Vedolizumab (Monograph)
Brand name: Entyvio
Drug class: Disease-modifying Antirheumatic Drugs, Miscellaneous
Introduction
Recombinant humanized anti-α4β7-integrin monoclonal antibody; integrin receptor antagonist.1
Uses for Vedolizumab
Ulcerative Colitis
Treatment of moderately to severely active ulcerative colitis; used to induce and maintain clinical response and clinical remission, improve endoscopic appearance of mucosa, and achieve corticosteroid-free remission in adults with moderately to severely active disease.1 2 5 6 25 26 27 28
Guidelines recommend the use of vedolizumab as a first or second-line treatment for moderate to severe ulcerative colitis for induction and maintenance of remission.2018 2019 2020
Crohn Disease
Treatment of moderately to severely active Crohn disease; used to achieve clinical response, clinical remission, and corticosteroid-free remission in adults with moderately to severely active disease.1 12 14 26 28 30 31 32 38
Guidelines generally recommend use of other biologic agents including TNF inhibitors and ustekinumab over vedolizumab in patients with moderate to severe active Crohn disease.2000 2001
Vedolizumab Dosage and Administration
General
Pretreatment Screening
-
Ensure patient is up to date with all immunizations according to current immunization guidelines prior to initiating therapy.1
-
Treat underlying active, severe infections prior to initiating therapy.1
-
Perform a pregnancy test prior to initiating therapy in females of reproductive potential.1
Patient Monitoring
-
Monitor patients for signs and symptoms of infusion-related and hypersensitivity reactions (including anaphylaxis) during and after infusions.1
-
Monitor patients for progressive muscle weakness, vision disturbances, changes in memory and orientation, confusion, or personality changes.1
Other General Considerations
-
Aminosalicylates, corticosteroids, and immunosuppressive agents (azathioprine, mercaptopurine) were continued in clinical studies evaluating vedolizumab in patients with ulcerative colitis or Crohn disease.1 6 12
Administration
Administer by IV infusion.1 May be administered by sub-Q therapy after initial IV therapy.1
IV Administration
Administer by IV infusion over approximately 30 minutes.1
Do not mix with or administer through the same administration set with other drugs.1
Flush IV line with 30 mL of 0.9% sodium chloride injection or Lactated Ringer's injection after the infusion is complete.1
Lyophilized powder must be reconstituted at room temperature and diluted prior to administration.1
Reconstitution
Reconstitute vedolizumab lyophilized powder by adding 4.8 mL of sterile water for injection, 0.9% sodium chloride injection, or Lactated Ringers injection (using a syringe with a 21- to 25-gauge needle) to a 300-mg vial to provide a solution containing 60 mg/mL.1 Direct diluent toward wall of vial to avoid excessive foaming.1
Gently swirl vial for at least 15 seconds to dissolve powder.1 Do not shake vigorously or invert.1 Allow solution to stand for up to 20 minutes at room temperature to allow for reconstitution and for any foam to settle.1 Vial can be swirled and inspected for dissolution during this time.1 If not fully dissolved within 20 minutes, allow an additional 10 minutes.1 Do not use vial if drug is not dissolved within 30 minutes.1
May refrigerate reconstituted solution in vial for up to 8 hours prior to further dilution; however, maximum storage time for reconstituted solution in vial may be limited by diluent selected to prepare the final infusion solution.1
Dilution
Gently invert vial 3 times, then immediately withdraw 5 mL (300 mg) of reconstituted solution (using a syringe with a 21- to 25-gauge needle).1 Add the reconstituted solution to an infusion bag containing 250 mL of 0.9% sodium chloride injection or Lactated Ringer's injection and mix gently.1
Storage time for diluted solution depends on storage conditions and diluent.1
Discard any unused portions of reconstituted or diluted solutions.1
Rate of Administration
Administer by IV infusion over approximately 30 minutes.1
Sub-Q Administration
