Nuvaxovid: Package Insert / Prescribing Info
Package insert / product label
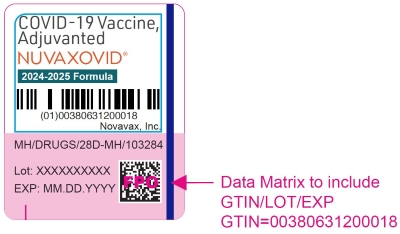
Generic name: Covid-19 vaccine
Dosage form: intramuscular injectable suspension
Drug class: Viral vaccines
Medically reviewed by Drugs.com. Last updated on Sep 10, 2025.
On This Page
- Indications and Usage
- Dosage and Administration
- Dosage Forms and Strengths
- Contraindications
- Warnings and Precautions
- Adverse Reactions/Side Effects
- Use In Specific Populations
- Description
- Clinical Pharmacology
- Nonclinical Toxicology
- Clinical Studies
- How Supplied/Storage and Handling
- Patient Counseling Information
Highlights of Prescribing Information
NUVAXOVIDTM (COVID-19 Vaccine, Adjuvanted) injectable suspension, for intramuscular use
2025-2026 Formula
Initial U.S. Approval: 2025
Indications and Usage for Nuvaxovid
NUVAXOVID is a vaccine indicated for active immunization to prevent coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
NUVAXOVID is approved for use in individuals who are:
- 65 years of age and older, or
- 12 years through 64 years of age with at least one underlying condition that puts them at high risk for severe outcomes from COVID-19. (1)
Nuvaxovid Dosage and Administration
Dosage Forms and Strengths
NUVAXOVID is an injectable suspension. A single dose is 0.5 mL. (3)
Contraindications
Do not administer NUVAXOVID to individuals with a known history of severe allergic reaction (e.g., anaphylaxis) to any component of NUVAXOVID or to individuals who had a severe allergic reaction (e.g., anaphylaxis) following a previous dose of a Novavax COVID-19 Vaccine, Adjuvanted. (4)
Warnings and Precautions
Clinical trials data provide evidence for increased risks of myocarditis and pericarditis following administration of NUVAXOVID. There have been postmarketing reports of myocarditis and pericarditis following administration of Novavax COVID-19 Vaccine, Adjuvanted. (5.2)
Adverse Reactions/Side Effects
The most commonly reported (> 10%) solicited adverse reactions after vaccination were:
- Participants 12 years through 17 years of age: injection site tenderness (up to 65.2%), injection site pain (up to 61%), headache (up to 56.9%), fatigue (up to 49.9%), muscle pain (up to 49.1%), malaise (up to 40.2%), nausea/vomiting (up to 19.9%), fever (up to 16.9%), and joint pain (up to 16.1%) (6.1)
- Participants 18 years through 64 years of age: injection site tenderness (up to 71.7%), injection site pain (up to 58.6%), muscle pain (up to 52.7%), fatigue (up to 50.5%), headache (up to 47.4%), malaise (up to 38.9%), joint pain (up to 22.2%), and nausea/vomiting (up to 12.1%) (6.1)
- Participants 65 years of age and older: injection site tenderness (up to 52.9%), injection site pain (up to 40.1%), fatigue (up to 29.2%), muscle pain (up to 29.2%), headache (up to 24.9%), malaise (up to 21.2%), and joint pain (up to 12.7%) (6.1)
- Participants 12 years through 17 years of age receiving a booster dose: injection site tenderness (65.9%), injection site pain (64.6%), headache (62.9%), muscle pain (60.4%), fatigue (57.1%), malaise (45.1%), nausea/vomiting (23.6%), joint pain (21.9%), fever (16.8%), and injection site redness (10.3%) (6.1)
- Participants 18 years of age and older receiving a booster dose: injection site tenderness (67.2%), injection site pain (56.4%), muscle pain (51.1%), fatigue (49.9%), headache (44.3%), malaise (37.7%), joint pain (24.2%), and nausea/vomiting (11.6%) (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Novavax, Inc. at 1-844-668-2829 or VAERS at 1-800-822-7967 or https://vaers.hhs.gov.
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 8/2025
Full Prescribing Information
1. Indications and Usage for Nuvaxovid
NUVAXOVID is a vaccine indicated for active immunization to prevent coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
NUVAXOVID is approved for use in individuals who are:
- 65 years of age and older, or
- 12 years through 64 years of age with at least one underlying condition that puts them at high risk for severe outcomes from COVID-19.
2. Nuvaxovid Dosage and Administration
For intramuscular use.
2.1 Dose and Schedule
Administer NUVAXOVID as a single 0.5 mL dose.
For individuals previously vaccinated with any COVID-19 vaccine, administer the dose of NUVAXOVID at least 2 months after the last dose of COVID-19 vaccine.
2.2 Preparation for Administration
- Verify that the label on the pre-filled syringe states 2025-2026 Formula.
- NUVAXOVID is a colorless to slightly yellow, clear to mildly opalescent suspension.
- Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. Do not administer the vaccine if either of these conditions exist.
4. Contraindications
Do not administer NUVAXOVID to individuals with a known history of severe allergic reaction (e.g., anaphylaxis) to any component of NUVAXOVID [see Description (11)] or to individuals who had a severe allergic reaction (e.g., anaphylaxis) following a previous dose of Novavax COVID-19 Vaccine, Adjuvanted.
5. Warnings and Precautions
5.1 Management of Acute Allergic Reactions
Appropriate medical treatment must be immediately available to manage potential anaphylactic reactions following administration of NUVAXOVID.
5.2 Myocarditis and Pericarditis
Clinical trials data provide evidence for increased risks of myocarditis and pericarditis following administration of NUVAXOVID. There have been postmarketing reports of myocarditis and pericarditis following administration of Novavax COVID-19 Vaccine, Adjuvanted [see Adverse Reactions (6)].
The Centers for Disease Control and Prevention (CDC) has published considerations related to myocarditis and pericarditis after vaccination, including for vaccination of individuals with a history of myocarditis or pericarditis (https://www.cdc.gov/vaccines/covid-19/clinical-considerations/myocarditis.html).
5.3 Syncope
Syncope (fainting) may occur in association with administration of injectable vaccines, including NUVAXOVID. Procedures should be in place to avoid injury from fainting.
5.4 Altered Immunocompetence
Immunocompromised persons, including individuals receiving immunosuppressive therapy, may have a diminished immune response to NUVAXOVID [see Use in Specific Populations (8.6)].
6. Adverse Reactions/Side Effects
An overview of clinical studies contributing to the safety assessment of NUVAXOVID in individuals 12 years of age and older is provided in Table 1. Participants in these clinical studies received a single dose, a 2-dose initial series (two doses 21 days apart; referred to as a primary series) and subsequent doses (referred to as booster doses) with Novavax COVID-19 Vaccine, Adjuvanted or with another COVID-19 vaccine manufactured by Novavax Inc.
| Study | Age | Vaccine Composition | Dosing Regimens | Vaccine Recipientsa |
|---|---|---|---|---|
|
Abbreviation: SARS-CoV-2 = severe acute respiratory syndrome coronavirus 2. |
||||
| Study 1 (NCT04611802) | 18 years of age and older | Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent)b | Primary Series | 26,106 |
| Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent)b | 1st Booster | 13,353c,d | ||
| 12 years through 17 years of age | Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent)b | Primary Series | 2,153 | |
| Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent)b | 1st Booster | 1,499c | ||
| Study 2 (NCT04583995) | 18 years through 84 years of age | Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent)b | Primary Series | 10,795 |
| Study 3 (NCT04533399) | 18 years through 84 years of age | Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent)b | Primary Series | 4,104 |
| Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent)b | 1st Booster | 1,898c | ||
| Study 4 (NCT04368988) | 18 years through 59 years of age (Part 1) | Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent)b | Primary Series | 29 |
| 18 years through 84 years of age (Part 2) | Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent)b | Primary Series | 514 | |
| Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent)b | 1st Booster | 105c | ||
| Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent)b | 2nd Booster | 45c | ||
| Study 5 (NCT05463068) | 18 years through 49 years of age | Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent)b | 1st or 2nd Booster | 905 |
| Study 6 (NCT05372588) | 18 years through 64 years of age (Part 1) | Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent)b | 2nd Booster | 274e |
| Monovalent Vaccine (Omicron BA.1)f | 2nd Booster | 286e | ||
| Bivalent Vaccine (Original monovalent and Omicron BA.1)g | 2nd Booster | 269e | ||
| 18 years of age and older (Part 2) | Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent)b | 2nd Booster | 251e | |
| Monovalent Vaccine (Omicron BA.5)h | 2nd Booster | 254e | ||
| Bivalent Vaccine (Original monovalent and Omicron BA.5)i | 2nd Booster | 259e | ||
| Study 7 (NCT05975060) | 18 years of age and older (Part 2) | Novavax COVID-19 Vaccine, Adjuvanted (2023-2024 Formula)j | Single Dose | 338 |
Safety data accrued in Studies 1, 5, 6, and 7 are relevant to NUVAXOVID because the vaccines administered in these studies were manufactured by the same manufacturing process as NUVAXOVID. Studies 2, 3 and 4, which utilized vaccines manufactured by a different process than NUVAXOVID, are considered supportive safety studies.
Adults 18 Years of Age and Older
2-Dose Series (Original Monovalent) in Vaccine-Naïve Adults
In participants 18 through 64 years of age, the most commonly reported (> 10%) solicited adverse reactions following administration of any dose of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) were injection site tenderness (76.5%), injection site pain (64.3%), muscle pain (57.4%), fatigue (56.4%), headache (54.6%), malaise (43.2%), joint pain (25.1%), and nausea/vomiting (16.4%).
In participants 65 years of age and older, the most commonly reported (> 10%) solicited adverse reactions following administration of any dose of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) were injection site tenderness (57.8%), injection site pain (44.1%), fatigue (36.3%), muscle pain (33.8%), headache (31.3%), malaise (24.3%), and joint pain (15.5%).
Single Dose (Original Monovalent) in Vaccine-Experienced Adults
In participants 18 through 64 years of age, the most commonly reported (> 10%) solicited adverse reactions following administration of a booster dose of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) were injection site tenderness (69.4%), injection site pain (58.8%), muscle pain (54.3%), fatigue (52.5%), headache (47.3%), malaise (40.2%), joint pain (25.7%), and nausea/vomiting (12.5%).
In participants 65 years of age and older, the most commonly reported (> 10%) solicited adverse reactions following administration of a booster dose of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) were injection site tenderness (54.4%), injection site pain (41.7%), muscle pain (32.1%), fatigue (34.2%), headache (26.1%), malaise (22.5%), and joint pain (14.9%).
Adolescents 12 Years of Age Through 17 Years of Age
2-Dose Series (Original Monovalent) in Vaccine-Naïve Adolescents
In participants 12 through 17 years of age, the most commonly reported (> 10%) solicited adverse reactions following administration of any dose of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) were injection site tenderness (71.3%), injection site pain (67.1%), headache (63.3%), muscle pain (56.9%), fatigue (54.0%), malaise (43.0%), nausea/vomiting (23.1%), joint pain (19.4%), and fever (16.5%).
Single Dose (Original Monovalent) in Vaccine-Experienced Adolescents
In participants 12 through 17 years of age, the most commonly reported (> 10%) solicited adverse reactions following administration of a booster dose of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) were injection site tenderness (65.9%), injection site pain (64.6%), headache (62.9%), muscle pain (60.4%), fatigue (57.1%), malaise (45.1%), nausea/vomiting (23.6%), joint pain (21.9%), fever (16.8%), and injection site redness (10.3%).
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a vaccine cannot be directly compared with rates in the clinical trials of another vaccine and may not reflect the rates observed in practice.
Adults 18 Years of Age and Older
2-Dose Series (Original Monovalent) in Vaccine-Naïve Adults
Safety of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) was assessed in a clinical study conducted in the United States (US) and Mexico (NCT04611802; Study 1). In this study, 26,106 participants 18 years of age and older received at least one primary series dose of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent). Additional supportive safety data are available from three other clinical trials in the United Kingdom (NCT04583995; Study 2), South Africa (NCT04533399; Study 3), and Australia (NCT04368988, Part 1 and Part 2 in Australia and the US; Study 4) which evaluated a COVID-19 vaccine containing the SARS-CoV-2 recombinant spike (rS) protein and Matrix-M® adjuvant but manufactured by a different process than Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent).
Study 1 was a Phase 3, multicenter, randomized (2:1), observer-blinded, placebo-controlled, crossover study in adult participants 18 years of age and older in the US and Mexico. Participants were randomized (2:1) to receive 2 doses of the vaccine or placebo administered 21 days apart.
