Biden Plan to Expand Obesity Drug Coverage Is Rejected
MONDAY, April 7, 2025 -- The Trump administration has decided not to expand Medicare and Medicaid coverage for popular obesity drugs, blocking a Biden administration initiative that could have helped millions of Americans access the medications.
Catherine Howden, a spokeswoman for the Centers for Medicare & Medicaid Services, said that expanding coverage for these drugs “is not appropriate at this time,” though it "may consider future policy options” for them.
The decision was included in a 438-page rule updating other parts of Medicare’s drug coverage.
Currently, Medicare covers these drugs only for people with diabetes, or in rare cases, for those who are obese and also have major heart problems or sleep apnea, The New York Times reported.
Former President Joe Biden's plan would have expanded access to people who are obese but do not have other health problems.
Officials estimated that about 3.4 million more people might start using the medications if coverage were expanded.
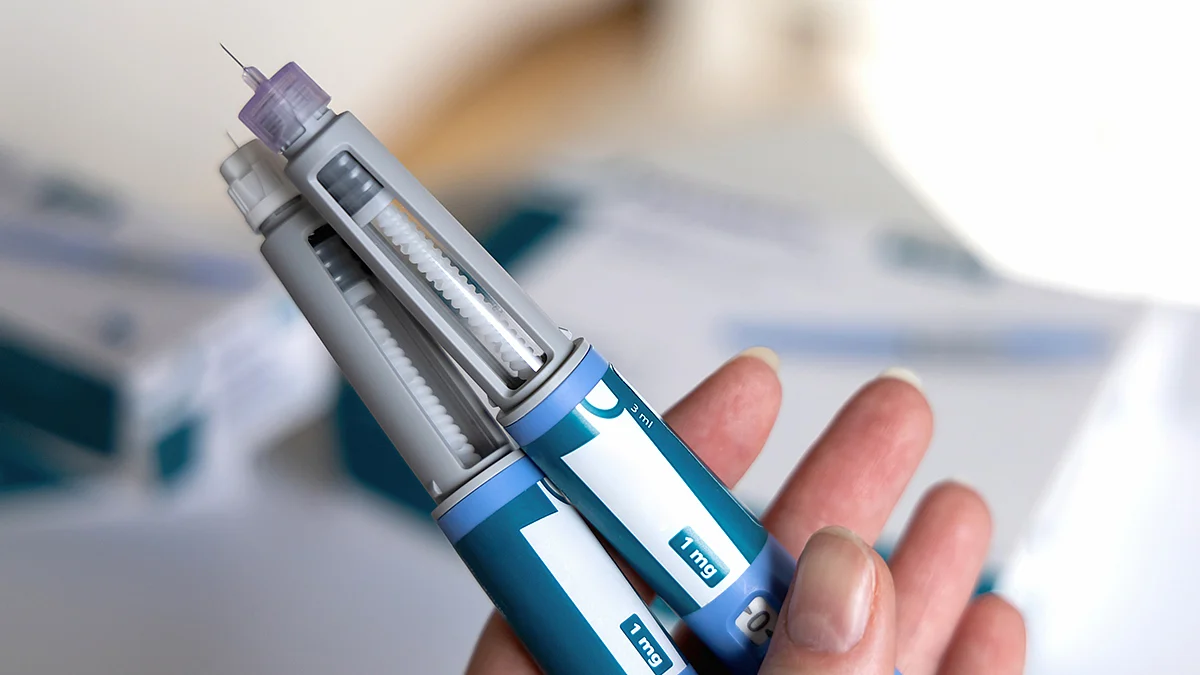
The drugs include Novo Nordisk’s Wegovy and Ozempic, and Eli Lilly’s Zepbound and Mounjaro. These medications have shown benefits beyond weight loss, such as lowering the risk of heart attacks and strokes.
But cost was a major concern. The Congressional Budget Office estimated that expanding coverage would cost the federal government around $35 billion over 10 years, The Times said.
Retail prices for the drugs range from $350 to $500 per month without insurance, according to The Times.
Compounded versions, made during shortages, have cost less than $200 -- but regulators plan to stop allowing those soon.
Some Medicaid programs already cover these drugs. Others don’t.
Proponents argue that the drugs would save money in the long run by preventing costly health issues. However, it’s still unclear whether those savings would actually happen.
Many private health plans also don’t cover these drugs. Some, like state employee plans in North Carolina and West Virginia, dropped coverage after demand and costs soared.
Sources
- The New York Times, April 4, 2025
Disclaimer: Statistical data in medical articles provide general trends and do not pertain to individuals. Individual factors can vary greatly. Always seek personalized medical advice for individual healthcare decisions.
© 2025 HealthDay. All rights reserved.
Read this next
Nearly Half Of People With Diabetes Unaware Of Their Illness
WEDNESDAY, Sept. 10, 2025 — Nearly half of people with diabetes around the world are unaware of their condition, according to a new study. Globally, an estimated 44% of...
Inactive Parents Tend To Have Couch Potato Kids
WEDNESDAY, Sept. 10, 2025 — Kids are more likely to become couch potatoes — or enthusiastically active — based on what they see their parents doing day-to-day, a...
WHO Updates List of Essential Medicines to Include GLP-1s
TUESDAY, Sept. 9, 2025 -- The World Health Organization published updated editions of its Model List of Essential Medicines (EML) and Essential Medicines for Children (EMLc) to...
More news resources
- FDA Medwatch Drug Alerts
- Daily MedNews
- News for Health Professionals
- New Drug Approvals
- New Drug Applications
- Drug Shortages
- Clinical Trial Results
- Generic Drug Approvals
Subscribe to our newsletter
Whatever your topic of interest, subscribe to our newsletters to get the best of Drugs.com in your inbox.