May switch patients from IV to sub-Q therapy at week 6 after the first 2 IV doses have been administered at week 0 and week 2; also may switch from IV to sub-Q therapy in patients who receive and respond to IV therapy beyond week 6.1
To switch to sub-Q therapy, administer the first sub-Q dose in place of the next scheduled IV infusion and then every 2 weeks thereafter.1
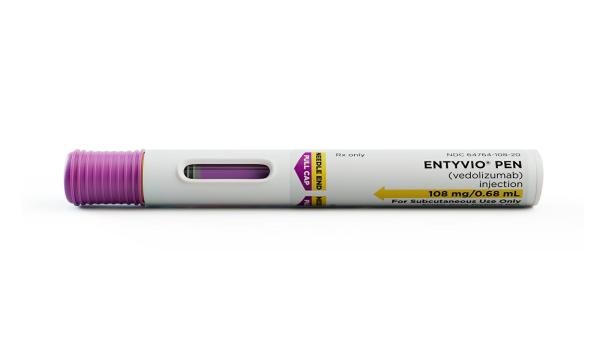
Available in single-use prefilled syringes and single-use prefilled pens.1
Patients or caregivers may administer sub-Q injections using either the prefilled syringe or pen after appropriate training is provided.1
Administer each sub-Q injection at a different anatomic location (such as thighs, any quadrant of abdomen, or upper arms.1 Do not inject into moles, scars, bruises, or areas where the skin is tender, erythematous, or indurated.1
If treatment is interrupted or if a scheduled dose(s) is missed, inject the next sub-Q dose as soon as possible and then every 2 weeks thereafter.1 In the event of incomplete dose administration (i.e., patient attempts administration of dose with the pen, however it is uncertain if a full dose was administered), instruct patient to call their pharmacy or healthcare provider.1
Dosage
Adults
Ulcerative Colitis
IV
300 mg at 0, 2, and 6 weeks and then every 8 weeks thereafter.1
Discontinue if no therapeutic benefit is evident by week 14 of therapy.1
Sub-Q
Following administration of the first 2 IV doses at week 0 and week 2, may administer by sub-Q injection at a dose of 108 mg at week 6 and then once every 2 weeks thereafter.1
Discontinue therapy if no therapeutic benefit is evident by week 14 of therapy.1
Crohn Disease
IV
300 mg at 0, 2, and 6 weeks and then every 8 weeks thereafter.1
Discontinue if no therapeutic benefit is evident by week 14 of therapy.1
Sub-Q
Following administration of the first 2 IV doses at week 0 and week 2, may administer by sub-Q injection at a dose of 108 mg at week 6 and then once every 2 weeks thereafter.1
Discontinue therapy if no therapeutic benefit is evident by week 14 of therapy.1
Special Populations
Hepatic Impairment
Manufacturer makes no specific dosage recommendations.1
Renal Impairment
Manufacturer makes no specific dosage recommendations.1
Geriatric Patients
Manufacturer makes no specific dosage recommendations.1
Cautions for Vedolizumab
Contraindications
-
Known history of serious or severe hypersensitivity reaction (e.g., dyspnea, bronchospasm, urticaria, flushing, rash, increased heart rate) to the drug or any ingredient in the formulation.1
Warnings/Precautions
Infusion-related and Hypersensitivity Reactions
Infusion-related and hypersensitivity reactions, including anaphylaxis, dyspnea, bronchospasm, urticaria, flushing, rash, and increased BP and heart rate, reported.1 5 6 12 14 Infusion-related reactions also may include nausea, headache, pruritus, dizziness, fatigue, pyrexia, and vomiting.1
Reactions may occur with the first infusion or with subsequent infusions; time of onset may be variable (during or up to several hours after an infusion).1
Clinicians should be prepared to treat hypersensitivity and infusion-related reactions.1 Ensure appropriate equipment and agents for treating such reactions are available for immediate use, and monitor patient until infusion is completed.1 If anaphylaxis or other serious infusion-related or hypersensitivity reactions occur, immediately discontinue the infusion and initiate appropriate treatment.1
In clinical trials, patients who experienced a mild infusion-related or hypersensitivity reaction to the drug could receive premedication (e.g., antihistamine, hydrocortisone, and/or acetaminophen) prior to subsequent infusions.1
Infections
Increased risk of infections.1 Most common infections are nasopharyngeal and upper respiratory tract infections.1 5 6 12 14 However, serious infections (e.g., anal abscess, sepsis [sometimes fatal], tuberculosis, Salmonella sepsis, Listeria meningitis, giardiasis, cytomegaloviral colitis) also reported, more commonly in patients with Crohn disease than in those with ulcerative colitis.1 14
Delay initiation of vedolizumab until any active severe infection has been controlled.1 If severe infection develops during therapy, consider interrupting vedolizumab therapy.1
