Pretomanid (Monograph)
Drug class: Antituberculosis Agents
VA class: AM500
Introduction
Antituberculosis agent; nitroimidazooxazine antimycobacterial.
Uses for Pretomanid
Tuberculosis
Treatment of extensively drug resistant (XDR) pulmonary tuberculosis (i.e., caused by Mycobacterium tuberculosis resistant to isoniazid, rifampin, any fluoroquinolone, and at least one injectable antituberculosis agent) or treatment-intolerant or non-responsive multidrug-resistant (MDR) pulmonary tuberculosis (i.e., caused by M. tuberculosis resistant to isoniazid and rifampin); used in conjunction with bedaquiline and linezolid. Designated an orphan drug by FDA for this use.
FDA approval for treatment of XDR and treatment-intolerant or non-responsive MDR tuberculosis was based on limited clinical safety and efficacy data; use only in this specific, limited patient population.
Must be used in conjunction with bedaquiline and linezolid; safety and efficacy of pretomanid in conjunction with other drugs used for treatment of tuberculosis not established.
Safety and efficacy for treatment of drug-susceptible tuberculosis, latent tuberculosis infection, extrapulmonary tuberculosis, or MDR tuberculosis that is not treatment-intolerant or non-responsive to standard therapy not established.
WHO states that the 3-drug regimen of pretomanid, bedaquiline, and linezolid (also known as BPaL) may be used for treatment of MDR tuberculosis in patients who have not previously received either bedaquiline or linezolid (or received the drugs for ≤2 weeks) and have documented evidence that the MDR strain also is resistant to a fluoroquinolone.
Patients with MDR or XDR tuberculosis are at high risk for treatment failure and acquisition of further drug resistance. ATS, CDC, and IDSA recommend that such patients be referred to or that consultation be obtained from a specialized treatment center as identified by local or state health departments or the CDC.
For additional information on treatment of MDR and XDR tuberculosis, consult current guidelines from ATS/CDC/IDSA and WHO.
Pretomanid Dosage and Administration
General
-
Must be used in conjunction with bedaquiline and linezolid; do not use pretomanid alone.
-
Prior to initiating the 3-drug combination regimen, perform laboratory tests to evaluate liver function and assess for signs and symptoms of liver disease. (See Hepatotoxicity under Cautions.)
-
Obtain CBCs prior to, at 2 weeks, and then monthly during therapy. Assess serum electrolyte concentrations and perform ECGs prior to initiating therapy. (See Cautions.)
Administration
Oral Administration
Administer orally with food. Swallow tablets whole with water.
Administer the combination regimen of pretomanid, bedaquiline, and linezolid using directly observed (supervised) therapy (DOT).
If the combination regimen is interrupted for safety reasons, the missed doses of the drugs may be taken at the end of treatment; however, if dose(s) of linezolid are missed because of linezolid-associated adverse reactions, the missed dose(s) should not be made up.
Dosage
Adults
Active Tuberculosis
XDR or Treatment-intolerant or Non-responsive MDR Pulmonary Tuberculosis
Oral200 mg once daily.
Must administer in conjunction with oral bedaquiline (400 mg once daily for 2 weeks followed by 200 mg 3 times weekly [with at least 48 hours between doses] for 24 weeks) and oral linezolid (1.2 g daily for 26 weeks). Adjustment of linezolid dosage to 600 mg daily with further reductions to 300 mg daily or interruption of linezolid therapy may be required if myelosuppression, peripheral neuropathy, or optic neuropathy occurs. (See Cautions.)
The 3-drug combination regimen should be continued for 26 weeks, but may be extended beyond 26 weeks if necessary. In a clinical trial, the combination regimen was continued for 39 weeks in a few patients.
Dosage Modification for Toxicity
If linezolid is permanently discontinued during the first 4 weeks of therapy, also discontinue pretomanid and bedaquiline. If linezolid is permanently discontinued after the first 4 weeks of therapy, pretomanid and bedaquiline may be continued.
If pretomanid or bedaquiline is permanently discontinued, discontinue entire 3-drug combination regimen.
Hepatotoxicity
OralIf ALT or AST concentrations elevated accompanied with total bilirubin concentrations >2 times the ULN, interrupt entire 3-drug combination regimen.
If ALT or AST concentrations >8 times ULN occur, interrupt entire 3-drug combination regimen.
If ALT or AST concentrations >5 times ULN occur and persist >2 weeks, interrupt entire 3-drug combination regimen.
Special Populations
No special population dosage recommendations at this time.
Cautions for Pretomanid
Contraindications
-
The manufacturer states no specific contraindications for pretomanid.
-
Because pretomanid must be used in conjunction with bedaquiline and linezolid, consider contraindications for these drugs. Consult prescribing information for bedaquiline and linezolid for contraindication regarding use of these drugs.
