphylaxis.Anaphylaxis can be life-threatening and can happen during or after your infusion of PEMGARDA. In case you have a severe allergic reaction to PEMGARDA and need medical help right away, you will receive PEMGARDA in a healthcare setting. Your healthcare provider will monitor you for allergic reactions during your infusion and for at least 2 hours after you are finished receiving PEMGARDA. Your healthcare provider will stop PEMGARDA right away if you develop signs or symptoms of anaphylaxis or severe allergic reaction. Tell your healthcare provider right away if you get any of the following signs or symptoms of anaphylaxis during or after your infusion of PEMGARDA:
| itching | dizziness |
| flushing | ringing in ears |
| hives | wheezing |
| skin redness | trouble breathing |
| swelling of your face, lips, mouth, tongue, throat, hands, or feet | chest discomfort |
| sweating | fast heartbeat |
See “What are the important possible side effects of PEMGARDA?”for more information about side effects.
You are being given this Fact Sheet because your healthcare provider believes it is necessary to provide you or your child with PEMGARDA for pre-exposure prophylaxis to help prevent coronavirus disease 2019 (COVID‑19) caused by the SARS-CoV-2 virus.
This Fact Sheet contains information to help you understand the potential risks and the potential benefits of receiving PEMGARDA, which you, or your child, have received or may receive.
The United States (US) Food and Drug Administration (FDA) has issued an Emergency Use Authorization (EUA) to make PEMGARDA available during the COVID-19 pandemic (for more details about an EUA please see “ What is an Emergency Use Authorization (EUA)?” at the end of this document). PEMGARDA is not an FDA-approved medicine in the US.
Read this Fact Sheet for information about PEMGARDA. Talk to your healthcare provider about your options or if you have any questions. It is your choice for you or your child to receive PEMGARDA or stop at any time.
What is COVID-19?
COVID-19 is caused by a virus called a coronavirus (SARS-CoV-2). You can get COVID-19 through contact with another person who has the virus.
COVID-19 illnesses have ranged from very mild (including some with no reported symptoms) to severe, including illness resulting in death. While information so far suggests that most COVID‑19 illnesses are mild, serious illness can happen and may cause some of your other medical conditions to become worse. Older people and people of all ages with severe, long lasting (chronic) medical conditions like immune compromise, heart disease, lung disease, diabetes, and obesity, for example, seem to be at higher risk of being hospitalized for COVID‑19.
What is PEMGARDA?
PEMGARDA is an investigational medicine that is used for pre-exposure prophylaxis to help prevent COVID-19 in adults and children 12 years of age and older who weigh at least 88 pounds (40 kg) who:
- are notcurrently infected with SARS-CoV-2 and who have notbeen known to be exposed to someone who is infected with SARS-CoV-2 and
- have moderate-to-severe immune compromise because of a medical condition or because they receive medicines or treatments that suppress the immune system andthey are unlikely to have an adequate response to COVID-19 vaccination.
PEMGARDA is investigational because it is still being studied. There is limited information about the safety and effectiveness of using PEMGARDA for prevention of COVID-19. The FDA has authorized the emergency use of PEMGARDA for pre-exposure prophylaxis to help prevent COVID-19 under an EUA. For more information on EUA, see the “What is an Emergency Use Authorization (EUA)?” section at the end of this Fact Sheet.
PEMGARDA is notauthorized:
- to treat COVID-19
- to prevent COVID-19 after being around someone infected with SARS-CoV-2 (post-exposure prophylaxis)
- when PEMGARDA is not expected to work against more than 90% of the SARS- CoV-2 variants in the US. Viruses can change over time (mutate) and develop into a slightly different form of the virus, called a variant.
- for use in children under 12 years of age or weighing less than 88 pounds (40 kg)
Pre-exposure prophylaxis to help prevent COVID-19 with PEMGARDA does not take the place of receiving COVID-19 vaccination in people who can be vaccinated for COVID-19. If your health care provider recommends it, you should receive a COVID-19 vaccination.
If you have received a COVID-19 vaccine, you should wait at least 2 weeks after vaccination to receive PEMGARDA.
What should I tell my healthcare provider before I receive PEMGARDA?
Tell your healthcare provider about all of your medical conditions, including if you:
- have any allergies, including if you have had a severe allergic reaction to a COVID‑19 vaccine or to PEMGARDA.