Exercise caution when considering use in patients with a history of recurring severe infections.1
Consider screening for active or latent tuberculosis infection.1
Progressive Multifocal Leukoencephalopathy (PML)
PML, an opportunistic infection of the brain caused by the JC virus, reported in patients receiving systemic immunosuppressive agents, including natalizumab, an anti-α4-integrin monoclonal antibody.1 20 PML generally occurs only in immunocompromised patients and usually progresses to death or severe disability.1 Also reported during postmarketing experience in a vedolizumab-treated patient with multiple contributory factors (e.g., HIV infection with CD4+ T-cell count of 300 cells/mm3 and prior and concomitant immunosuppression).1 Although considered unlikely, risk of PML in vedolizumab-treated patients cannot be ruled out.1
Monitor for any new or worsening neurologic manifestations.1 If PML is suspected, withhold drug and refer patient to a neurologist.1 Permanently discontinue if PML is confirmed.1
Liver Injury
Increases in serum ALT and AST concentrations and/or bilirubin concentrations, including several cases of hepatitis, reported following 2–5 doses of the drug; unclear whether reactions were drug induced or autoimmune.1 All patients recovered following drug discontinuance, although some patients also required corticosteroid treatment.1
Discontinue vedolizumab in patients with jaundice or other evidence of clinically significant hepatic injury.1
Live and Oral Vaccines
Administer all appropriate vaccines as recommended by current immunization guidelines prior to initiation of vedolizumab.1
Patients receiving vedolizumab may receive inactive vaccines (e.g., parenteral influenza virus vaccine inactivated) and may receive live vaccines if potential benefits justify possible risks.1
Malignancies
Malignancies (excluding dysplasia and basal cell carcinoma) reported during clinical trials in ulcerative colitis or Crohn disease.1 Malignancies also reported during extension phases of the trials; however, data regarding effects of long-term exposure to the drug are limited.1
Immunogenicity
Formation of antibodies, including neutralizing antibodies, to vedolizumab reported.1 Presence of persistently positive anti-vedolizumab antibodies associated with undetectable or negligible serum concentrations of the drug and failure to achieve clinical remission.1
Specific Populations
Pregnancy
Available data in pregnant women have not reliably identified a vedolizumab-associated risk of major birth defects, spontaneous abortion, or adverse maternal or fetal outcomes.1
Increased disease activity in women with inflammatory bowel disease may increase the risk of adverse pregnancy outcomes (e.g., preterm delivery, low birth weight, small size for gestational age at birth).1
Use during pregnancy could affect immune responses in neonates and infants exposed to the drug in utero.1 Clinical importance of low concentrations of the drug in infants exposed in utero is unknown.1 Safety of administering live vaccines to infants exposed to the drug in utero also is unknown.1
Lactation
Vedolizumab distributes into human milk in low concentrations.1 23 24 Effects on nursing infants, including potential effects of local GI exposure or systemic exposure (expected to be low), are unknown; effects on milk production also unknown.1
Consider developmental and health benefits of breast-feeding along with the mother's clinical need for vedolizumab and any potential adverse effects on the breast-fed infant from the drug or underlying maternal condition.1
Pediatric Use
Safety and efficacy not established in pediatric patients.1
Geriatric Use
Insufficient experience in patients ≥65 years of age to determine whether geriatric patients respond differently than younger adults; however, no overall differences in efficacy and safety observed.1
Hepatic Impairment
No specific information available from the manufacturer.1
Renal Impairment
No specific information available from the manufacturer.1
Common Adverse Effects