In the adult part of Study 1, participants received Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) (n=19,735) or placebo (n=9,847) in the pre-crossover period. In the pre-crossover period, among participants who received at least one dose of vaccine, 52.5% were male, 47.5% were female; 75.0% were White, 11.8% were Black or African American, 4.1% were Asian, 6.6% were American Indian (including Native Americans) or Alaskan Native, and 1.7% were multiple races; 22.0% were Hispanic/Latino. Demographic characteristics of participants were similar between the Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) and placebo groups. During the study, COVID-19 vaccines authorized for emergency use became available, and participants, when eligible for vaccination, were offered the opportunity to cross over from the originally assigned study treatment to the other study treatment (vaccine or placebo) in a blinded fashion (“blinded crossover”). Due to data quality issues at two study sites, a total of 289 participants were excluded from the safety analysis set. In the post-crossover period, 6,416 participants who had initially received placebo and subsequently received Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) [referred to as Placebo/Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent)]; and 15,298 participants who had initially received Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) and subsequently received placebo [referred to as Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent)/Placebo]. The demographic characteristics were similar between participants in the pre-crossover and post-crossover groups.
Solicited Adverse Reactions
During the pre-crossover period, local and systemic adverse reactions were solicited within 7 days following each dose of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) or placebo in participants using an electronic diary.
The reported frequency and severity of solicited local and systemic adverse reactions in participants 18 through 64 years of age are presented in Table 2.
| Event | Novavax COVID-19 Vaccine, Adjuvanted (Original Monovalent) | Placebod | ||
|---|---|---|---|---|
| Dose 1 N=16,041 n (%) | Dose 2 N=16,106 n (%) | Dose 1 N=7,968 n (%) | Dose 2 N=7,859 n (%) |
|
|
a Solicited reactogenicity events and use of antipyretic or pain medication were collected by the participant in the electronic diary (eDiary). |
||||
| Local Adverse Reactionse | ||||
| Tendernessf | ||||
| Any Grade | 8,796 (54.8) | 11,543 (71.7) | 1,379 (17.3) | 1,221 (15.5) |
| Grade 3 | 146 (0.9) | 811 (5.0) | 16 (0.2) | 17 (0.2) |
| Grade 4 | 0 | 2 (< 0.1) | 0 | 0 |
| Paing | ||||
| Any Grade | 5,816 (36.3) | 9,436 (58.6) | 921 (11.6) | 1,041 (13.2) |
| Grade 3 | 52 (0.3) | 287 (1.8) | 2 (< 0.1) | 6 (< 0.1) |
| Grade 4 | 0 | 1 (< 0.1) | 0 | 0 |
| Redness (erythema)h | ||||
| Any Grade | 148 (0.9) | 1,039 (6.5) | 23 (0.3) | 26 (0.3) |
| Grade 3 | 2 (< 0.1) | 119 (0.7) | 0 | 2 (< 0.1) |
| Swellingi | ||||
| Any Grade | 136 (0.8) | 945 (5.9) | 23 (0.3) | 22 (0.3) |
| Grade 3 | 4 (< 0.1) | 67 (0.4) | 1 (< 0.1) | 1 (< 0.1) |
| Systemic Adverse Reactionse | ||||
| Fatiguej | ||||
| Any Grade | 4,343 (27.1) | 8,133 (50.5) | 1,894 (23.8) | 1,723 (21.9) |
| Grade 3 | 391 (2.4) | 2,522 (15.7) | 190 (2.4) | 307 (3.9) |
| Grade 4 | 3 (< 0.1) | 2 (< 0.1) | 1 (< 0.1) | 3 (< 0.1) |
| Headachek | ||||
| Any Grade | 4,292 (26.8) | 7,630 (47.4) | 1,942 (24.4) | 1,596 (20.3) |
| Grade 3 | 134 (0.8) | 500 (3.1) | 58 (0.7) | 36 (0.5) |
| Grade 4 | 4 (< 0.1) | 2 (< 0.1) | 1 (< 0.1) | 2 (< 0.1) |
| Muscle pain (myalgia)j | ||||
| Any Grade | 3,949 (24.6) | 8,490 (52.7) | 1,142 (14.3) | 1,010 (12.9) |
| Grade 3 | 79 (0.5) | 818 (5.1) | 31 (0.4) | 28 (0.4) |
| Grade 4 | 2 (< 0.1) | 2 (< 0.1) | 1 (< 0.1) | 4 (< 0.1) |
| Malaisej | ||||
| Any Grade | 2,460 (15.3) | 6,273 (38.9) | 963 (12.1) | 943 (12.0) |
| Grade 3 | 126 (0.8) | 1,043 (6.5) | 52 (0.7) | 54 (0.7) |
| Grade 4 | 6 (< 0.1) | 5 (< 0.1) | 1 (< 0.1) | 2 (< 0.1) |
| Joint pain (arthralgia)j | ||||
| Any Grade | 1,272 (7.9) | 3,574 (22.2) | 528 (6.6) | 514 (6.5) |
| Grade 3 | 49 (0.3) | 403 (2.5) | 25 (0.3) | 22 (0.3) |
| Grade 4 | 1 (< 0.1) | 2 (< 0.1) | 0 | 2 (< 0.1) |
| Nausea or vomitingl | ||||
| Any Grade | 1,150 (7.2) | 1,953 (12.1) | 513 (6.4) | 443 (5.6) |
| Grade 3 | 18 (0.1) | 29 (0.2) | 7 (< 0.1) | 7 (< 0.1) |
| Grade 4 | 4 (< 0.1) | 5 (< 0.1) | 2 (< 0.1) | 2 (< 0.1) |
| Feverm | ||||
| Any Grade | 61 (0.4) | 1,062 (6.6) | 31 (0.4) | 22 (0.3) |
| Grade 3 | 8 (< 0.1) | 79 (0.5) | 7 (< 0.1) | 5 (< 0.1) |
| Grade 4 | 7 (< 0.1) | 2 (< 0.1) | 1 (< 0.1) | 2 (< 0.1) |
The reported frequency and severity of solicited local and systemic adverse reactions are presented for participants 65 years of age and older in Table 3.
| Event | Novavax COVID-19 Vaccine, Adjuvanted (Original Monovalent) | Placebod | ||
|---|---|---|---|---|
| Dose 1 N=2,293 n (%) | Dose 2 N=2,217 n (%) | Dose 1 N=1,138 n (%) | Dose 2 N=1,057 n (%) |
|
| a Solicited reactogenicity events and use of antipyretic or pain medication were collected by the participant in the electronic diary (eDiary). b 7 days included day of vaccination and the subsequent 6 days. c The analysis included 2,293 (Dose 1) and 2,217 (Dose 2) participants in the Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) group and 1,138 (Dose 1) and 1,057 (Dose 2) participants in the placebo group who received at least one dose and completed at least one day of the vaccination reactogenicity diary, reported an unsolicited adverse event that was mapped to a reactogenicity term within 7 days of the dose, reported a symptom in the Daily Illness Symptoms Diary that was mapped to a reactogenicity term within 7 days of the dose, or reported a temperature in the Daily Illness Symptoms Diary within 7 days of the dose. d Placebo was a saline solution. e Absence of rows for Grade 4 adverse reactions indicates no events were reported. f Any Grade = any event that is ≥ Grade 1, where Grade 1 = Mild discomfort to touch; Grade 2 = Discomfort with movement; Grade 3 = Significant discomfort at rest; Grade 4 = Emergency room (ER) visit or hospitalization. g Any Grade = any event that is ≥ Grade 1, where Grade 1 = Does not interfere with activity; Grade 2 = Repeated use of non-narcotic pain reliever > 24 hours or interferes with activity; Grade 3 = Any use of narcotic pain reliever or prevents daily activity; Grade 4 = ER visit or hospitalization. h Any Grade = any event that is ≥ Grade 1, where Grade 1 = 2.5 – 5 cm; Grade 2 = 5.1 – 10 cm; Grade 3 = > 10 cm; Grade 4 = Necrosis or exfoliative dermatitis. i Any Grade = any event that is ≥ Grade 1, where Grade 1 = 2.5 – 5 cm and does not interfere with activity; Grade 2 = 5.1 – 10 cm or interferes with activity; Grade 3 = > 10 cm or prevents daily activity; Grade 4 = Necrosis. j Any Grade = any event that is ≥ Grade 1, where Grade 1 = No interference with activity; Grade 2 = Some interference with activity; Grade 3 = Significant; prevents daily activity; Grade 4 = ER visit or hospitalization. k Any Grade = any event that is ≥ Grade 1, where Grade 1 = No interference with activity; Grade 2 = Repeated use of non-narcotic pain reliever > 24 hours or some interference with activity; Grade 3 = Significant; any use of narcotic pain reliever or prevents daily activity; Grade 4 = ER visit or hospitalization. l Any Grade = any event that is ≥ Grade 1, where Grade 1 = No interference with activity or 1 – 2 episodes/24 hours; Grade 2 = Some interference with activity or > 2 episodes/24 hours; Grade 3 = Prevents daily activity, requires outpatient IV hydration; Grade 4 = ER visit or hospitalization for hypotensive shock. m Any Grade = any event that is ≥ Grade 1, where Grade 1 = 38.0 – 38.4°C (100.4 – 101.1°F); Grade 2 = 38.5 – 38.9°C (101.2 – 102.0°F); Grade 3 = 39.0 – 40°C (102.1 – 104°F); Grade 4 = > 40°C (> 104°F). |
||||
| Local Adverse Reactionse | ||||
| Tendernessf | ||||
| Any Grade | 772 (33.7) | 1,173 (52.9) | 148 (13.0) | 108 (10.2) |
| Grade 3 | 10 (0.4) | 33 (1.5) | 2 (0.2) | 1 (< 0.1) |
| Paing | ||||
| Any Grade | 461 (20.1) | 890 (40.1) | 93 (8.2) | 114 (10.8) |
| Grade 3 | 3 (0.1) | 14 (0.6) | 1 (< 0.1) | 1 (< 0.1) |
| Redness (erythema)h | ||||
| Any Grade | 17 (0.7) | 103 (4.6) | 5 (0.4) | 4 (0.4) |
| Grade 3 | 0 | 7 (0.3) | 0 | 0 |
| Swellingi | ||||
| Any Grade | 17 (0.7) | 116 (5.2) | 2 (0.2) | 4 (0.4) |
| Grade 3 | 0 | 5 (0.2) | 0 | 0 |
| Systemic Adverse Reactionse | ||||
| Fatiguej | ||||
| Any Grade | 431 (18.8) | 647 (29.2) | 196 (17.2) | 163 (15.4) |
| Grade 3 | 73 (3.2) | 138 (6.2) | 27 (2.4) | 34 (3.2) |
| Headachek | ||||
| Any Grade | 382 (16.7) | 551 (24.9) | 199 (17.5) | 161 (15.2) |
| Grade 3 | 12 (0.5) | 18 (0.8) | 4 (0.4) | 2 (0.2) |
| Grade 4 | 0 | 1 (< 0.1) | 0 | 0 |
| Muscle pain (myalgia)j | ||||
| Any Grade | 324 (14.1) | 648 (29.2) | 144 (12.7) | 115 (10.9) |
| Grade 3 | 3 (0.1) | 32 (1.4) | 4 (0.4) | 2 (0.2) |
| Malaisej | ||||
| Any Grade | 230 (10.0) | 469 (21.2) | 100 (8.8) | 95 (9.0) |
| Grade 3 | 12 (0.5) | 40 (1.8) | 4 (0.4) | 5 (0.5) |
| Joint pain (arthralgia)j | ||||
| Any Grade | 141 (6.1) | 282 (12.7) | 72 (6.3) | 63 (6.0) |
| Grade 3 | 4 (0.2) | 16 (0.7) | 4 (0.4) | 2 (0.2) |
| Nausea/vomitingl | ||||
| Any Grade | 120 (5.2) | 132 (6.0) | 47 (4.1) | 39 (3.7) |
| Grade 3 | 0 | 2 (< 0.1) | 0 | 0 |
| Feverm | ||||
| Any Grade | 9 (0.4) | 45 (2.0) | 6 (0.5) | 7 (0.7) |
| Grade 3 | 1 (< 0.1) | 2 (< 0.1) | 0 | 1 (< 0.1) |
| Grade 4 | 0 | 0 | 2 (0.2) | 0 |
Unsolicited Adverse Events
In Study 1, participants were monitored for unsolicited adverse events from the first dose through 28 days after the second dose in both the pre- and post-crossover periods. Serious adverse events, adverse events of special interest (AESI) and vaccine-related medically attended adverse events were recorded for the entirety of study participation. Participants who received at least one dose in the pre- or post-crossover periods were included in the safety analysis. In the pre-crossover period 19,735 participants received Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) and 9,847 participants received placebo. In the post-crossover period, 6,416 participants received Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) and 15,298 received placebo. Of participants who received two doses of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) in the pre-crossover period (n=19,075), 76% had a follow-up duration of at least 2 months (median = 2.5 months) after Dose 2. Of participants who received two doses of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) in the post-crossover period (n=6,306), 98% had a follow-up duration of at least 2 months (median = 8.3 months) after the last dose.