Warnings/Precautions
Use of Combination Treatment Regimens
Must be used in conjunction with bedaquiline and linezolid. Consider cautions, precautions, contraindications, and drug interactions associated with all 3 drugs.
Hepatotoxicity
Hepatic adverse effects reported in patients receiving the combination regimen of pretomanid, bedaquiline, and linezolid.
Monitor for signs and symptoms of hepatic toxicity (e.g., fatigue, anorexia, nausea, jaundice, dark urine, liver tenderness, hepatomegaly). At a minimum, assess liver function tests (e.g., ALT, AST, alkaline phosphatase, total bilirubin) prior to initiation of the combination regimen, 2 weeks later, and then once monthly as clinically indicated during treatment with the regimen. If there is evidence of new or worsening liver dysfunction, assess for viral hepatitides and discontinue any other concomitant hepatotoxic drugs. Temporary interruption of the pretomanid, bedaquiline, and linezolid regimen may be necessary depending on severity of hepatic toxicity. (See Hepatotoxicity under Dosage and Administration.)
Avoid alcohol and other hepatotoxic drugs or herbal products, especially in those with hepatic impairment
Hematologic Effects
Myelosuppression (e.g., anemia, leukopenia, thrombocytopenia, pancytopenia) reported in patients receiving the combination regimen of pretomanid, bedaquiline, and linezolid; myelosuppression is a known toxicity of linezolid. Anemia, potentially life-threatening, reported. Cytopenias generally began after 2 weeks of treatment.
Evaluate CBCs prior to initiating therapy, 2 weeks later, and then once monthly as clinically indicated.
Temporary interruption, dosage reduction, or discontinuance of linezolid should be considered if myelosuppression develops or worsens. Hematologic parameters generally have increased toward pretreatment values following temporary interruption, dosage reduction, or discontinuance of linezolid.
Peripheral and Optic Neuropathy
Peripheral and optic neuropathies, potentially severe, reported in patients receiving the combination regimen of pretomanid, bedaquiline and linezolid. Peripheral neuropathy and optic neuropathy are known adverse effects of linezolid; generally is reversible or improves following temporary interruption, dosage reduction, or discontinuance of linezolid.
Peripheral neuropathy usually occurred after 8 weeks of treatment with the combination regimen.
Monitor visual function in patients receiving the combination regimen of pretomanid, bedaquiline, and linezolid. If symptoms of visual impairment (e.g., changes in visual acuity or color vision, blurred vision, or visual field defect) occur, interrupt linezolid therapy and perform ophthalmic evaluation promptly.
Prolongation of the QT Interval
Prolongation of the QT interval reported in patients receiving the combination regimen of pretomanid, bedaquiline, and linezolid. Prolongation of the QT interval is known toxicity of bedaquiline.
Risk of QT interval prolongation may be increased in patients receiving other drugs that prolong QT interval; patients with hypocalcemia, hypokalemia, or hypomagnesemia; or patients with a history of torsades de pointes, congenital long QT syndrome, hypothyroidism and bradyarrhythmias, or uncompensated heart failure. Consider the risks and benefits of initiating bedaquiline in such patients; closely monitor ECGs if the regimen of pretomanid, bedaquiline, and linezolid is used.
Perform ECG prior to initiating combination regimen of pretomanid, bedaquiline, and linezolid and at least at 2, 12, and 24 weeks after starting the regimen. Measure serum potassium, calcium, and magnesium concentrations at baseline and correct if necessary. If QT prolongation detected, monitor electrolyte concentrations.
Discontinue the combination regimen in patients who develop clinically important ventricular arrhythmia or QTcF >500 msec (confirmed by repeat ECG). If syncope occurs, perform ECG to detect prolongation of QT interval.
Lactic Acidosis
Lactic acidosis, characterized by recurrent nausea and vomiting, reported in patients receiving the combination regimen of pretomanid, bedaquiline, and linezolid. Lactic acidosis is a known adverse effect of linezolid.
Patients who develop recurrent nausea and vomiting, unexplained acidosis, or a low bicarbonate concentration while receiving the combination regimen of pretomanid, bedaquiline, and linezolid should undergo immediate medical evaluation, including assessment of bicarbonate and lactic acid levels. Consider temporary interruption of linezolid or the entire 3-drug combination regimen.
Specific Populations
Pregnancy
Data regarding use of pretomanid in pregnant women insufficient to determine whether there is a risk of adverse developmental outcomes. In rats and rabbits receiving the drug at doses resulting in maternal exposures approximately 2 times the human exposure at the recommended dosage, no adverse embryofetal toxicities were observed.