Most common adverse reactions (≥3%): Nasopharyngitis, headache, arthralgia, nausea, pyrexia, upper respiratory tract infection, fatigue, cough, bronchitis, influenza, back pain, rash, pruritus, sinusitis, oropharyngeal pain, pain in extremities.1
Adverse effects with sub-Q vedolizumab are similar to those reported with IV vedolizumab with the exception of injection site reactions with sub-Q vedolizumab.1
Drug Interactions
CYP450 Substrates
Formation of CYP450 enzymes may be suppressed by increased levels of certain cytokines during chronic inflammation.1 Upon initiation or discontinuation of vedolizumab in patients treated with CYP450 substrates, monitor drug concentrations or other therapeutic parameters, and adjust dosage of the substrate as needed.1
Vaccines
Inactivated vaccines: Effect of vedolizumab on immune responses to oral or intranasal vaccines other than IM hepatitis B vaccine and oral inactivated cholera vaccine is not known.1 Manufacturer states patients receiving vedolizumab may receive inactivated vaccines.1
Live vaccines: No data on secondary transmission of infection by live vaccines in patients receiving vedolizumab.1 Manufacturer states patients receiving vedolizumab may receive live vaccines if potential benefits justify possible risks.1
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Cholera vaccine, oral inactivated |
Single vedolizumab dose given 4 days before initiation of immunization series reduced seroconversion rate and titers of antibody to cholera toxin1 21 |
May be used concomitantly1 |
|
Hepatitis B vaccine |
Single vedolizumab dose given 4 days before initiation of IM immunization series did not affect seroconversion rate1 21 |
May be used concomitantly1 |
|
Influenza virus vaccine inactivated |
May be used concomitantly1 |
|
|
Natalizumab |
Increased risk of PML and other infections1 |
Avoid concomitant use1 |
|
Tumor necrosis factor (TNF) blocking agents |
Increased risk of infections1 |
Avoid concomitant use1 |
Vedolizumab Pharmacokinetics
Absorption
Bioavailability
108 mg single-dose sub-Q injection compared to a 300 mg single-dose IV infusion in healthy subjects approximately 75%.1
Distribution
Extent
Not known whether vedolizumab distributes into human milk.1
Not detected in CSF at 5 weeks after single IV dose (450 mg).1
Elimination
Half-life
Approximately 25 days at 300-mg dose.1
Clearance dependent on linear and nonlinear pathways; nonlinear clearance decreases with increasing concentrations.1
Special Populations
Pharmacokinetics similar in patients with ulcerative colitis and those with Crohn disease.1
Pharmacokinetics not formally studied in patients with renal or hepatic impairment.1
Disease severity, body weight, prior treatment with TNF blocking agents, age (within range of 18–78 years), serum albumin concentration, and concomitant therapy (azathioprine, mercaptopurine, methotrexate, aminosalicylates) did not have a clinically meaningful effect on pharmacokinetics.1
Presence of persistently positive anti-vedolizumab antibodies may reduce serum vedolizumab concentrations to undetectable or negligible levels.1
Stability
Storage
Parenteral
Powder for IV Infusion
2–8°C.1 Keep in original package to protect from light.1
Reconstituted solution
Reconstituted solution in vial: 2–8°C for up to 8 hours (but may be limited by diluent selected to prepare the final infusion solution).1 Do not freeze.1
Diluted solution
Infusion solution (in 0.9% sodium chloride): 2–8°C for up to 24 hours (may include up to 12 hours at room temperature) or 20–25°C for up to 12 hours; these storage times include any time that the reconstituted solution was refrigerated prior to dilution.1
Infusion solution (in Lactated Ringer's injection): 2–8°C for up to 6 hours (including any time that the reconstituted solution was refrigerated prior to dilution); if not refrigerated, use immediately after dilution.1 Do not freeze.1
Prefilled syringe or pen for sub-Q injection
2–8°C.1 Keep in original carton to protect from light.1
May store in the original package at room temperature up to 25°C for up to 7 days (for example, when traveling).1 Do not use if left out of refrigerator for more than 7 days.1
Actions
-