From Dose 1 through 28 days following Dose 2 in the pre-crossover period, the overall frequency of unsolicited adverse events was similar in the Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) group (11.8%) and the placebo group (11.0%). Unsolicited adverse events reported following any dose, through 28 days following Dose 2, not already captured by solicited local and systemic reactions, in the Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) group and placebo group included chills (0.3% vs < 0.1% pre-crossover and < 0.1% vs < 0.1% post-crossover), lymphadenopathy (0.2% vs 0.1% pre-crossover and 0.1% vs < 0.1% post-crossover) and injection site pruritus (0.1% vs 0.0% pre-crossover and 0.1% vs 0.0% post-crossover), respectively.
In the pre-crossover period, serious adverse events were reported by 228 (1.2%) participants in the Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) group and by 115 (1.2%) participants in the placebo group. In the post-crossover period, serious adverse events were reported by 164 (2.6%) participants who received Placebo/Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) and by 364 (2.4%) participants who received Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent)/Placebo.
Within 7 days of any dose (including 26,106 Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) recipients and 25,145 placebo recipients, of which 15,298 received Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) in the pre-crossover period, in both the pre- and post-crossover periods), hypersensitivity reactions (including urticaria, hypersensitivity, angioedema, and swelling of the face, lips, periorbital, and/or eyelids) were reported by 30 (0.11%) participants after Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) and 9 (0.04%) participants after placebo. Of these events, 1 reaction (generalized urticaria and facial angioedema with a duration of 2 days) was serious and occurred 2 days after Dose 1 of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent).
In Study 1, myocarditis and/or pericarditis were reported. A total of 3 events of myocarditis and/or pericarditis were reported by 2 (0.01%) participants after the Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) and a total of 2 events were reported in 2 participants (0.01%) after placebo (one of whom had received Novavax COVID-19 Vaccine, Adjuvanted [Original monovalent] 504 days prior to the event during the pre-crossover period). After Novavax COVID-19 Vaccine, Adjuvanted, one serious event was reported by a 67-year-old male 28 days after Dose 1, associated with concomitant COVID-19, and non-serious events of myocarditis and pericarditis (n=1 each) were reported by a 20-year-old male 10 days after Dose 1. Among the three reported events, one was reported as resolved and two did not have follow-up available. Reports of myocarditis and/or pericarditis from Study 1 and Study 2 (see Safety Data from Study 2) provide evidence for increased risks of myocarditis and pericarditis following administration of the Novavax COVID-19 Vaccine, Adjuvanted.
In the pre-crossover period of Study 1, atrial fibrillation was reported in 13 (0.07%) participants who received Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent), and 4 (0.04%) participants who received placebo (of which 10 (0.05%) participants in the Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) arm and 2 (0.02%) participants in the placebo arm experienced events that were serious). Of the total cases reported in the pre-crossover period, onset of atrial fibrillation within 30 days post vaccination occurred in 6 (0.03%) participants compared with 2 (0.02%) participants in the placebo group [of which 3 (0.02%) participants in the Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) arm and 0 participants in the placebo arm experienced events that were serious]. The currently available information on atrial fibrillation is insufficient to determine a causal relationship to the vaccine.
Within 28 days of any dose, the following numerical imbalances with more events in vaccine than placebo recipients [including 26,106 Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) recipients and 25,145 placebo recipients in both the pre- and post-crossover periods] were observed for the following serious and other adverse events of interest:
Within 28 days after vaccination throughout the study duration including after booster dose, events of cardiomyopathy, cardiac failure, congestive cardiomyopathy, congestive cardiac failure, acute cardiac failure, left ventricular failure, or acute left ventricular failure were reported. Ten events were reported by 10 (0.04%) participants after Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) was administered as a primary series (6 events) or booster dose (4 events), and 3 events were reported in 2 (0.01%) participants after placebo (one of whom had received Novavax COVID-19 Vaccine, Adjuvanted [Original monovalent] during the pre-crossover period). All events were serious except congestive cardiac failure (n=2), cardiomyopathy (n=2) and congestive cardiomyopathy (n=1) after Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent). Currently available information on cardiomyopathy or cardiac failure is insufficient to determine a causal relationship with the vaccine.
Within 28 days after vaccination in the pre- or post-crossover period, a total of 6 events of acute cholecystitis or cholecystitis were reported by 6 (0.02%) participants after Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) and a total of 2 events were reported by 2 (0.01%) participants after placebo (both of whom had received Novavax COVID-19 Vaccine, Adjuvanted [Original monovalent] during the pre-crossover period). All events were serious. Currently available information on acute cholecystitis or cholecystitis is insufficient to determine a causal relationship with the vaccine.
Within 28 days after vaccination in the pre- or post-crossover period, a total of 12 non-cardiac, non-neurovascular thrombotic and embolic events were reported by 11 (0.04%) participants after the Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) and a total of 7 events were reported by 6 (0.02%) participants after placebo (five of whom had received Novavax COVID-19 Vaccine, Adjuvanted [Original monovalent] during the pre-crossover period). Events following the Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) included pulmonary embolism (n=5), deep vein thrombosis (n=2), thrombosis (n=2), mesenteric artery thrombosis, peripheral arterial occlusive disease and portal vein thrombosis (n=1 each); six events were serious, including pulmonary embolism (n=5) and deep vein thrombosis (n=1). Events following placebo included pulmonary embolism (n=3), and deep vein thrombosis and peripheral arterial occlusive disease (n=2 each), all of which were serious except deep vein thrombosis and peripheral arterial occlusive disease (n=1 each). Currently available information on non-cardiac, non-neurovascular thrombotic and embolic events is insufficient to determine a causal relationship with the vaccine.
A total of 5 events of iridocyclitis, iritis or uveitis were reported by 3 (0.01%) participants after Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) and a total of 2 events were reported by 2 (0.01%) participants after placebo. All events were non-serious. One participant had onset of uveitis after Dose 1 of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) which resolved and then recurred following Dose 2. The two placebo recipients with events appeared to have had a previous history of uveitis and one of the Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) recipients had a history of iritis. Currently available information on iridocyclitis, iritis or uveitis is insufficient to determine a causal relationship with the vaccine.
Single Dose (Original Monovalent) in Vaccine-Experienced Adults
In an open-label portion of Study 1, 13,310 participants 18 years of age and older received a single booster dose of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) (0.5 mL) at least 6 months after the two-dose primary series (median of 11.0 months between completion of primary series and booster dose); an additional 43 participants received the booster dose after receiving only one dose in the two-dose primary series. Safety analyses included evaluation of solicited local and systemic adverse reactions within 7 days after a booster dose for participants who completed the electronic diary (n=11,447) and unsolicited adverse events within 28 days after a booster dose (n=13,353). Safety analyses also included evaluation of serious adverse events and adverse events of special interest after a booster dose (n=13,353) with a median follow-up of 6.7 months (0 – 8 months).
Among the 13,353 boosted participants, 84.5% were between 18 and 64 years of age and 15.5% were 65 years of age and older, 50.6% were male, 49.4% were female; 71.8% were White, 14.1% were Black or African American, 3.7% were Asian, 7.8% were American Indian (including Native Americans) or Alaskan Native, 0.2% were Native Hawaiian or Other Pacific Islander, and 1.7% were multiple races; 23.4% were Hispanic or Latino.
Solicited Adverse Reactions
Local and systemic adverse reactions were solicited within 7 days following the booster dose of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) using an electronic diary.
The reported frequency and severity of solicited local and systemic adverse reactions in participants 18 years of age and older are presented in Table 4.
|
a Solicited reactogenicity events and use of antipyretic or pain medication were collected by the participant in the electronic diary (eDiary). |
|||
| Event |
Novavax COVID-19 Vaccine, Adjuvanted (Original Monovalent) Booster |
||
|
Participants 18 through 64 Years |
Participants 65 Years and Older |
||
|
Local Adverse Reactionsd |
|||
|
Tendernesse |
|||
|
Any Grade |
6811 (69.4) | 887 (54.4) | |
|
Grade 3 |
676 (6.9) | 35 (2.1) | |
|
Grade 4 |
6 (< 0.1) | 1 (< 0.1) | |
|
Painf |
|||
|
Any Grade |
5773 (58.8) | 680 (41.7) | |
|
Grade 3 |
295 (3.0) | 18 (1.1) | |
|
Grade 4 |
4 (< 0.1) | 2 (0.1) | |
|
Redness (erythema)g |
|||
| Any Grade | 843 (8.6) | 110 (6.7) | |
| Grade 3 | 170 (1.7) | 13 (0.8) | |
| Swellingh | |||
| Any Grade | 765 (7.8) | 108 (6.6) | |
| Grade 3 | 101 (1.0) | 8 (0.5) | |
| Systemic Adverse Reactionsd | |||
| Muscle pain (myalgia)i | |||
| Any Grade | 5,329 (54.3) | 523 (32.1) | |
| Grade 3 | 853 (8.7) | 40 (2.5) | |
| Grade 4 | 10 (0.1) | 1 (< 0.1) | |
| Fatiguei | |||
| Any Grade | 5,150 (52.5) | 558 (34.2) | |
| Grade 3 | 1839 (18.7) | 130 (8.0) | |
| Grade 4 | 12 (0.1) | 0 | |
| Headachej | |||
| Any Grade | 4,645 (47.3) | 426 (26.1) | |
| Grade 3 | 539 (5.5) | 30 (1.8) | |
| Grade 4 | 6 (< 0.1) | 0 | |
| Malaisei | |||
| Any Grade | 3,946 (40.2) | 366 (22.5) | |
| Grade 3 | 935 (9.5) | 50 (3.1) | |
| Grade 4 | 12 (0.1) | 0 | |
| Joint pain (arthralgia)i | |||
| Any Grade | 2,525 (25.7) | 243 (14.9) | |
| Grade 3 | 495 (5.0) | 27 (1.7) | |
| Grade 4 | 5 (< 0.1) | 1 (< 0.1) | |
| Nausea or vomitingk | |||
| Any Grade | 1,232 (12.5) | 98 (6.0) | |
| Grade 3 | 45 (0.5) | 2 (0.1) | |
| Grade 4 | 5 (< 0.1) | 0 | |
| Feverl | |||
| Any Grade | 860 (8.8) | 69 (4.2) | |
| Grade 3 | 121 (1.2) | 5 (0.3) | |
| Grade 4 | 5 (< 0.1) | 1 (< 0.1) | |
Unsolicited Adverse Events
In Study 1, participants were monitored for unsolicited adverse events from the booster dose through 28 days after the booster dose and for serious adverse events, adverse events of special interest and vaccine-related medically attended events for the duration of study participation. In the booster dose period, 13,353 participants received Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent). Of the participants who received the booster dose, 96% had a follow-up duration of at least 2 months (median 6.7 months) after the booster dose.
From the booster dose through 28 days after the booster dose, the overall frequency of unsolicited adverse events, excluding events collected through a COVID-19 surveillance diary, was 4.7%. From the booster dose through the duration of follow up (median 6.7 months), serious adverse events were reported by 227 (1.7%) participants who received a booster dose of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent).
One serious event of non-ST elevation myocardial infarction was reported in a 28-year-old male participant 3 days after a booster dose of Novavax COVID-19 Vaccine, Adjuvanted; however, clinical features were also consistent with myocarditis (chest pain and elevated troponin), and no cardiac catheterization or cardiac MRI was performed during the acute presentation.
A serious adverse event of autoimmune hepatitis was reported in a 57-year-old male participant approximately 12 days after a booster dose of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent). A year prior to vaccination, the participant had transient increases in alanine transferase (ALT), up to 3 times the upper limit of normal (ULN). From a normal baseline ALT prior to receipt of the first dose of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent), ALT increased to 4 times ULN following the second dose of the primary series. After the booster dose, a recurrent and higher ALT increase was observed (7 times ULN). Viral hepatitis tests were negative, and no alternative etiologies have been identified. The event was ongoing for 8 months and was not resolved with azathioprine treatment. Currently available information for this event is insufficient to determine a causal relationship with the vaccine.