Pregnant women are at increased risk for complications from active tuberculosis, which may lead to adverse maternal and/or neonatal outcomes (e.g., maternal anemia, cesarean delivery, preterm delivery, low birthweight, birth asphyxia, perinatal infant death).
Because pretomanid must be used in conjunction with bedaquiline and linezolid, also consider precautions related to use of these drugs in pregnant women.
Lactation
Not known whether distributed into human milk, affects milk production, or has effects on the breast-fed infant. Distributed into milk in rats.
Consider benefits of breast-feeding and the importance of pretomanid to the woman along with potential adverse effects on the breast-fed child from the drug or from the underlying maternal condition.
Because pretomanid must be used in conjunction with bedaquiline and linezolid, also consider precautions related to use of these drugs in breast-feeding women.
Males of Reproductive Potential
Based on findings from animal studies, pretomanid may impair male fertility.
Testicular atrophy and complete infertility observed in male rats receiving pretomanid at exposure levels approximately 1 and 2 times, respectively, the human exposure at the recommended dosage. Testicular toxicity was associated with hormonal changes (decreased serum inhibin B, increased serum follicle stimulating hormone and luteinizing hormone) in male rats and mice. Decreased sperm motility, total sperm count, and increased abnormal sperm ratio observed in monkeys receiving pretomanid at exposure levels approximately 3 times the human exposure at the recommended dosage.
Pediatric Use
Safety and efficacy not established in pediatric patients.
Geriatric Use
Insufficient experience in patients ≥65 years of age to determine whether geriatric patients respond differently than younger adults.
Hepatic Impairment
Not studied in patients with hepatic impairment.
Renal Impairment
Not studied in patients with renal impairment.
Common Adverse Effects
Multiple-drug regimen of pretomanid, bedaquiline, and linezolid: Peripheral neuropathy, acne, anemia, nausea, vomiting, headache, elevated serum concentrations of transaminases (ALT, AST), dyspepsia, decreased appetite, rash, pruritus, abdominal pain, pleuritic pain, elevated serum concentrations of gamma-glutamyltransferase, lower respiratory tract infection, hyperamylasemia, hemoptysis, back pain, cough, visual impairment, hypoglycemia, abnormal loss of weight, diarrhea.
Drug Interactions
Partially metabolized (approximately 20%) by CYP3A4; not a substrate of CYP2C9, 2C19, or 2D6. Does not inhibit CYP1A2, 2C8, 2C9, 2C19, or 2D6 to any clinically important extent and does not induce CYP2C9 or 3A4.
Potent inhibitor of organic anion transporter (OAT) 3 in vitro. Does not inhibit OAT1, organic cation transporter (OCT) 1, OCT2, organic anion transporting polypeptide (OATP) 1B1, OATP1B3, breast cancer resistance protein (BCRP), bile salt export pump (BSEP), P-glycoprotein (P-gp), multidrug and toxin extrusion transporter (MATE) 1, or MATE2K at clinically relevant concentrations. Not a substrate of OAT1, OAT3, OCT2, OATP1B1, OATP1B3, MATE1, MATE2-K, BCRP, or P-gp transporters.
Drugs Affecting or Metabolized by Hepatic Microsomal Enzymes
Moderate or potent CYP3A4 inducers: Pharmacokinetic interaction (decreased pretomanid AUC). Avoid concomitant use.
Drugs Affecting or Affected by Membrane Transporters
OAT3 substrates: Pharmacokinetic interaction (increased AUC of the OAT3 substrate with possible substrate-associated adverse effects). If used concomitantly, monitor for OAT3 substrate toxicity and reduce dosage of the substrate drug if necessary.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Efavirenz |
Decreased pretomanid AUC and plasma concentrations |
Avoid concomitant use |
|
Lopinavir |
Fixed combination of lopinavir and ritonavir (lopinavir/ritonavir): No clinically important effect on pretomanid exposure |
|
|
Methotrexate |
Possible increased methotrexate exposure and increased risk of methotrexate-associated adverse effects |
If used concomitantly, closely monitor for methotrexate-associated adverse effects and reduce methotrexate dosage if needed. |
|
Midazolam |
No clinically important effect on pharmacokinetics of midazolam or its major metabolite (1-hydroxymidazolam) |
|
|
Rifampin |
Decreased pretomanid AUC (66%) and peak plasma concentrations (53%) |
Avoid concomitant use |
Pretomanid Pharmacokinetics
Absorption
Bioavailability
Following oral administration, peak plasma concentrations attained at approximately 4–5 hours.
Dose proportional increases in peak plasma concentrations and AUC with single doses up to 200 mg.
Following multiple 200-mg doses, steady-state plasma concentrations attained within approximately 4–6 days; accumulation ratio is approximately 2.