Binds specifically to α4β7 integrin, a protein expressed on the surface of a small subset of memory T-lymphocytes that preferentially migrate into the GI tract.1 2 4 5 6 7 8 9 10 12 13 14 15 16 Binding of vedolizumab to α4β7 integrin blocks interaction of α4β7 integrin with mucosal addressin cell adhesion molecule-1 (MAdCAM-1), which is expressed mainly on vascular endothelial cells in the GI tract, and inhibits migration of memory T-lymphocytes across the endothelium into inflamed GI parenchymal tissue.1 5 8
-
Interaction of α4β7 integrin with MAdCAM-1 implicated as an important contributor to the chronic inflammation of ulcerative colitis and Crohn disease.1
-
Does not bind to or inhibit the function of α4β1 and αEβ7 integrins; does not antagonize the interaction of α4 integrins with vascular cell adhesion molecule-1 (VCAM-1).1
-
Appears to exert a more selective effect on the GI tract than does natalizumab, which binds to α4 subunits of α4β1 and α4β7 integrins expressed on the surface of all leukocytes except neutrophils.7 8 16 20
Advice to Patients
-
Provide patients with a copy of the manufacturer's patient information (medication guide).1
-
Risk of hypersensitivity reaction. Instruct patients to immediately report symptoms consistent with a hypersensitivity reaction (e.g., rash, pruritus, shortness of breath or difficulty breathing, wheezing, dizziness, flushing, palpitations, swelling of the lips, tongue, throat, or face) that occur during or following an infusion of vedolizumab.1
-
Risk of infection. Advise patients that they may be more likely to develop infections while receiving vedolizumab.1 Instruct patients to inform a clinician if they develop any signs or symptoms of infection (e.g., fever, chills, cough, dyspnea, fatigue, red or painful skin or sores, myalgia, rhinorrhea, sore throat, pain on urination) while receiving vedolizumab.1
-
Risk of progressive multifocal leukoencephalopathy. Inform patients that progressive multifocal leukoencephalopathy (PML) has occurred in patients receiving some integrin receptor antagonist and systemic immunosuppressive agents.1 Instruct patients to report any new or worsening neurologic manifestations (e.g., progressive weakness on one side of the body or clumsiness of limbs; changes in speech or walking; vision changes; changes in thinking, memory, and orientation leading to confusion and personality changes) immediately to their clinician.1
-
Risk of liver injury. Inform patients that increased serum aminotransferase (ALT and AST) concentrations with or without elevated bilirubin concentrations have occurred in patients who received vedolizumab.1 Advise patients to promptly report any symptoms suggestive of hepatic injury (e.g., fatigue, anorexia, right upper abdominal discomfort, dark urine, jaundice) while receiving vedolizumab.1
-
Advise patients to review their vaccination status with their clinician and receive all appropriate vaccines prior to initiation of vedolizumab therapy.1
-
Instruct patients and caregivers on proper sub-Q administration technique, and on the correct use of the vedolizumab single-dose prefilled syringe or single-dose prefilled pen.1
-
Advise patients to inform clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements, as well as any concomitant illnesses (e.g., hepatic disease, tuberculosis or other infection) or any history of recurrent infections.1
-
Advise females to inform their clinician if they are or plan to become pregnant or plan to breast-feed.1
-
Advise patients to inform their clinician of other important precautionary information.1
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
Vedolizumab can only be obtained through designated specialty pharmacies.37 Contact the manufacturer or consult the Entyvio website ([Web]) for specific information.37
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
For injection, for IV infusion |
300 mg |
Entyvio (available as single-dose vials) |
Takeda |
|
Injection, for subcutaneous use |
108 mg/0.68 mL |
Entyvio (available as a single-dose prefilled syringe and single-dose prefilled pen) |
Takeda |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions November 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