Two serious adverse events in the injected arm were reported, including muscle edema in a 51-year-old female with onset 7 days after booster vaccination and cellulitis of the injection site in a 58-year-old male with onset 3 days after booster vaccination. The cellulitis resolved following antibiotic and steroid treatment. The muscle edema was not responsive to non-steroidal anti-inflammatory agents. The event was reported as not resolved. Available information for these events is insufficient to determine a causal relationship with the vaccine.
A serious adverse event of extensive left leg and pelvic deep vein thrombosis and pulmonary embolism was reported 7 and 10 days, respectively, after booster in a 35-year-old female participant receiving oral contraceptive therapy. She required surgical intervention, thrombolytic therapy and prolonged anti-coagulation. Available information for this event is insufficient to determine a causal relationship with the vaccine.
2-Dose Series (Vaccine with a Different Manufacturing Process) in Vaccine-Naïve Adults
Study 2 was a randomized (1:1), placebo-controlled study that included a crossover design, with 10,795 participants who received at least one dose of a COVID-19 vaccine containing SARS-CoV-2 recombinant spike protein and Matrix-M adjuvant, manufactured by a different process than Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) evaluated in Study 1, and 10,864 participants who received at least one dose of placebo.
A serious event of Guillain Barré syndrome was reported 9 days following administration of Dose 1 of the vaccine. No events of Guillain Barré syndrome were reported following administration of placebo.
In Studies 3 and 4, approximately 5,500 participants received at least one dose of a COVID-19 vaccine containing SARS-CoV-2 recombinant spike protein and Matrix-M adjuvant, manufactured by a different process than Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) evaluated in Study 1. No serious adverse events considered related to vaccination were reported in these studies.
Myocarditis and/or pericarditis were reported in Study 2 and were not reported in Studies 3 and 4. In Study 2, serious events of myocarditis in a 19-year-old male and pericarditis in a 60-year-old female were reported 3 days following administration of Dose 2 and 11 days following Dose 1, respectively, of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent). No events of myocarditis or pericarditis were reported following administration of placebo.
Single Dose (Original Monovalent, Monovalent Omicron BA.1, or Bivalent Original and Omicron BA.1) in Vaccine-Experienced Adults
The safety of a Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) booster dose in individuals who completed a primary vaccination with another authorized or approved COVID-19 vaccine (heterologous booster dose) is inferred from the safety of a Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) booster dose administered following completion of a Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) primary series (homologous booster dose) and from a clinical study conducted in the US (NCT05463068; Study 5). This was a Phase 3, randomized study comparing 3 different lots of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) in 905 adults 18 through 49 years of age who had been previously vaccinated with a primary series of an authorized/approved COVID-19 vaccine with or without a booster, at least 6 months before receiving Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent). Most participants were previously vaccinated with Pfizer-BioNTech (57%) or Moderna (34%) COVID-19 Vaccines.
The safety of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent), Monovalent Vaccine (Omicron BA.1) and Bivalent Vaccine (Original monovalent and Omicron BA.1) administered as a booster dose to individuals 18 through 64 years of age, previously vaccinated with three doses of an authorized or approved mRNA COVID-19 vaccine was assessed in a randomized, observer blind study (NCT05372588, Part 1 in Australia; Study 6).
The safety analysis set included 274 participants in the Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) group, 286 participants in the Monovalent Vaccine (Omicron BA.1) group, and 269 participants in the Bivalent Vaccine (Original monovalent and Omicron BA.1) group. The median time since the last COVID-19 vaccination was 180.0 days. The median age of the population was 41 years (range 18 – 64); 727 (87.7%) participants were 18 through 54 years of age and 102 (12.3%) were 55 years and older. Overall, 46.1% were male, 53.9% were female; 2.4% were Hispanic or Latino; 80.6% were White, 0.2% were African American, 0.6% were Aboriginal Australian, 14.6% were Asian, 0.2% were Native Hawaiian or Pacific Islander, 2.7% were other races, and 1.1% were Multiracial. Demographic characteristics were similar across the three groups.
In Study 5, participants were monitored for medically attended unsolicited adverse events through 28 days after the booster dose. The overall frequency of these events was 4.3% and was similar for those previously vaccinated with either Pfizer-BioNTech or Moderna COVID-19 Vaccines. Serious adverse events were reported by 2 (0.2%) participants, with no events of myocarditis and/or pericarditis.
In Study 6, Part 1, participants were monitored through 28 days after the booster dose for unsolicited adverse events and through end of study (median duration of follow-up was 244 days) for serious adverse events. In the 28 days after vaccination, unsolicited adverse events were reported by 32.2%, 38.3% and 33.5% of participants who received the Monovalent Vaccine (Omicron BA.1), Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent), and Bivalent Vaccine (Original monovalent and Omicron BA.1), respectively. No unsolicited adverse events were severe and considered related to vaccine.
Serious adverse events were reported by 8 participants (8/286, 2.8%) in the Monovalent Vaccine (Omicron BA.1) group, 4 participants (4/274, 1.5%) in the Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) group, and 4 participants (4/269, 1.5%) in the Bivalent Vaccine (Original monovalent and Omicron BA.1) group. None of these serious adverse events were considered related to vaccination.
Single Dose (Original Monovalent, Monovalent Omicron BA.5, or Bivalent Original and Omicron BA.5) in Vaccine-Experienced Adults
The safety of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent), the Monovalent Vaccine (Omicron BA.5), and the Bivalent Vaccine (Original monovalent and Omicron BA.5) administered as a booster dose to individuals 18 years of age and older previously vaccinated with three or more doses of an authorized or approved mRNA COVID-19 vaccine was assessed in a randomized, observer blind study (NCT05372588, Part 2 in Australia; Study 6).
The safety analysis set included 251 participants in the Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) group, 254 participants in the Monovalent Vaccine (Omicron BA.5) group and 259 participants in the Bivalent Vaccine (Original monovalent and Omicron BA.5) group. The median time since the last COVID-19 vaccination was 352.5 days. The median age of the population was 43 years (range 18 – 83); 632 (82.7%) participants were 18 through 54 years of age and 132 (17.3%) were 55 years and older. Overall, 45.0% were male, 55.0% were female; 2.1% were Hispanic or Latino; 80.5% were White, 0.3% were African American, 2.0% were Aboriginal Australian, 12.3% were Asian, 0.7% were Native Hawaiian or Pacific Islander, 3.1% were other races, and 0.9% were Multiracial. Demographic characteristics were similar across the three groups. Safety analysis included a median follow-up of 220 days post booster dose through data extraction of 07 February 2024. The safety follow-up is ongoing.
Solicited Adverse Reactions
Local and systemic adverse reactions were solicited within 7 days following vaccination with Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent), the Monovalent Vaccine (Omicron BA.5), or the Bivalent Vaccine (Original monovalent and Omicron BA.5) using an electronic diary. In Study 6, in participants who had previously received authorized or approved mRNA Covid-19 vaccines, the percentages and types of reported solicited local and systemic adverse reactions were consistent with those reported by participants following administration of the Original Monovalent vaccine as presented in Table 4.
Unsolicited Adverse Events
Participants were monitored through 28 days after the booster dose for unsolicited adverse events and through end of study (median duration of follow-up was 220 days) for AESIs, serious adverse events, and treatment related medically attended adverse events. In the 28 days after 1 dose of study vaccine, unsolicited adverse events were reported by 19.7%, 25.9%, and 20.8% of participants who received the Monovalent Vaccine (Omicron BA.5), Novavax COVID-19 Vaccine (Original monovalent), and the Bivalent Vaccine (Original monovalent and Omicron BA.5), respectively. One unsolicited severe, related nonserious adverse event of diarrhea was reported.
Serious adverse events were reported by 7 participants (7/254, 2.8%) in the Monovalent Vaccine (Omicron BA.5) group, 10 participants (10/251, 4.0%) in the Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) group, and 3 participants (3/259, 1.2%) in the Bivalent Vaccine (Original monovalent and Omicron BA.5) group.
Two participants reported serious adverse events of cranial nerve palsy, including a serious adverse event of fourth cranial nerve palsy with onset of symptoms 7 days post vaccination and a serious adverse event of sixth cranial nerve palsy with onset of symptoms 14 days post vaccination. Both participants had predisposing risk factors, including diabetes, hypertension, and hypercholesterolemia. Currently available information on oculomotor cranial palsies is insufficient to determine a causal relationship with the vaccine.
One participant reported a serious adverse event of vestibular neuronitis (eighth cranial nerve), which occurred twice (11 days after dose one and 16 days after dose two of study vaccine), and was assessed as related to the vaccine.
Single Dose (Monovalent Omicron XBB.1.5) in Vaccine-Naïve Adults with Evidence of Prior SARS-CoV-2 Infection and in Vaccine-Experienced Adults
The safety of Novavax COVID-19 Vaccine, Adjuvanted (2023-2024 Formula) administered as a single dose in baseline SARS-CoV-2 seropositive and COVID-19 vaccine-naïve individuals 18 years of age and older was assessed in an open-label study in the US and US territories (NCT05975060, Part 2; Study 7).
The safety analysis set included 338 participants. The median age of the population was 38 years (range 18 to 75 years); 284 (84.0%) participants were 18 through 54 years of age, and 54 (16.0%) were 55 years and older. Overall, 56.2% were female, 43.8% were male; 49.4% were White, 43.5% were Black or African American, 1.8% were American Indian or Alaskan Native, 0.3% were Native Hawaiian or Other Pacific Islander, 0.6% were Asian, 0.9% were other races, and 1.5% were Multiracial; 25.7% were Hispanic or Latino. Safety analysis included a median follow-up of 171 days post single-dose vaccination through end of study.
Solicited Adverse Reactions
Local and systemic adverse reactions were solicited within 7 days following single-dose vaccination with Novavax COVID-19 Vaccine, Adjuvanted (2023-2024 Formula) in COVID-19 vaccine-naïve adult participants. The reported frequency and severity of solicited local and systemic adverse reactions in participants 18 years of age and older are presented in Table 5.
| Event | Novavax COVID-19 Vaccine, Adjuvanted (2023-2024 Formula) Single Dose |
|---|---|
|
a Solicited reactogenicity events and use of antipyretic or pain medication were collected by the participant in the electronic diary (eDiary). |
|
| N=338
n (%) |
|
| Local Adverse Reactionsd | |
| Tendernesse | |
| Any Grade | 129 (38.2) |
| Grade 3 | 3 (0.9) |
| Painf | |
| Any Grade | 85 (25.1) |
| Grade 3 | 2 (0.6) |
| Redness (erythema)g | |
| Any Grade | 4 (1.2) |
| Swellingh | |
| Any Grade | 1 (0.3) |
| Systemic Adverse Reactionsd | |
| Muscle paini | |
| Any Grade | 106 (31.4) |
| Grade 3 | 4 (1.2) |
| Headachej | |
| Any Grade | 92 (27.2) |
| Grade 3 | 3 (0.9) |
| Fatiguei | |
| Any Grade | 80 (23.7) |
| Grade 3 | 3 (0.9) |
| Malaisei | |
| Any Grade | 48 (14.2) |
| Grade 3 | 3 (0.9) |
| Joint paini | |
| Any Grade | 44 (13.0) |
| Grade 3 | 2 (0.6) |
| Nausea/vomitingk | |
| Any Grade | 42 (12.4) |
| Grade 3 | 2 (0.6) |
| Feverl | |
| Any Grade | 3 (0.9) |
Unsolicited Adverse Events (non-serious and serious)
Participants were monitored through 28 days after single-dose vaccination for unsolicited adverse events. Of the 338 participants who received a dose of study vaccine, unsolicited adverse events were reported by 5.3% of participants. Of these, 1 participant reported a non-serious unsolicited adverse event considered related to the study vaccine (heavy menstrual bleeding), and 1 participant reported a serious adverse event (obstructive pancreatitis) assessed as severe in intensity and not related to vaccination.
Serious adverse events were reported by 5 (1.5%) participants after single-dose vaccination with Novavax COVID-19 Vaccine, Adjuvanted (2023-2024 Formula) through end of study (median duration of follow-up was 171 days), and none were assessed as related to study vaccine.
Adolescents 12 Years Through 17 Years of Age
Safety of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) in adolescents was assessed in the adolescent part of Study 1 conducted in the US. In this study, 2,153 participants 12 through 17 years of age received at least one primary series dose of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent).
2-Dose Series (Original Monovalent) in Vaccine-Naïve Adolescents
Study 1 was a Phase 3, multicenter, randomized (2:1), observer-blinded, placebo-controlled, crossover study adolescent participants 12 through 17 years of age in the US. Participants were randomized (2:1) to receive 2 doses of the vaccine or placebo administered 21 days apart.