- are pregnant or plan to become pregnant. It is not known if PEMGARDA can harm your unborn baby.
- are breastfeeding or plan to breastfeed. It is not known if PEMGARDA can pass into your breast milk. Talk to your healthcare provider about the best way to feed your baby if you receive PEMGARDA.
- have any serious illnesses.
- take any medicines including prescription, over-the-counter, vitamins, and herbal products.
How will I receive PEMGARDA?
- You will receive 1 dose of PEMGARDA.
- PEMGARDA will be given to you through an infusion in a vein (intravenous [IV] infusion). It will take about 60 minutes to finish the infusion.
- You will receive PEMGARDA in a healthcare setting.
- You will be observed by a healthcare provider during your infusion and for at least 2 hours after your infusion is finished.
You may need to receive additional doses of PEMGARDA for ongoing protection from COVID-19. Viruses can change over time (mutate) and develop into a slightly different form of the virus, called a variant. Based on what we know about current SARS-CoV-2 variants, you may need to receive additional doses of PEMGARDA every 3 months.
Who should generally not take PEMGARDA?
Do not take PEMGARDA if you have had a severe allergic reaction to PEMGARDA or any ingredient in PEMGARDA. See the end of this Fact Sheet for a complete list of ingredients in PEMGARDA.
What are the important possible side effects of PEMGARDA?
- See “ What is the most important information I should know about PEMGARDA?”
- Allergic and infusion-related reactions.Allergic and infusion-related reactions are common and can sometimes be severe or life-threatening. Allergic and infusion-related reactions can happen during and after your infusion of PEMGARDA. You may have an increased risk of allergic reaction with PEMGARDA if you have had a severe allergic reaction to a COVID‑19 vaccine. PEMGARDA contains polysorbate 80, an ingredient in some COVID‑19 vaccines. Also, polysorbate 80 is similar to polyethylene glycol (PEG), an ingredient in other COVID‑19 vaccines. Your healthcare provider may consult with a healthcare provider who specializes in allergy and immunology before giving you PEMGARDA if you have had a serious allergic reaction to a COVID-19 vaccine. Your healthcare provider will monitor you for allergic reactions during the infusion and for at least 2 hours after you receive PEMGARDA. Tell your healthcare provider right away if you get any of the following signs or symptoms of an allergic or infusion-related reaction during or after your infusion of PEMGARDA:
| fever | headache |
| trouble breathing or shortness of breath | throat tightness or irritation |
| chills | high or low blood pressure |
| tiredness | swelling of your face, lips, mouth, tongue, throat, hands, or feet |
| fast or slow heart rate | rash, including hives |
| chest pain or discomfort | itching |
| weakness | muscle aches |
| confusion | feeling lightheaded, faint, or dizzy |
| nausea | sweating |
The side effects of receiving any medicine by vein (IV) may include pain, redness, bleeding, bruising of the skin, soreness, swelling, and possible infection at the infusion site.
The most common side effects in people treated with PEMGARDAwho have moderate-to-severe immune compromise include allergic and infusion-related reactions, infusion site reactions, common cold, viral infection, flu-like illness, tiredness, headache and nausea.
These are not all the possible side effects of PEMGARDA. Not a lot of people have been given PEMGARDA. Serious and unexpected side effects may happen. PEMGARDA is still being studied, so it is possible that all of the risks are not known at this time.
What other important information do I need to know when receiving PEMGARDA?
Risk of COVID-19 caused by certain SARS-CoV-2 variants:Viruses can change over time (mutate) and develop into a slightly different form of the virus, called a variant. PEMGARDA may not prevent COVID-19 caused by certain SARS‑CoV-2 variants. If you are exposed to these variants, your chance of developing COVID-19 is higher than from other variants. Tell your healthcare provider right away, and test for COVID-19, if you develop any symptoms of COVID-19, including:
| fever or chills | headache |
| cough | sore throat |
| shortness of breath or difficulty breathing | new loss of taste or smell |
| congestion or runny nose | feeling tired (fatigue) |
| nausea or vomiting | muscle or body aches |
| diarrhea |
For more information about the symptoms of COVID-19, go to https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html.