References
1. Takeda Pharmaceuticals, Inc. Entyvio(vedolizumab) injection prescribing information. Deerfield, IL; 2024 Apr.
2. Bickston SJ, Behm BW, Tsoulis DJ et al. Vedolizumab for induction and maintenance of remission in ulcerative colitis. Cochrane Database Syst Rev. 2014; 8:CD007571.
3. Danese S, Fiorino G, Peyrin-Biroulet L et al. Biological agents for moderately to severely active ulcerative colitis: a systematic review and network meta-analysis. Ann Intern Med. 2014; 160:704-11. https://pubmed.ncbi.nlm.nih.gov/24842416
4. . Induction and maintenance therapy with vedolizumab, a novel biologic therapy for ulcerative colitis. Gastroenterol Hepatol (N Y). 2014; 10:64-6. https://pubmed.ncbi.nlm.nih.gov/24799843
5. Feagan BG, Greenberg GR, Wild G et al. Treatment of ulcerative colitis with a humanized antibody to the alpha4beta7 integrin. N Engl J Med. 2005; 352:2499-507. https://pubmed.ncbi.nlm.nih.gov/15958805
6. Feagan BG, Rutgeerts P, Sands BE et al. Vedolizumab as induction and maintenance therapy for ulcerative colitis. N Engl J Med. 2013; 369:699-710. https://pubmed.ncbi.nlm.nih.gov/23964932
7. Gilroy L, Allen PB. Is there a role for vedolizumab in the treatment of ulcerative colitis and Crohn's disease?. Clin Exp Gastroenterol. 2014; 7:163-72. https://pubmed.ncbi.nlm.nih.gov/24899819
8. Gledhill T, Bodger K. New and emerging treatments for ulcerative colitis: a focus on vedolizumab. Biologics. 2013; 7:123-30. https://pubmed.ncbi.nlm.nih.gov/23723689
9. McLean LP, Shea-Donohue T, Cross RK. Vedolizumab for the treatment of ulcerative colitis and Crohn's disease. Immunotherapy. 2012; 4:883-98. https://pubmed.ncbi.nlm.nih.gov/23046232
10. . Vedolizumab (Entyvio) for inflammatory bowel disease. Med Lett Drugs Ther. 2014; 56:86-8. https://pubmed.ncbi.nlm.nih.gov/25211302
11. Reenaers C, Louis E, Belaiche J. Current directions of biologic therapies in inflammatory bowel disease. Therap Adv Gastroenterol. 2010; 3:99-106. https://pubmed.ncbi.nlm.nih.gov/21180594
12. Sandborn WJ, Feagan BG, Rutgeerts P et al. Vedolizumab as induction and maintenance therapy for Crohn's disease. N Engl J Med. 2013; 369:711-21. https://pubmed.ncbi.nlm.nih.gov/23964933
13. Sandborn WJ. Highlights in Crohn's Disease and Ulcerative Colitis: Digestive Disease Week 2012. Gastroenterol Hepatol (N Y). 2012; 8(8 Suppl 5):1-24. https://pubmed.ncbi.nlm.nih.gov/24847181
14. Sands BE, Feagan BG, Rutgeerts P et al. Effects of vedolizumab induction therapy for patients with Crohn's disease in whom tumor necrosis factor antagonist treatment failed. Gastroenterology. 2014; 147:618-627.e3. https://pubmed.ncbi.nlm.nih.gov/24859203
15. Seo GS, Chae SC. Biological therapy for ulcerative colitis: An update. World J Gastroenterol. 2014; 20:13234-13238. https://pubmed.ncbi.nlm.nih.gov/25309060
16. Soler D, Chapman T, Yang LL et al. The binding specificity and selective antagonism of vedolizumab, an anti-alpha4beta7 integrin therapeutic antibody in development for inflammatory bowel diseases. J Pharmacol Exp Ther. 2009; 330:864-75. https://pubmed.ncbi.nlm.nih.gov/19509315
17. Parikh A, Fox I, Leach T et al. Long-term clinical experience with vedolizumab in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2013; 19:1691-9. https://pubmed.ncbi.nlm.nih.gov/23591599
18. Parikh A, Leach T, Wyant T et al. Vedolizumab for the treatment of active ulcerative colitis: a randomized controlled phase 2 dose-ranging study. Inflamm Bowel Dis. 2012; 18:1470-9. https://pubmed.ncbi.nlm.nih.gov/22147460
19. Feagan BG, Greenberg GR, Wild G et al. Treatment of active Crohn's disease with MLN0002, a humanized antibody to the alpha4beta7 integrin. Clin Gastroenterol Hepatol. 2008; 6:1370-7. https://pubmed.ncbi.nlm.nih.gov/18829392