In the adolescent part of Study 1, participants 12 through 17 years of age received at least one dose of vaccine (n=1,487) or placebo (n=745) in the pre-crossover period; 50.8% were male, 49.2% were female; 75.0% were White, 13.6% were Black or African American, 2.9% were Asian, 2.2% were American Indian (including Native Americans) or Alaskan Native, and 5.5% were multiple races; 18.4% were Hispanic/Latino. Demographic characteristics were similar between the Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) and placebo groups. During the study, COVID-19 vaccines authorized for emergency use became available, and participants, when eligible for vaccination, were offered the opportunity to cross over from the originally assigned study treatment to the other study treatment (vaccine or placebo) in a blinded fashion (“blinded crossover”). In the post-crossover period, 666 participants received Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent), and 1,354 participants received placebo. The demographic characteristics were similar between participants in the pre-crossover and post-crossover groups.
Solicited Adverse Reactions
During the pre-crossover period, local and systemic adverse reactions were solicited within 7 days following each dose of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) or placebo in participants using an electronic diary.
The reported frequency and severity of solicited local and systemic adverse reactions in participants 12 through 17 years of age are presented in Table 6.
| Event | Novavax COVID-19 Vaccine, Adjuvanted (Original Monovalent) | Placebod | ||
|---|---|---|---|---|
| Dose 1 N=1,448 n (%) | Dose 2 N=1,394 n (%) | Dose 1 N=726 n (%) | Dose 2 N=686 n (%) |
|
|
a Solicited reactogenicity events and use of antipyretic or pain medication were recorded by participants’ parent(s)/caregiver(s) and collected in the electronic diary (eDiary). |
||||
| Local Adverse Reactionse | ||||
| Tendernessf | ||||
| Any Grade | 819 (56.6) | 909 (65.2) | 153 (21.1) | 97 (14.1) |
| Grade 3 | 16 (1.1) | 93 (6.7) | 2 (0.3) | 1 (0.1) |
| Paing | ||||
| Any Grade | 647 (44.7) | 850 (61.0) | 126 (17.4) | 102 (14.9) |
| Grade 3 | 10 (0.7) | 38 (2.7) | 2 (0.3) | 3 (0.4) |
| Swellingh | ||||
| Any Grade | 20 (1.4) | 111 (8.0) | 3 (0.4) | 1 (0.1) |
| Grade 3 | 0 | 8 (0.6) | 0 | 0 |
| Redness (erythema)i | ||||
| Any Grade | 15 (1.0) | 104 (7.5) | 5 (0.7) | 0 |
| Grade 3 | 0 | 10 (0.7) | 0 | 0 |
| Systemic Adverse Reactionse | ||||
| Muscle pain (myalgia)j | ||||
| Any Grade | 492 (34.0) | 684 (49.1) | 114 (15.7) | 82 (12.0) |
| Grade 3 | 17 (1.2) | 104 (7.5) | 4 (0.6) | 6 (0.9) |
| Headachek | ||||
| Any Grade | 440 (30.4) | 793 (56.9) | 181 (24.9) | 119 (17.3) |
| Grade 3 | 13 (0.9) | 87 (6.2) | 12 (1.7) | 14 (2.0) |
| Grade 4 | 0 | 1 (< 0.1) | 0 | 0 |
| Fatiguej | ||||
| Any Grade | 350 (24.2) | 696 (49.9) | 112 (15.4) | 100 (14.6) |
| Grade 3 | 23 (1.6) | 189 (13.6) | 9 (1.2) | 11 (1.6) |
| Malaisej | ||||
| Any Grade | 215 (14.8) | 560 (40.2) | 67 (9.2) | 51 (7.4) |
| Grade 3 | 16 (1.1) | 126 (9.0) | 7 (1.0) | 4 (0.6) |
| Nausea or vomitingl | ||||
| Any Grade | 113 (7.8) | 277 (19.9) | 56 (7.7) | 33 (4.8) |
| Grade 3 | 2 (0.1) | 14 (1.0) | 3 (0.4) | 3 (0.4) |
| Grade 4 | 0 | 1 (< 0.1) | 0 | 0 |
| Joint pain (arthralgia)j | ||||
| Any Grade | 102 (7.0) | 225 (16.1) | 35 (4.8) | 21 (3.1) |
| Grade 3 | 6 (0.4) | 40 (2.9) | 1 (0.1) | 2 (0.3) |
| Feverm | ||||
| Any Grade | 9 (0.6) | 235 (16.9) | 4 (0.6) | 1 (0.1) |
| Grade 3 | 1 (< 0.1) | 31 (2.2) | 0 | 0 |
Unsolicited Adverse Events
In Study 1, participants were monitored for unsolicited adverse events from the first dose through 28 days after the second dose in both the pre- and post-crossover periods and for serious adverse events, AESIs and vaccine-related medically attended adverse events for the duration of study participation. Participants who received at least one dose in the pre- or post-crossover periods were included in the safety analysis. In the pre-crossover period 1,487 participants received Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) and 745 participants received placebo. In the post-crossover period, 666 participants received Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) and 1,354 received placebo. Of participants who received two doses of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) in the pre-crossover period (n=1,468), 86% had a follow-up duration of at least 2 months (median = 71 days) after Dose 2. Of participants who received two doses of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) in the post-crossover period (n=658), 99.7% had a follow-up duration of at least 2 months (median = 234 days) after the last dose.
From Dose 1 through 28 days following Dose 2 in the pre-crossover period, the overall frequency of unsolicited adverse events was 15.8% in the Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) group vs 16.0% in the placebo group. From Dose 1 through 28 days following Dose 2 in the post-crossover period, the overall frequency of unsolicited adverse events was 17.1% in the Placebo/Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) group vs 14.6% in the Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent)/Placebo group. In an analysis of all unsolicited adverse events reported following any dose, through 28 days following Dose 2, those assessed as adverse reactions not already captured by solicited local and systemic reactions in the Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) group and placebo group were lymphadenopathy (0.7% vs 0 pre-crossover and 0.2% vs 0.2% post-crossover) and chills (0.3% vs 0.3% pre-crossover and 0.6% vs 0.1% post-crossover), respectively.
In the pre-crossover period, serious adverse events were reported by 7 (0.5%) participants in the Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) group and by 2 (0.3%) participants in the placebo group. In the post-crossover period, serious adverse events were reported by 8 (1.2%) participants who received Placebo/Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) and by 11 (0.8%) participants who received Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent)/Placebo.
A total of one event of myocarditis was reported by one (0.05%) participant after Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) and no events were reported by participants after placebo. One serious adverse event of myocarditis was reported by a 16-year-old male 2 days after Dose 2.
Single Dose (Original Monovalent) in Vaccine-Experienced Adolescents
In an open-label portion of Study 1, 1,495 participants 12 through 17 years of age received a single booster dose of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) (0.5 mL) at least 5 months after the two-dose primary series (median of 10.3 months between completion of primary series and booster dose); an additional 4 participants received the dose without having completed the two-dose primary series. Safety analyses included evaluation of solicited local and systemic adverse reactions within 7 days after a booster dose for participants who completed the electronic diary (n=1,256) and unsolicited adverse events within 28 days after a booster dose (n=1,499). Safety analysis also included evaluation of serious adverse events, adverse events of special interest and vaccine-related medically attended events after a booster dose (n=1,499) with a median follow-up of 3.4 months post booster dose. The safety follow-up is ongoing.
Among the 1,499 adolescent participants, 53.8% were male, 46.2% were female; 73.1% were White, 14.6% were Black or African American, 3.5% were Asian, 2.7% were American Indian (including Native Americans) or Alaskan Native, 0.3% were Native Hawaiian or Other Pacific Islander, and 5.1% were multiple races; 18.4% were Hispanic or Latino.
Solicited Adverse Reactions
Local and systemic adverse reactions were solicited within 7 days following the booster dose of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) using an electronic diary.
The reported frequency and severity of solicited local and systemic adverse reactions in a subset of participants 12 years through 17 years of age are presented in Table 7.
| Event | Novavax COVID-19 Vaccine, Adjuvanted (Original Monovalent) Booster N=1,256 n (%) |
|---|---|
|
a Solicited reactogenicity events and use of antipyretic or pain medication were recorded by participants’ parent(s)/caregiver(s) and collected in the electronic diary (eDiary). |
|
| Local Adverse Reactionsd | |
| Tendernesse | |
| Any Grade | 828 (65.9) |
| Grade 3 | 116 (9.2) |
| Grade 4 | 1 (< 0.1) |
| Painf | |
| Any Grade | 812 (64.6) |
| Grade 3 | 61 (4.9) |
| Redness (erythema)g | |
| Any Grade | 129 (10.3) |
| Grade 3 | 29 (2.3) |
| Swellingh | |
| Any Grade | 119 (9.5) |
| Grade 3 | 18 (1.4) |
| Systemic Adverse Reactionsd | |
| Headachei | |
| Any Grade | 790 (62.9) |
| Grade 3 | 154 (12.3) |
| Grade 4 | 2 (0.2) |
| Muscle pain (myalgia)j | |
| Any Grade | 758 (60.4) |
| Grade 3 | 143 (11.4) |
| Grade 4 | 1 (< 0.1) |
| Fatiguej | |
| Any Grade | 717 (57.1) |
| Grade 3 | 216 (17.2) |
| Grade 4 | 1 (< 0.1) |
| Malaisej | |
| Any Grade | 566 (45.1) |
| Grade 3 | 170 (13.5) |
| Grade 4 | 1 (< 0.1) |
| Nausea or vomitingk | |
| Any Grade | 296 (23.6) |
| Grade 3 | 20 (1.6) |
| Joint pain (arthralgia)j | |
| Any Grade | 275 (21.9) |
| Grade 3 | 50 (4.0) |
| Grade 4 | 1 (< 0.1) |
| Feverl | |
| Any Grade | 211 (16.8) |
| Grade 3 | 44 (3.5) |
| Grade 4 | 3 (0.2) |
Unsolicited Adverse Events
In Study 1, participants were monitored for unsolicited adverse events from the booster dose through 28 days after the booster dose and for serious adverse events, adverse events of special interest and vaccine-related medically attended events for the duration of study participation. In the booster dose period, 1,499 adolescent participants received Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent). Of the participants who received the booster dose, 98% had a follow-up duration of at least 2 months (median 6.6 months) after the booster dose. From the booster dose through 28 days after the booster dose, the proportion of participants reporting an unsolicited adverse event was 6.4% and the proportion of participants reporting lymphadenopathy was 0.4%.
Serious adverse events in the boosted population of 1,499 participants were reported by 19 (1.3%) participants who received a booster dose of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent), with no reported events of myocarditis and/or pericarditis.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-authorization use of Novavax COVID-19 Vaccine, Adjuvanted. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to vaccine exposure.
Cardiac Disorders: myocarditis, pericarditis
Immune System Disorders: anaphylaxis
Nervous System Disorders: paresthesia, hypoesthesia
Related/similar drugs
8. Use In Specific Populations
8.1 Pregnancy
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to NUVAXOVID during pregnancy. Women who are vaccinated with NUVAXOVID during pregnancy are encouraged to enroll in the registry by visiting https://c-viper.pregistry.com/.
Risk Summary
All pregnancies have a risk of birth defect, loss, or other adverse outcomes. In the US general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively. Available data on NUVAXOVID administered to pregnant women are insufficient to inform vaccine-associated risks in pregnancy.
A developmental toxicity study was performed in female rats administered a vaccine formulation containing the same quantity of SARS-CoV-2 recombinant spike protein and one-fifth the quantity of adjuvant and formulation buffer inactive ingredients included in Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) on four occasions, twice prior to mating and twice during gestation. The study revealed no evidence of harm to the fetus due to the vaccine (see Animal Data).
Clinical Considerations
Disease-Associated Maternal and/or Embryo/Fetal Risk
Pregnant women infected with SARS-CoV-2 are at increased risk of severe COVID-19 compared with non-pregnant individuals.
Data
In a developmental toxicology study, 0.1 mL of a vaccine formulation containing the same quantity of SARS-CoV-2 rS protein (5 mcg), one-fifth the quantity of adjuvant (10 mcg), and inactive ingredients which comprise the formulation buffer [25 mM sodium phosphate, 300 mM sodium chloride, and 0.01% (w/v) polysorbate 80] contained in a single dose of the Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) was administered to female rats by the intramuscular route on four occasions: 27 and 13 days prior to mating, and on gestational days 7 and 15. No vaccine-related adverse effects on female fertility, fetal development, or postnatal development were reported in this study.
8.2 Lactation
Risk Summary
It is not known whether NUVAXOVID is excreted in human milk. Data are not available to assess the effects of NUVAXOVID on the breastfed infant or on milk production/excretion. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for NUVAXOVID and any potential adverse effects on the breastfed child from NUVAXOVID or from the underlying maternal condition. For preventive vaccines, the underlying maternal condition is susceptibility to disease otherwise prevented by the vaccine.