Food
Administration with high-fat, high-calorie meal (approximately 150, 250, and 500–600 calories from protein, carbohydrate, and fat, respectively) results in 76% increase in peak plasma concentrations and 88% increase in AUC compared with fasting conditions.
Distribution
Extent
Not known whether distributed into human milk; distributed into milk in rats.
Plasma Protein Binding
Approximately 86%.
Elimination
Metabolism
Metabolized by multiple reductive and oxidative pathways; partially metabolized by CYP3A4 (approximately 20%).
Elimination Route
Following a single dose, excreted in urine (53%) and feces (38%), principally as metabolites; only 1% of dose excreted as unchanged pretomanid.
Half-life
Mean terminal half-life is approximately 16–17 hours.
Special Populations
Effect of renal or hepatic impairment on pretomanid pharmacokinetics not studied to date.
No clinically important differences in pharmacokinetics related to body weight, sex, race, pulmonary tuberculosis status, or HIV status.
Stability
Storage
Oral
Tablets
<30°C in tight container; dispense in original container.
Actions
-
Nitroimidazooxazine antimycobacterial agent.
-
Following entry into M. tuberculosis cells, pretomanid is activated by a deazaflavin (F420)-dependent nitroreductase (Ddn) which results in release of reactive nitrogen species (e.g., nitric oxide). In non-replicating mycobacterial cells (anaerobic conditions), nitric oxide acts as a respiratory poison. In actively replicating mycobacterial cells, pretomanid inhibits mycolic acid biosynthesis, thereby inhibiting mycobacterial cell wall production.
-
Active against replicating and non-replicating M. tuberculosis, including drug-susceptible M. tuberculosis and multidrug-resistant (MDR) strains. Usually bactericidal in action,
-
Data from several murine models of pulmonary tuberculosis indicate the 3-drug combination regimen of pretomanid, bedaquiline, and linezolid results in greater reductions in mycobacterial counts in the lungs (superior bactericidal and sterilizing activity) at 4 and 8 weeks and results in fewer relapses at 2 and 3 months after treatment compared to 2-drug combinations of these drugs (i.e., pretomanid and linezolid, bedaquiline and pretomanid, or bedaquiline and linezolid).
-
Not active in vitro against nontuberculosis mycobacteria, including M. avium, M. fortuitum, M. kansasii, and M. smegmatis.
-
M. tuberculosis with reduced susceptibility or resistance to pretomanid in vitro reported. Mutations in M. tuberculosis genes that affect activation of pretomanid (ddn, fgd1, fbiA, fbiB, fbiC) have been associated with resistance to pretomanid; other mechanisms of resistance may also exist.
-
Cross-resistance between pretomanid and other nitroimidazooxazines (e.g., delamanid) reported.
Advice to Patients
-
Importance of providing patient a copy of the manufacturer's patient information (medication guide). Importance of the patient reading the medication guide prior to initiation of therapy and each time the prescription is refilled.
-
Importance of taking pretomanid exactly as prescribed and completing the full course of therapy. Advise patients that pretomanid must be taken in conjunction with bedaquiline and linezolid.
-
Advise patients that missed doses may decrease treatment effectiveness and increase the risk of developing resistance to pretomanid and other antituberculosis drugs.
-
Importance of taking with food.
-
Risk of hepatotoxicity; importance of liver function test monitoring. Inform patients of the signs and symptoms of hepatotoxicity (e.g., nausea, vomiting, abdominal pain, fever, weakness, pruritus, fatigue, anorexia, jaundice, dark urine, light-colored stools) and importance of immediately reporting possible symptoms of hepatotoxicity to their clinician.
-
Risk of peripheral and optic neuropathy. Advise patients to promptly inform clinician if they experience changes in vision; importance of obtaining prompt ophthalmologic evaluation if symptoms of visual impairment occur.
-
Importance of informing clinicians of personal or family history of congenital QT interval prolongation or heart failure.
-
Importance of informing clinician of any history of liver or kidney problems. Safety and effectiveness of the combination regimen of pretomanid, bedaquiline, and linezolid not evaluated in patients with hepatic or renal impairment.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal products, as well as any concomitant illnesses. Advise patients to abstain from alcohol and other hepatotoxic drugs or herbal products.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
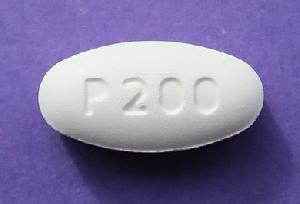
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
200 mg |
Pretomanid Tablets |
Mylan |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions August 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
More about pretomanid
- Check interactions
- Compare alternatives
- Pricing & coupons
- Drug images
- Side effects
- Dosage information
- During pregnancy
- FDA approval history
- Drug class: miscellaneous antituberculosis agents
- Breastfeeding
- En español