20. Biogen Idec Inc. Tysabri (natalizumab) injection prescribing information. Cambridge, MA; 2023 Oct.
21. Wyant T, Leach T, Sankoh S et al. Vedolizumab affects antibody responses to immunisation selectively in the gastrointestinal tract: randomised controlled trial results. Gut. 2015; 64:77-83. https://pubmed.ncbi.nlm.nih.gov/24763133
22. US Food and Drug Administration. Center for Drug Evaluation and Research. Application number 125476Orig1s000: Summary review. From FDA website. http://www.accessdata.fda.gov/drugsatfda_docs/nda/2014/125476Orig1s000SumR.pdf
23. Lahat A, Shitrit AB, Naftali T et al. Vedolizumab Levels in Breast Milk of Nursing Mothers With Inflammatory Bowel Disease. J Crohns Colitis. 2018; 12:120-123. https://pubmed.ncbi.nlm.nih.gov/28961712
24. Julsgaard M, Kjeldsen J, Bibby BM et al. Vedolizumab Concentrations in the Breast Milk of Nursing Mothers With Inflammatory Bowel Disease. Gastroenterology. 2018; 154:752-754.e1. https://pubmed.ncbi.nlm.nih.gov/28988916
25. Feagan BG, Patel H, Colombel JF, et al. Effects of vedolizumab on health-related quality of life in patients with ulcerative colitis: results from the randomised GEMINI 1 trial. Aliment Pharmacol Ther. 2017;45(2):264-275.
26. Yajnik V, Khan N, Dubinsky M, et al. Efficacy and safety of vedolizumab in ulcerative colitis and crohn's disease patients stratified by age. Adv Ther. 2017;34(2):542-559.
27. Loftus EV Jr, Colombel JF, Feagan BG, et al. Long-term efficacy of vedolizumab for ulcerative colitis. J Crohns Colitis. 2017;11(4):400-411.
28. Loftus EV Jr, Feagan BG, Panaccione R, et al. Long-term safety of vedolizumab for inflammatory bowel disease. Aliment Pharmacol Ther. 2020;52(8):1353-1365.
29. Sands BE, Peyrin-Biroulet L, Loftus EV Jr, et al; VARSITY Study Group. Vedolizumab versus adalimumab for moderate-to-severe ulcerative colitis. N Engl J Med. 2019;381(13):1215-1226.
30. Sands BE, Sandborn WJ, Van Assche G, et al. Vedolizumab as induction and maintenance therapy for crohn's disease in patients naïve to or who have failed tumor necrosis factor antagonist therapy. Inflamm Bowel Dis. 2017;23(1):97-106.
31. Vermeire S, Loftus EV Jr, Colombel JF, et al. Long-term efficacy of vedolizumab for Crohn's disease. J Crohns Colitis. 2017;11(4):412-424.
32. Danese S, Sandborn WJ, Colombel JF, et al. Endoscopic, radiologic, and histologic healing with vedolizumab in patients with active Crohn's disease. Gastroenterology. 2019;157(4):1007-1018.e7.