8.4 Pediatric Use
The safety and effectiveness of NUVAXOVID in adolescents 12 through 17 years of age with at least one underlying condition that puts them at high risk for severe outcomes from COVID-19 is based on safety and effectiveness data in this age group and in adults [see Adverse Reactions (6) and Clinical Studies (14.2)].
The safety and effectiveness of NUVAXOVID in individuals younger than 12 years of age have not been established.
8.5 Geriatric Use
In a clinical study (Study 1), out of 19,735 subjects who received primary vaccination with Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent), 12.6% (n=2,480) were 65 years of age and older and 1.8% (n=361) were 75 years of age and older. Overall, there were no notable differences in the safety profiles observed between participants 65 years of age and older and younger participants [see Adverse Reactions (6)]. Study 1 did not include sufficient numbers of participants aged 65 years and older to determine whether they respond differently from younger participants [see Clinical Studies (14.1)].
In this study, among subjects who received a booster dose of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) (n=13,353), 15.5% (n=2,064) of participants were 65 years of age and older and 2.5% (n=334) of participants were 75 years of age and older. Overall, there were no notable differences in the safety profiles observed between participants 65 years of age and older and younger participants [see Adverse Reactions (6)]. The effectiveness of the booster dose in participants aged 65 years and older was consistent with that observed in participants 18 years through 64 years [see Clinical Studies (14.1)].
Studies 6 and 7 did not include sufficient numbers of patients 65 years of age and older to determine whether they respond differently from younger adult patients.
11. Nuvaxovid Description
NUVAXOVID (COVID-19 Vaccine, Adjuvanted) is a colorless to slightly yellow, clear to mildly opalescent sterile suspension for intramuscular use that is free from visible particles. Each 0.5 mL dose of NUVAXOVID (2025-2026 Formula) contains 5 mcg of recombinant spike (rS) protein of the SARS-CoV-2 Omicron variant lineage JN.1 and 50 mcg Matrix-M adjuvant. The Matrix-M adjuvant is composed of Fraction-A (42.5 mcg) and Fraction-C (7.5 mcg) of saponin extracts from the soapbark tree, Quillaja saponaria Molina. The rS protein is produced by recombinant DNA technology using a baculovirus expression system in the Sf9 insect cell line that is derived from the Spodoptera frugiperda species.
Each 0.5 mL dose of NUVAXOVID also contains the following ingredients: cholesterol (30.5 mcg), phosphatidylcholine (23 mcg), potassium dihydrogen phosphate (3.85 mcg), potassium chloride (2.25 mcg), disodium hydrogen phosphate dihydrate (14.7 mcg), disodium hydrogen phosphate heptahydrate (2.465 mg), sodium dihydrogen phosphate monohydrate (0.445 mg), sodium chloride (8.766 mg), polysorbate 80 (0.050 mg), and Water for Injection. The pH is adjusted with sodium hydroxide or hydrochloric acid.
Each 0.5 mL dose of NUVAXOVID may also contain residual amounts of baculovirus and Sf9 cell proteins (≤ 0.96 mcg), baculovirus and cellular DNA (≤ 0.00016 mcg), lentil lectin (< 0.025 mcg), methyl-α-D-mannopyranoside (2 mcg), simethicone (< 0.92 mcg), pluronic F-68 (< 2.19 mcg), Triton X-100 (< 0.025 mcg), Tergitol (NP9) (< 0.05 mcg), and DL-α-tocopherol (≤ 0.05 mcg).
NUVAXOVID does not contain a preservative.
The syringe tip cap and plunger stopper are not made with natural rubber latex.
14. Clinical Studies
14.1 Adults 18 Years of Age and Older
Efficacy of 2-Dose Series (Original Monovalent) in Vaccine-Naïve Adults
Study 1 adult main study was a Phase 3, multicenter, randomized, observer-blinded, placebo-controlled, crossover study in participants 18 years of age and older in the US and Mexico who were considered to be at higher risk of exposure to and infection with SARS-CoV-2. Eligible participants were medically stable and had no history of previous laboratory-confirmed (by PCR or serology to SARS-CoV-2) diagnosis of SARS-CoV-2 infection or COVID-19 prior to randomization. SARS-CoV-2 PCR samples were tested by a central laboratory. The study excluded individuals who were significantly immunocompromised due to immunodeficiency disease; had received chronic immunosuppressive therapy or had received immunoglobulin or blood-derived products within 90 days; or had a history of laboratory-confirmed diagnosed COVID-19. Individuals with clinically stable underlying comorbidities were included, as were individuals with well-controlled human immunodeficiency virus (HIV) infection. Participants were stratified by age into two strata (18 to < 65 years and ≥ 65 years) and randomized to Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) or placebo (normal saline) in a 2:1 ratio. A total of 29,943 participants were randomized in a 2:1 ratio to receive two doses of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) or placebo 21 days apart. Assessments of safety and efficacy against COVID-19 were conducted for up to 24 months after the second dose.
The primary efficacy analysis population (Per-Protocol Efficacy [PP-EFF] Analysis Set) included 25,510 participants who received a 2-dose series (dose 1 on day 0 and dose 2 on day 21) of either Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) (n=17,184) or placebo (n=8,326), did not experience an exclusionary protocol deviation, and did not have evidence of SARS-CoV-2 infection at baseline or through 6 days after the second dose.
In the PP-EFF Analysis Set, 48.4% were female; 21.4% were Hispanic or Latino; 75.9% were White, 11.1% were Black or African American, 6.1% were American Indian or Alaska Native, 4.4% were Asian, and 1.7% were Multiracial. 94.2% participants were enrolled at sites in the US and 5.8% participants were enrolled at sites in Mexico. The median age of participants was 47 years (range 18 – 95 years) and 11.7% were 65 years of age and older. Of the study participants in the PP-EFF Analysis Set, 95.2% were at high risk for COVID-19 due to living or working conditions involving known frequent exposure to SARS-CoV-2, comorbidities (chronic lung disease, cardiovascular disease, chronic liver disease, severe obesity, and diabetes), or age ≥ 65 years. Between participants who received Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) and those who received placebo, there were no notable differences in demographics or pre-existing medical conditions. Participants in the PP-EFF Analysis Set were included in the primary efficacy analysis up until the earliest of the time that they received their crossover vaccination, they received a booster dose (if they did not receive a crossover vaccine) or were censored.
The primary efficacy endpoint was defined as the first PCR-positive symptomatic mild, moderate, or severe COVID-19 illness diagnosed 7 or more days after completion of the second dose of the primary series during the pre-crossover period. Mild COVID-19 was defined as at least one of the following: fever (defined by subjective or objective measure, regardless of use of anti-pyretic medications), new onset of cough, or two or more COVID-19 symptoms (new onset or worsening of shortness of breath or difficulty breathing compared to baseline; new onset fatigue; new onset generalized muscle or body aches; new onset headache; new loss of taste or smell; acute onset of sore throat, congestion or runny nose; new onset nausea, vomiting or diarrhea). Moderate COVID-19 was defined as at least one of the following: high fever (≥ 38.4 °C for ≥ 3 days [regardless of use of anti-pyretic medications, need not be contiguous days]), or any evidence of lower respiratory tract infection (shortness of breath [or breathlessness or difficulty breathing] with or without exertion [greater than baseline]; tachypnea 24 to 29 breaths per minute at rest; SpO2: 94% to 95% on room air; abnormal chest X-ray or chest computerized tomography consistent with pneumonia or lower respiratory tract infection; or adventitious sounds on lung auscultation [i.e., crackles/rales, wheeze, rhonchi, pleural rub, stridor]). Severe COVID-19 was defined as at least one of the following: tachypnea ≥ 30 breaths per minute at rest; resting heart rate ≥ 125 beats per minute; SpO2 ≤ 93% on room air; PaO2/FiO2 < 300 mmHg; high flow oxygen therapy or NIV/NIPPV; mechanical ventilation or extracorporeal membrane oxygenation; evidence of shock (systolic blood pressure < 90 mmHg, diastolic blood pressure < 60 mmHg or requiring vasopressors); significant acute renal, hepatic, cardiac, or neurologic dysfunction or failure; admission to an intensive care unit; or death.
The efficacy of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) to prevent PCR-confirmed symptomatic mild, moderate, or severe COVID-19 from 7 days after Dose 2 was 89.6% (95% CI: 82.5%, 93.8%) in participants without evidence of SARS-CoV-2 infection through 6 days after the second dose (see Table 8). The primary efficacy endpoint criterion for success was met as the lower limit of the confidence interval was > 30%. In the PP-EFF Analysis Set, no cases of moderate or severe COVID-19 were reported in participants who had received Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent), compared with eight cases of moderate COVID-19 and four cases of severe COVID-19 that were reported in participants who had received placebo. The PP-EFF Analysis Set had a median follow-up of 2 months post-Dose 2 during the pre-crossover period.
| Novavax COVID-19 Vaccine, Adjuvanted (Original Monovalent) | Placebo | Vaccine Efficacy (95% CI) (%) |
|||||
|---|---|---|---|---|---|---|---|
| Participants N | COVID-19 Cases n (%) | Mean Incidence Rate Per 1,000 Person-Yearsb | Participants N | COVID-19 Cases n (%) | Mean Incidence Rate Per 1,000 Person-Yearsb | ||
| * The PP-EFF Analysis Set had a median follow-up of 2 months post-Dose 2 during the pre-crossover period. a Vaccine efficacy (VE) evaluated in participants without major protocol deviations who are seronegative (for SARS-CoV-2) at baseline and do not have a laboratory confirmed current SARS-CoV-2 infection with symptom onset through 6 days after the second dose, and who have received two doses of vaccine or placebo as randomized. b Mean incidence rate per 1,000 person-years was estimated with weighting for age strata reflective of the distribution seen in the study population. c Based on log-linear model of PCR-confirmed COVID-19 infection incidence rate using Poisson regression with treatment group and age strata as fixed effects and robust error variance, where VE = 100 × (1 – ratio of incidence rate) (Zou 2004). |
|||||||
| Primary efficacy endpoint | |||||||
| All participants | 17,184 | 18 (0.1) | 6.0 | 8,326 | 76 (0.9) | 57.2 | 89.6 (82.5, 93.8)c |
| Mild | – | 18 (0.1) | – | – | 64 (0.8) | – | – |
| Moderate | 0 | 8 (0.1) | |||||
| Severe | 0 | 4 (< 0.1) | |||||
Descriptive analyses of efficacy showed efficacy point estimates similar to the estimate for the overall study population across genders and racial groups, and across participants with or without medical comorbidities associated with high risk of severe COVID-19. Vaccine efficacy in participants of Hispanic/Latino ethnicity was 77.4% (95% CI: 49.6%, 89.8%), and in participants who were not Hispanic/Latino, it was 93.2% (95% CI: 86.3%, 96.6%). Vaccine efficacy in participants 65 years of age and older was 68.0% (95% CI: -43.0%, 92.8%), and in participants 50 through 64 years of age, it was 89.2% (95% CI: 67.9%, 96.4%).
Immunogenicity of a Single Dose (Original Monovalent) in Vaccine-Experienced Adults
Effectiveness of a booster dose of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) in vaccine-experienced adults was based on assessment of neutralizing antibody titers (MN50) against the original SARS-CoV-2 strain (SARS-CoV-2 hCoV-19/Australia/VIC01/2020). Immunogenicity analyses compared the MN50 titers following the booster dose to the MN50 titers following the primary series.
In the open-label booster dose phase of Study 1, participants 18 years of age and older received a single booster dose of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) at least 6 months after completion of the primary series. A subset of 225 participants were included in the per-protocol immunogenicity (PP-IMM) analysis set. The median age of participants in the PP-IMM analysis set was 52 years (range 19 to 79 years). Overall, 52.0% were male and 48.0% were female; 82.7% were White, 9.3% were Black or African American, 0.4% were American Indian or Alaskan Native, 0.4% were Native Hawaiian or Other Pacific Islander, 5.8% were Asian, and 1.3% were Multiracial; 14.7% were Hispanic or Latino.
Prespecified noninferior immunogenicity analyses included an assessment of MN50 geometric mean titer (GMT) ratio and difference in seroconversion rates. Seroconversion for a participant was defined as achieving a 4-fold rise in MN50 from baseline (before the booster dose and before the first dose of the primary series).