If you develop COVID-19, your healthcare provider may recommend one of the available COVID-19 treatments.
What other prevention choices are there?
Vaccines to help prevent COVID-19 are approved or available under Emergency Use Authorization. Use of PEMGARDA does not replace vaccination against COVID-19. For more information about other medicines authorized for treatment or prevention of COVID-19, go to https://www.fda.gov/emergency-preparedness-and-response/mcm- legal-regulatory-and-policy-framework/emergency-use-authorization#coviddrugs.
It is your choice to receive or not receive PEMGARDA for pre-exposure prophylaxis to help prevent COVID-19. Should you decide not to receive PEMGARDA, it will not change your standard medical care.
PEMGARDA is not authorized to treat COVID-19 or for post-exposure prophylaxis of COVID-19.
What if I am pregnant or breastfeeding?
There is no experience using PEMGARDA in women who are pregnant or breastfeeding. For a mother and unborn baby, the benefit of receiving PEMGARDA may be greater than the risk of using the product. If you are pregnant or breastfeeding, discuss your options and specific situation with your healthcare provider.
How do I report side effects with PEMGARDA?
Tell your healthcare provider right away if you have any side effect that bothers you or does not go away. Report side effects to FDA MedWatch at www.fda.gov/medwatch, or call 1‑800‑FDA‑1088, or call Invivyd at 1-800-890-3385.
How can I learn more about PEMGARDA?
If you have questions, visit the website, or call the telephone number provided below. To access the most recent PEMGARDA Fact Sheet, please scan the QR code provided below.
| Website | Telephone Number |
| www.Pemgarda.com | 1-800-890-3385 |
How can I learn more about COVID-19?
- Ask your healthcare provider.
- Visit https://www.cdc.gov/COVID19.
- Contact your local or state public health department.
What is an Emergency Use Authorization?
The United States FDA has made PEMGARDA available under an emergency access mechanism called an Emergency Use Authorization (EUA). The EUA is supported by a Secretary of Health and Human Services (HHS) declaration under the Federal Food, Drug, and Cosmetic Act that circumstances exist to justify the emergency use of drugs and biological products during the COVID-19 pandemic.
PEMGARDA for pre-exposure prophylaxis to help prevent COVID-19 has not undergone the same type of review as an FDA-approved product. In issuing an EUA the FDA has determined, among other things, that based on the total amount of scientific evidence available, including data from adequate and well-controlled clinical trials, it is reasonable to believe that the product may be effective for preventing COVID‑-19, or a serious or life-threatening disease or condition caused by COVID-19; that the known and potential benefits of the product, when used to prevent such disease or condition, outweigh the known and potential risks of such product; and that there are no adequate, approved, and available alternatives.
All of these criteria must be met to allow the product to be used during the COVID-19 pandemic. The EUA for PEMGARDA is in effect for the duration of the COVID-19 HHS declaration justifying emergency use of PEMGARDA, unless terminated or revoked (after which PEMGARDA may no longer be used under the EUA).
What are the ingredients in PEMGARDA?
Active ingredient: pemivibart
Inactive ingredients: glycine, L-arginine hydrochloride, L-histidine, L-histidine hydrochloride monohydrate, L-methionine, polysorbate 80, and sterile water for injection.
Manufactured and distributed by: Invivyd, Inc., 1601 Trapelo Road, Suite 178, Waltham, MA 02451
INVIVYD™, PEMGARDA™, and the Ribbon logos are trademarks of Invivyd, Inc.
©2024 Invivyd, Inc. All rights reserved.
Revised: August 2024
Emergency Use Authorization (EUA) of PEMGARDA (pemivibart) for Coronavirus Disease 2019 (COVID-19)
PRINCIPAL DISPLAY PANEL - 500 MG/4 ML CARTON
NDC 81960-031-03
Rx-Only
PEMGARDA
(pemivibart) injection
500 mg/4 mL (125 mg/mL)
For use under Emergency Use Authorization (EUA).
For Intravenous Infusion only.
Refer to the FDA-authorized Fact Sheet for detailed instructions on dosage and administration.