33. Food and Drug Administration. Search orphan drug designations and approvals. From FDA website. Accessed 2024 Oct 14. https://www.accessdata.fda.gov/scripts/opdlisting/oopd/listResult.cfm
34. Fløisand Y, Schroeder MA, Chevallier P, et al. A phase 2a randomized clinical trial of intravenous vedolizumab for the treatment of steroid-refractory intestinal acute graft-versus-host disease. Bone Marrow Transplant. 2021;56(10):2477-2488.
35. Chen YB, Shah NN, Renteria AS, et al. Vedolizumab for prevention of graft-versus-host disease after allogeneic hematopoietic stem cell transplantation. Blood Adv. 2019;3(23):4136-4146.
36. Danylesko I, Bukauskas A, Paulson M, et al. Anti-α4β7 integrin monoclonal antibody (vedolizumab) for the treatment of steroid-resistant severe intestinal acute graft-versus-host disease. Bone Marrow Transplant. 2019;54(7):987-993.
37. Takeda Pharmaceuticals Inc. Reference Toolkit for Accessing Entyvio. Accessed October 14, 2024. https://www.entyviohcp.com/Content/pdf/Entyvio-Reimbursement-Toolkit.pdf
38. Vermiere S, D'Haens G, Baert F, et al. Efficacy and safety of subcutaneous vedolizumab in patients with moderately to severely active Crohn's disease: results from the VISIBLE 2 randomised trial. J Crohn Colitis. 2022;16(1):27-38.
2000. Lichtenstein GR, Loftus EV, Isaacs KL, Regueiro MD, Gerson LB, Sands BE. ACG clinical guideline: management of crohn's disease in adults. Am J Gastroenterol. 2018;113(4):481-517. doi: 10.1038/ajg.2018.27
2001. Feuerstein JD, Ho EY, Shmidt E, et al; American Gastroenterological Association Institute Clinical Guidelines Committee. AGA clinical practice guidelines on the medical management of moderate to severe luminal and perianal fistulizing crohn's disease. Gastroenterology. 2021;160(7):2496-2508. doi: 10.1053/j.gastro.2021.04.022
2002. . Nguyen GC, Loftus EV Jr, Hirano I, et al. American Gastroenterological Association Institute guideline on the management of Crohn disease after surgical resection. Gastroenterology. 2017;152(1):271-275. https://pubmed.ncbi.nlm.nih.gov/27840074
2018. . Ko CW, Singh S, Feuerstein JD, Falck-Ytter C, Falck-Ytter Y, Cross RK; American Gastroenterological Association Institute Clinical Guidelines Committee. AGA clinical practice guidelines on the management of mild-to-moderate ulcerative colitis. Gastroenterology. 2019;156(3):748-764.
2019. . Feuerstein JD, Isaacs KL, Schneider Y, Siddique SM, Falck-Ytter Y, Singh S; AGA Institute Clinical Guidelines Committee. AGA clinical practice guidelines on the management of moderate to severe ulcerative colitis. Gastroenterology. 2020;158(5):1450-1461.
2020. . Rubin DT, Ananthakrishnan AN, Siegel CA, Sauer BG, Long MD. ACG clinical guideline: ulcerative colitis in adults. Am J Gastroenterol. 2019;114(3):384-413.
Biological Products Related to vedolizumab
Find detailed information on biosimilars for this medication.
Frequently asked questions
- How much does Entyvio cost per month?
- Is Entyvio an immunosuppressant or a biologic?
- Can I take antibiotics while on Entyvio?
- How long has Entyvio been on the market?
- Does Medicaid cover Entyvio?
- Is Entyvio used to treat Crohn’s disease?
More about vedolizumab
- Check interactions
- Compare alternatives
- Reviews (185)
- Side effects
- Dosage information
- During pregnancy
- Drug class: selective immunosuppressants
- Breastfeeding
- En español