The analysis of the GMT ratio of MN50 following the booster dose compared with that following the primary series met the noninferiority criteria for a booster dose response (lower limit of the 95% CI > 0.67) and point estimate > 0.83 (see Table 9).
| Assay | Time Point | Booster Dose n=222b | Primary Series n=222b | GMR (95% CI)c | Met Noninferiority Criteriag,h |
|---|---|---|---|---|---|
| GMT (95% CI)c | GMT (95% CI)c |
||||
| Abbreviations: CI = confidence interval; GMT = geometric mean titer; MN50 = microneutralization assay with an inhibitory concentration of 50%; PP-IMM = Per-Protocol Immunogenicity; SCR = seroconversion rate. a PP-IMM Analysis Set included participants who received two doses (0.5 mL 21 days apart) of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) in the initial vaccination period or in the blinded crossover vaccination period, had an immunogenicity blood sample collected at Day 35, did not have serologic or virologic evidence of SARS-CoV-2 infection up to 28 days post booster dose, did not receive an emergency use authorized COVID-19 vaccine, received the booster dose, and remained blinded on study and without major protocol deviations until 7 days post-crossover Dose. b The analysis included a total of 222 participants of the PP-IMM analysis set who had immunogenicity data (microneutralization) available for both the booster dose and primary series. c The 95% CI for GMT and GMT ratio were calculated based on the t-distribution of the log-transformed values, then back transformed to the original scale for presentation. d The 95% CI for SCR was based on the Clopper-Pearson method. e Comparison between SCR of 28 days post-booster dose relative to time of booster dose and SCR of 14 days after second dose of the primary series relative to time of first dose. f Based on the Tango method. g Noninferiority of the single booster dose was achieved if the lower limit of the 95% CI for the ratio of MN50 GMT at 28 days after a single booster dose versus 14 days after the second dose of NVX-CoV2373 was > 0.67 and the point estimate > 0.83. h Noninferiority of the single booster dose was achieved if the lower limit of the 95% CI for the difference of the proportion of participants with SCR at 28 days after a single booster dose relative to the time of booster dose vaccination versus at 14 days after the second dose of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) relative to the time of first vaccination was > -10%. Note: The median duration between the time of the second dose of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) and the time of the booster dose was 11 months. Note: The SCR percentage was defined as percentage of participants at the post vaccination visit with a >= 4-fold rise from baseline if baseline is equal to or above LLOQ, or at least 4-fold rise from LLOQ if baseline is below LLOQ in antibody. |
|||||
| SARS-CoV-2 wild-type microneutralization assay (1/dilution) | 28 days after Booster Dose; 14 days after Primary Series Dose 2 | 4947.1 (4315.6, 5671.1) | 1553.4 (1277.3, 1889.1) | 3.2 (2.7, 3.8) | Yes |
| SCR n(%) (95% CI)d | SCR n(%) (95% CI)d | Difference in SCR%e (95% CI)f |
|||
| 205 (92.3) (88.0, 95.5) | 209 (94.1) (90.2, 96.8) | -1.8 (-6.1, 2.3) |
|||
Immunogenicity of a Single Dose (Monovalent Omicron XBB.1.5) in Vaccine-Naïve Adults with Evidence of Prior SARS-CoV-2 Infection and in Vaccine-Experienced Adults
Study 7 was an open-label, single arm study conducted in the US and US territories that included participants 18 years of age and older. This study compared specific immune responses of COVID-19 vaccine-naïve participants who had a clinical history of COVID-19-like disease with immunologic or virologic evidence of prior SARS-CoV-2 infection (defined as a positive Roche Elecsys immunoassay result at Day 0) and no active infection (defined as a negative RT-PCR test at Day 0) with those of participants who were previously vaccinated (received at least 3 doses of the Pfizer-BioNTech COVID-19 Vaccine or the Moderna COVID-19 Vaccine). All participants received a single dose of Novavax COVID-19 Vaccine, Adjuvanted (2023-2024 Formula). The primary immunogenicity analysis population included 288 participants who were baseline SARS-CoV-2 seropositive and COVID-19 vaccine-naïve and 305 participants who were previously vaccinated. Among vaccine-naïve participants in the primary immunogenicity analysis subset, the median age of participants was 38 years, 40.6% were male, 59.4% were female; 50.0% were White, 43.1% were African American or Black, 2.1% were American Indian or Alaska Native, 0.7% were Asian, 0.3% were Native Hawaiian or Other Pacific Islander, 0.7% were other races, and 1.7% were Multiracial; 26.0% were Hispanic or Latino. Among participants who were previously vaccinated, the median age of participants was 53 years, 38.4% were male, 61.6% were female; 75.1% were White, 14.8% were African American or Black, 3.9% were Asian, 2.0% were American Indian or Alaska Native, 0.7% were Native Hawaiian or Other Pacific Islander, 0.3% were other races, and 1.0% were Multiracial; 19.7% were Hispanic or Latino.
The co-primary immunogenicity analyses of the GMT ratio and seroresponse rates (defined as the percentage of participants achieving a 4-fold rise in titer from baseline) against a pseudovirus expressing Omicron XBB.1.5 following the single dose in vaccine-naïve participants compared with after a single dose in participants who were previously vaccinated met the pre-defined success criteria for noninferiority for Omicron XBB.1.5. These analyses are summarized in Table 10.
| Vaccine-naïvea
n=288 | Previously Vaccinatedb
n=305 |
|
|---|---|---|
| Abbreviations: CI = confidence interval; GMT = geometric mean titer; n = number of participants in the assay-specific PP-IMM Analysis Set with non-missing data at both Baseline and Day 28 for this strain; LLOQ = lower limit of quantification; NP = nucleocapsid protein; PCR = polymerase chain reaction; PP = Per-Protocol; SARS-CoV-2 = severe acute respiratory syndrome coronavirus 2; SSR = seroresponse rate. a The PP Pseudovirus Neutralization Assay Novavax Clinical Immunology Subset for vaccine-naïve participants included all participants with a clinical history of COVID-19-like disease who had not received any COVID-19 vaccine prior to enrollment in Study 7, received the full regimen of the study vaccine according to protocol, were anti-NP antibody seropositive at baseline, were RT-PCR negative for active SARS-COV-2 infection at baseline, had neutralization assay results available at baseline and at Day 28, and had no major protocol violations that were considered clinically relevant to impact immunogenicity response. b The PP Pseudovirus Neutralization Assay Novavax Clinical Immunology Subset for previously vaccinated participants included all participants who received at least 3 doses of an mRNA COVID-19 vaccine prior to enrollment in Study 7, received the full regimen of the study vaccine according to protocol, were RT-PCR negative for active SARS-CoV-2 infection at baseline, had neutralization assay results available at baseline and at Day 28, and had no major protocol violations or an event that were considered clinically relevant to impact immunogenicity response. c An ANCOVA with vaccine group as fixed effect and baseline value (Day 0) as covariate was performed to estimate the adjusted GMT and GMT ratio. The mean difference between vaccine groups and the corresponding CI limits was then exponentiated to obtain the ratio of GMTs and the corresponding 95% CIs. d Noninferiority was met, as the lower bound of the two-sided 95% CI for the GMT ratio exceeded 0.67. e The SRR percentage was defined as percentage of participants at the post vaccination visit with a ≥ 4-fold rise from baseline if baseline was equal to or above LLOQ, or at least 4-fold rise from LLOQ if baseline was below LLOQ in antibody. The 95% CI for SRR was calculated using the Clopper-Pearson exact method. f Difference in SRR is the SRR in vaccine-naïve minus SRR in previously vaccinated. The 95% CI for the difference of SRR between groups was calculated with the method of Miettinen and Nurminen g Noninferiority was met, as the lower bound of the two-sided 95% CI for the SRR difference was > -10%. |
||
| Baseline GMT (95% CI) | 67.6 (56.8, 80.4) | 120.8 (101.5, 143.8) |
| Post-Vaccination Adjusted GMT (95% CI)c | 1491.5 (1277.5, 1741.4) | 841.4 (723.9, 978.0) |
| GMT Ratioc (95% CI) | 1.8d (1.4, 2.2) | |
| SRRe % (95% CI) | 74.3 (68.9, 79.3) | 64.3 (58.6, 69.6) |
| Difference in SRR % (95% CI)f | 10.0g (2.6, 17.4) | |
14.2 Adolescents 12 Years Through 17 Years of Age
Effectiveness of 2-Dose Series (Original Monovalent) in Vaccine-Naïve Adolescents
Effectiveness of a 2-dose series in adolescents 12 years through 17 years of age is based on a comparison of immune responses in this age group to adults 18 years through 25 years of age.
Study 1 adolescent expansion was a Phase 3 multicenter, randomized, observer-blinded, placebo-controlled, crossover study that included 2,247 participants 12 through 17 years of age at selected sites in the US from a diverse population including underserved minorities [see Adverse Reactions (6.1)]. Eligible participants were healthy or medically stable and had no history of previous laboratory-confirmed (by PCR or serology to SARS-CoV-2) diagnosis of SARS-CoV-2 infection or COVID-19 prior to randomization. SARS-CoV-2 PCR samples were tested by a central laboratory. The study excluded individuals who were significantly immunocompromised due to immunodeficiency disease; had received chronic immunosuppressive therapy or had received immunoglobulin or blood-derived products within 90 days; or had a history of laboratory-confirmed diagnosed COVID-19. Participants were enrolled without further stratification, although sites were instructed to recruit a similar number of participants in the 12 to < 15 years and 15 to < 18 years subgroups and randomized to Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) or placebo (normal saline) in a 2:1 ratio. A total of 2,247 participants were randomized to receive two doses of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) or placebo 21 days apart. Assessments of safety, immunogenicity, and efficacy against COVID-19 were conducted for up to 24 months after the second dose.
The primary analysis was conducted comparing SARS-CoV-2 neutralizing antibody titers 14 days after Dose 2 in a subset of adolescents 12 through 17 years of age to those of participants 18 through 25 years of age from the adult main study. In the adolescent subset, the median age was 14 years; 52.4% were male and 47.6% were female; 79.8% were White, 11.2% were Black or African American, 1.1% were American Indian or Alaskan Native, 0.2% were Native Hawaiian or Other Pacific Islander, 2.4% were Asian, 5.2% were Multiracial, and 0.2% did not report a race; 17.2% were Hispanic or Latino. In the adult subset, the median age was 22 years; 46.7% were male and 53.3% were female; 69.7% were White, 10.4% were Black or African American, 8.7% were American Indian or Alaskan Native, 0.5% were Native Hawaiian or Other Pacific Islander, 7.3% were Asian, 1.7% were Multiracial, 1.5% did not report a race, and race information was missing for 0.2%; 32.4% were Hispanic or Latino.
Noninferior immune responses as assessed by geometric mean titers and seroconversion rates were demonstrated in a comparison of adolescents 12 through 17 years of age to participants 18 through 25 years of age (see Table 11).
| Assay | Time Point | 12 Years Through 17 Years | 18 Years Through 25 Years | Analysis | Met Noninferiority Criteriac | |
|---|---|---|---|---|---|---|
| CI = Confidence interval; GMR = Geometric mean ratio; GMT = Geometric mean titer; SCR = Seroconversion rate a The 95% CI for GMT was calculated based on the t-distribution of the log-transformed values, then back transformed to the original scale for presentation. b GMR is defined as the ratio of two geometric mean titers for comparison of two age cohorts. An analysis of covariance (ANCOVA) with age cohort as main effect and baseline microneutralization assay neutralizing antibodies as covariate was performed to estimate the GMR. c Noninferiority was achieved if the following 3 pre-specified criteria were met simultaneously: 1) Upper limit of two-sided 95% CI for the ratio of GMTs (GMT12-17yo/GMT18-25yo) > 0.67; 2) Point estimate of the ratio of GMTs ≥ 0.82; and 3) Upper limit of the two-sided 95% CI for difference of SCRs (SCR12-17yo – SCR18-25yo) was > -10%. d Validated virus neutralizing assay (VNA) with wild-type virus (SARS-CoV-2 hCoV-19/Australia/VIC01/2020 [GenBank MT007544.1]; 360biolabs, Melbourne, Australia). The lower limit for quantification for this assay was a titer of 20, with titers below this level documented as 10. e The SCR percentage was defined as percentage of participants at the post vaccination visit with a >= 4-fold rise from baseline if baseline is equal to or above LLOQ, or at least 4-fold rise from LLOQ if baseline is below LLOQ in antibody. The 95% CI for SCR was calculated using the Clopper-Pearson exact method. f Difference in SCR in the pediatric expansion minus the SCR in the adult part of the study for 18 through 25-year-old. The 95% CI for the difference of SCR between groups was calculated with the method of Miettinen and Nurminen. |
||||||
| SARS-CoV-2 wild-type microneutralization assay (1/dilution)d | 14 days after Dose 2 | GMTa
(95% CI) n=466 | GMTa
(95% CI) n=413 | GMRb
(95% CI) | Yes | |
| 3791.2 (3411.6, 4213.1) | 2603.3 (2359.1, 2872.9) | 1.5 (1.3, 1.7)c | ||||
| SCR%e
(95% CI) n=461 | SCR%e
(95% CI) n=410 | Difference in
SCR%f (95% CI) |
||||
| 98.9 (97.5, 99.7) | 99.3 (97.9, 99.8) | -0.3 (-1.9, 1.2) |
||||
A descriptive efficacy analysis evaluating PCR-confirmed symptomatic mild, moderate, or severe COVID-19 cases was performed prior to the crossover period in 1,788 participants who were included in the per-protocol efficacy (PP-EFF) Analysis Set.