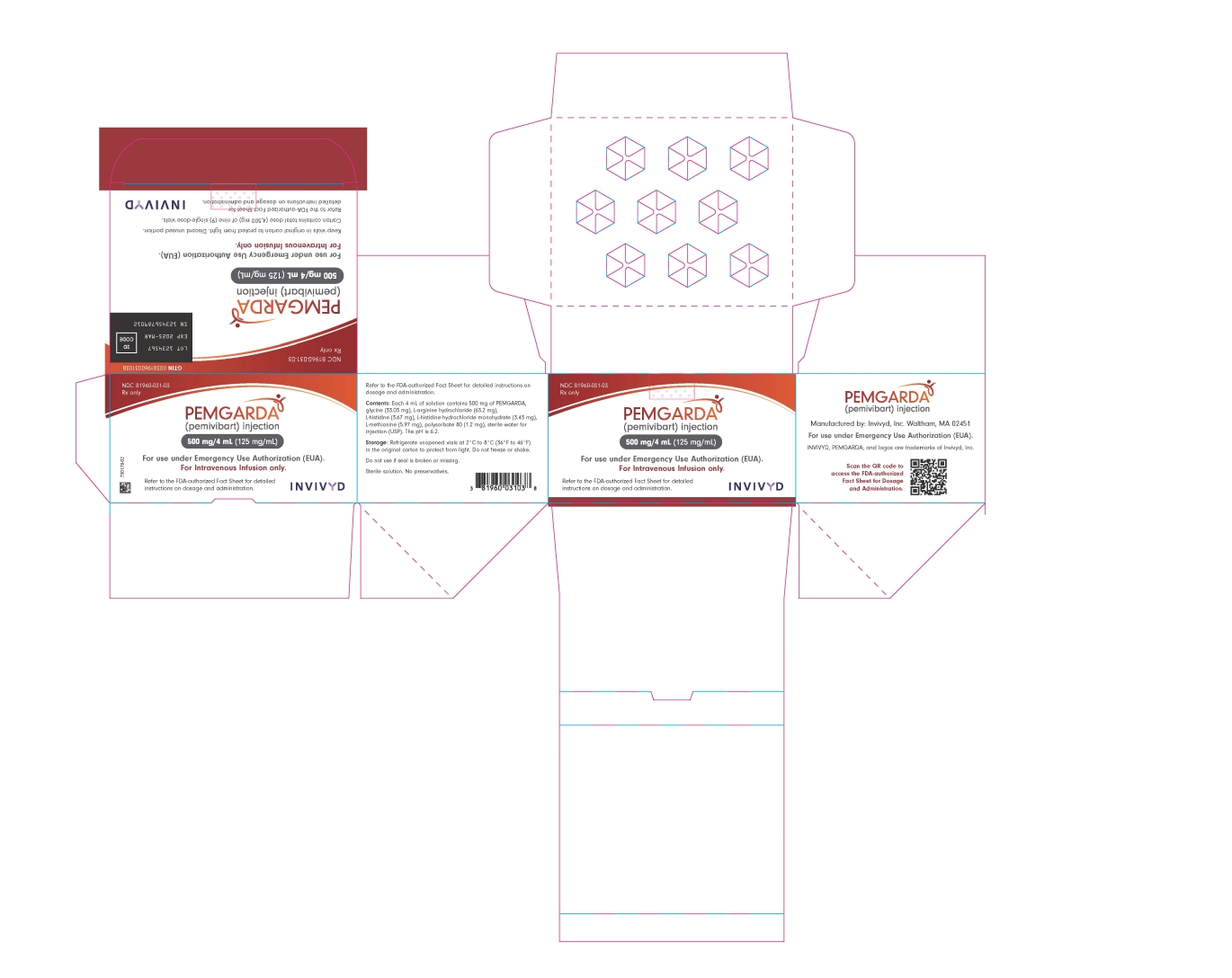
| PEMGARDA
pemivibart injection |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Invivyd, Inc (117621026) |
| Registrant - Invivyd, Inc (117621026) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| PCI Pharma Services | 053217022 | pack(81960-031) , label(81960-031) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| WuXi Biologics Co., Ltd | 421298354 | analysis(81960-031) , api manufacture(81960-031) | |
More about Pemgarda (pemivibart)
- Check interactions
- Compare alternatives
- Pricing & coupons
- Drug images
- Side effects
- Dosage information
- FDA approval history
- Drug class: miscellaneous antivirals
- Breastfeeding
- En español