Vaccine efficacy in participants without evidence of SARS-CoV-2 infection through 6 days after the second dose is presented in Table 12. The efficacy of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) to prevent PCR-confirmed symptomatic mild, moderate, or severe COVID-19 from 7 days after Dose 2 was 79.8% (95% CI: 47.5%, 92.2%). All cases for which sequence data were available (vaccine n=3; placebo n=8) were due to the Delta variant. No cases of moderate or severe COVID-19 were reported in participants who received Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent). One moderate and no severe cases of COVID-19 were reported in participants who received placebo.
| Subgroup | Novavax COVID-19 Vaccine, Adjuvanted (Original Monovalent) | Placebo | Vaccine Efficacy (95% CI) (%) |
||||
|---|---|---|---|---|---|---|---|
| Participants N | COVID-19 Cases n (%) | Mean Incidence Rate Per 100 Person-Years | Participants N | COVID-19 Cases n (%) | Mean Incidence Rate Per 100 Person-Years | ||
| a Vaccine efficacy (VE) evaluated in participants without major protocol deviations who were seronegative (for SARS-CoV-2) at baseline and did not have a laboratory confirmed current SARS-CoV-2 infection with symptom onset through 6 days after the second dose, and who had received two doses of vaccine or placebo as randomized. b Based on Modified Poisson regression with logarithmic link function and treatment group as fixed effect and robust error variance (Zou 2004). c The definitions for mild, moderate, and severe COVID-19 disease used for the analysis of efficacy in adolescents 12 through 17 years of age were the same as those used for the assessment of efficacy in adults 18 years of age and older, with the exception of the inclusion of Multisystem Inflammatory Syndrome in Children (MIS-C) in the definition of severe COVID-19 disease for adolescents. |
|||||||
| Primary efficacy endpoint | |||||||
| All participants | 1,199 | 6 (0.5) | 2.9 | 590 | 14 (2.4) | 14.3 | 79.8 (47.5, 92.2)b |
| Mildc | – | 6 (0.5) | – | – | 13 (2.2) | – | – |
| Moderatec | 0 | 1 (0.2) | |||||
| Severec | 0 | 0 | |||||
Immunogenicity of a Single Dose (Original Monovalent) in Vaccine-Experienced Adolescents
Effectiveness of a booster dose of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) in vaccine-experienced adolescents was based on assessment of neutralizing antibody titers (MN50) against the original SARS-CoV-2 strain (SARS-CoV-2 hCoV-19/Australia/VIC01/2020). Immunogenicity analyses compared the MN50 titers following the booster dose with the MN50 titers following the primary series in participants who had data at both time points.
In the open-label booster dose phase of Study 1, participants 12 through 17 years of age received a single booster dose of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) at least 5 months after completion of the primary series. A subset of 56 participants were included in the per-protocol immunogenicity (PP-IMM) analysis set. The median age of participants in the PP-IMM analysis set was 14 years (range 12 to 17 years). Overall, 51.8% were male and 48.2% were female; 91.1% were White, 1.8% were Black or African American, 1.8% were Asian, and 5.4% were Multiracial; 17.9% were Hispanic or Latino.
Prespecified analyses of noninferior immunogenicity included an assessment of MN50 GMT ratio and difference in seroconversion rates. Seroconversion for a participant was defined as achieving a 4-fold rise in MN50 from baseline (before the first dose of the primary series).
The analysis of the GMT ratio of MN50 following the booster dose compared with the primary series met the noninferiority criteria for a booster dose response (lower limit of the 95% CI > 0.67) and point estimate > 0.83.
The analysis of the difference in seroconversion rates following the booster dose compared with the pre-primary series met the noninferiority criteria for a booster dose response (lower limit of the 95% CI > -10%). These analyses are summarized in Table 13.
| Assay | Time Point | Booster Dose n=56b | Primary Series n=56b | GMR (95% CI)c | Met Noninferiority Criteriag,h |
|---|---|---|---|---|---|
| GMT (95% CI)c | GMT (95% CI)c |
||||
| Abbreviations: CI = confidence interval; GMT = geometric mean titer; MN50 = microneutralization assay with an inhibitory concentration of 50%; PP-IMM = Per-Protocol Immunogenicity; SCR = seroconversion rate. a The PP-IMM Analysis Set included participants who received two doses (0.5 mL 21 days apart) of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) in the initial vaccination period , had an immunogenicity blood sample collected at Day 35 (primary series) and at 28 days after booster dose vaccination, did not have serologic or virologic evidence of SARS-CoV-2 infection on or before the booster dose, did not receive an emergency use authorized COVID-19 vaccine, received the booster dose, and remained blinded on study and without major protocol deviations until 7 days post-crossover Dose. b The analysis included a total of 56 participants of the PP-IMM analysis set who had immunogenicity data available for both the booster dose and primary series. c The 95% CI for GMT and GMT ratio were calculated based on the t-distribution of the log-transformed values, then back transformed to the original scale for presentation. d The 95% CI for SCR was based on the Clopper-Pearson method. e The difference in SCR was based on the Tango method. f Comparison between SCR of 28 days post-booster dose relative to time of first dose and SCR of 14 days after second dose of the primary series relative to time of first dose. g Noninferiority of the single booster dose was achieved if the lower limit of the 95% CI for the ratio of MN50 GMT at 28 days after a single booster dose versus 14 days after the second dose of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) was > 0.67 and point estimate > 0.83. h Noninferiority of the single booster dose was achieved if the lower limit of the 95% CI for the difference of the proportion of participants with SCR at 28 days after a single booster dose relative to the time of first vaccination versus at 14 days after the second dose of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent) relative to the time of first vaccination was > -10%. Note: The median duration between the time of the second dose of Novavax COVID-19 Vaccine, Adjuvanted (Original monovalent), and the time of the booster dose was 10.6 months. Note: SCR was defined as percentage of subjects with a ≥ 4-fold rise from baseline if the baseline value is equal to or above LLOQ, or at least 4-fold rise from LLOQ if the baseline value is below LLOQ in antibody concentration. |
|||||
| SARS-CoV-2 wild-type microneutralization assay (1/dilution) | 28 days after Booster Dose; 14 days after Primary Series Dose 2 | 12177.5 (9294.6, 15954.6) | 4305.4 (3543.7, 5230.7) | 2.8 (2.1, 3.8) | Yes |
| SCR% (95% CI)d | SCR% (95% CI)d | Difference in SCR%e (95% CI)f |
|||
| 100.0 (93.6, 100.0) | 100.0 (93.6, 100.0) | 0.0 (-6.4, 6.4) |
|||
16. How is Nuvaxovid supplied
NUVAXOVID is supplied as a pre-filled syringe (NDC 80631-207-01) containing 1 dose of 0.5 mL. Ten pre-filled syringes are supplied in a carton (NDC 80631-207-10).
Store in the original carton to protect from light.
Store in a refrigerator at 2°C to 8°C (36°F to 46°F).
Do not freeze.
17. Patient Counseling Information
Advise the vaccine recipient or caregiver to read the FDA-approved patient labeling.
Inform the vaccine recipient or caregiver of the potential benefits and risks of vaccination with NUVAXOVID.
Instruct the vaccine recipient or caregiver to report any adverse events to their healthcare provider or to the Vaccine Adverse Event Reporting System at 1-800-822-7967 and http://www.vaers.hhs.gov.
There is a pregnancy exposure registry for NUVAXOVID. Encourage individuals exposed to NUVAXOVID around the time of conception or during pregnancy to register by visiting https://c-viper.pregistry.com/.
novavax
Manufactured for:
Novavax, Inc.
Gaithersburg, MD 20878
©2025 Novavax, Inc. All rights reserved.
NUVAXOVID is a trademark of Novavax, Inc.
US License No. 2349
Revised: 8/2025
PRINCIPAL DISPLAY PANEL - NUVAXOVID 2025-2026 Formula - Carton
NDC 80631-207-10
novavax
COVID-19 Vaccine, Adjuvanted
NUVAXOVIDTM
2025-2026 Formula
For intramuscular use.
For 65 years of age and older
For people 12 through 64 years at high risk for severe COVID-19
10 single-dose pre-filled syringes
Each syringe contains 1 dose of 0.5 mL
Rx Only
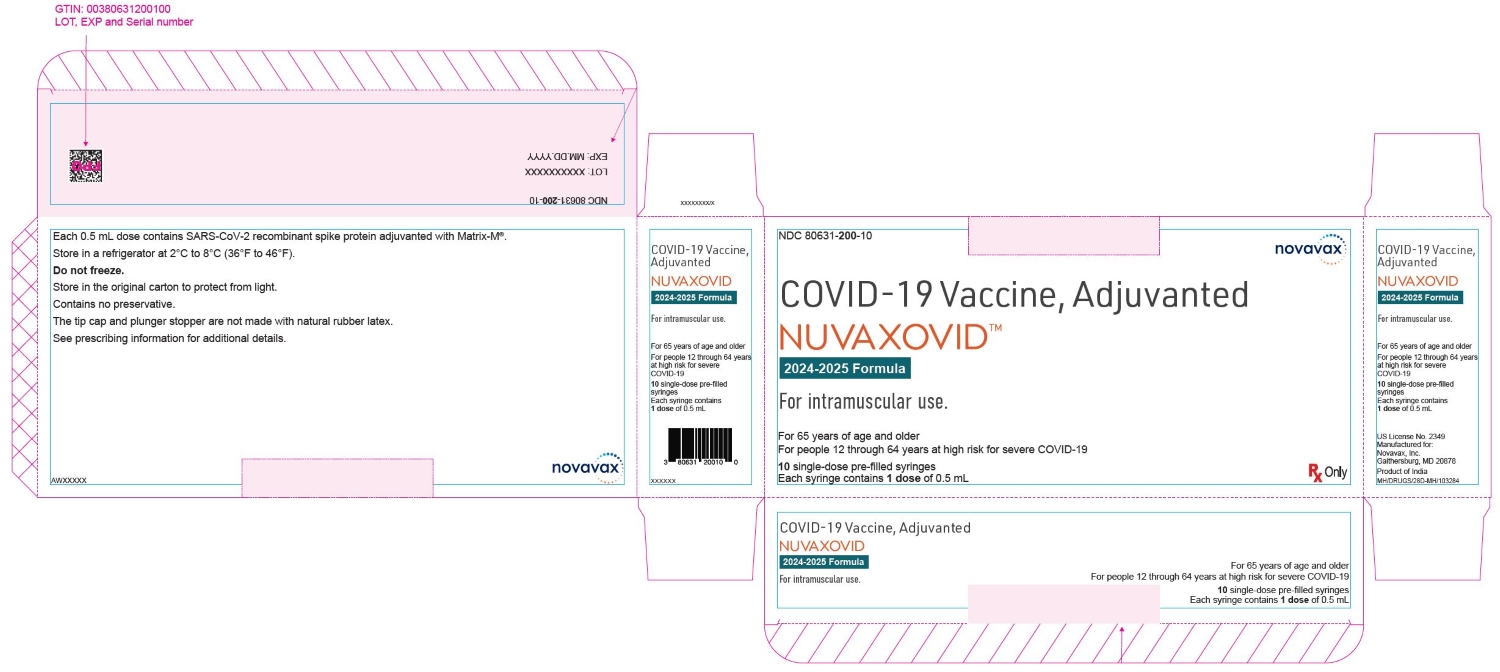
| NUVAXOVID COVID-19 VACCINE, ADJUVANTED
nvx-cov2705 injection, suspension |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| NUVAXOVID COVID-19 VACCINE, ADJUVANTED
nvx-cov2705 injection, suspension |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| Labeler - Novavax, Inc. (808837520) |
Frequently asked questions
More about Nuvaxovid (sars-cov-2 (covid-19) nvx-cov2705 vaccine, adjuvanted)
- Check interactions
- Compare alternatives
- Drug images
- Dosage information
- FDA approval history
- Drug class: viral vaccines