Paricalcitol (Monograph)
Brand name: Zemplar
Drug class: Vitamin D
ATC class: A11CC
VA class: VT509
Chemical name: (1α,3β,7E,22E)-19-Nor-9,10-secoergosta-5,7,22-triene-1α,3β,25-triol
Molecular formula: C27H44O3
CAS number: 131918-61-1
Introduction
A synthetic vitamin D analog.110 111 112 113 117
Uses for Paricalcitol
Secondary Hyperparathyroidism
IV paricalcitol used for prevention and treatment of secondary hyperparathyroidism associated with stage 5 chronic kidney disease (CKD).110
Oral paricalcitol used for prevention and treatment of secondary hyperparathyroidism associated with stage 3 or 4 CKD or stage 5 CHD requiring hemodialysis or peritoneal dialysis.117
Paricalcitol Dosage and Administration
General
-
Individualize dosage according to serum or plasma intact parathyroid hormone (iPTH) concentrations and serum concentrations of calcium and phosphorus.110 111 113 117 Nephrology experts currently recommend using individual values for serum calcium and phosphorus (evaluated together) instead of the mathematical construct of calcium times phosphorus product to guide clinical practice.126 128
-
Closely monitor serum calcium and phosphorus concentrations during therapy.110 117 (See Patient Monitoring under Cautions.)
Administration
Oral Administration
Administer orally once daily or 3 times weekly without regard to meals.117
If paricalcitol is administered 3 times weekly, administer no more frequently than every other day.117
IV Administration
Administer by direct IV injection at any time during dialysis, no more frequently than every other day.110
Dosage
Nephrology experts currently state that optimal iPTH concentration for predialysis patients with stage 3a (eGFR 45–59 mL/minute per 1.73 m2) to stage 5 (eGFR <15 mL/minute per 1.73 m2) CKD is unknown, but modest elevations may represent an appropriate adaptive response to declining renal function.128 129
For patients with stage 5 CKD undergoing dialysis, some experts suggest maintaining iPTH concentrations within a range of approximately 2–9 times the assay's ULN (may correspond to range of approximately 130–600 pg/mL for commercial assays130 ).128 PTH assays exhibit substantial variability; previously recommended range of 150–300 pg/mL for patients with stage 5 CKD requiring dialysis was based on an assay that is no longer available.126 130 131
Avoid oversuppression of PTH, which may increase risk of adynamic bone disease.126 131
Pediatric Patients
Secondary Hyperparathyroidism
Stage 3 or 4 CKD
OralPediatric patients 10–16 years of age: Initial dosage of 1 mcg 3 times weekly.117
Individualize dosage based on iPTH concentration and serum calcium and phosphorus concentrations to maintain iPTH concentration within the target range.117
May increase dosage in increments of 1 mcg 3 times weekly (i.e., from 1 mcg 3 times weekly to 2 mcg 3 times weekly) at intervals of 4 weeks.117
May decrease dose by 1 mcg at any time during therapy.117
If patient is receiving 1 mcg 3 times weekly and requires dosage reduction, withhold therapy as needed and resume when appropriate.117
If hypercalcemia is observed, reduce dosage or withhold therapy until the concentration has normalized.117
Stage 5 CKD (Dialysis)
OralPediatric patients 10–16 years of age: Manufacturer recommends calculating initial dose (in mcg) by dividing baseline iPTH concentration (in pg/mL) by 120.117 Round calculated dose down to nearest whole number and administer 3 times weekly.117
Individualize dosage based on iPTH concentration and serum calcium and phosphorus concentrations to maintain iPTH concentration within the target range.117
May increase dosage in increments of 1 mcg 3 times weekly (i.e., from 1 mcg 3 times weekly to 2 mcg 3 times weekly) at intervals of 4 weeks.117
May decrease dose by 2 mcg at any time during therapy.117
If patient is receiving 1 or 2 mcg 3 times weekly and requires dosage reduction, withhold therapy as needed and resume when appropriate.117
If hypercalcemia is observed, reduce dosage or withhold therapy until the concentration has normalized.117
IVChildren and adolescents 5–19 years of age: In one study, initial dosage was 0.04 mcg/kg 3 times weekly if iPTH concentration <500 pg/mL or 0.08 mcg/kg 3 times weekly if iPTH concentration ≥500 pg/mL.110
Dosage in this study was adjusted in increments of 0.04 mcg/kg based on serum concentrations of iPTH, calcium, and calcium times serum phosphorus product (Ca × P).110 Mean dose was 4.6 mcg (range: 0.8–9.6 mcg).110
Adults
Secondary Hyperparathyroidism
Stage 3 or 4 CKD
OralIf baseline iPTH concentration is ≤500 pg/mL, manufacturer recommends initial dosage of 1 mcg once daily or 2 mcg 3 times weekly.117 If baseline iPTH concentration is >500 pg/mL, initial dosage of 2 mcg once daily or 4 mcg 3 times weekly.117
Adjust dosage at 2- to 4-week intervals based on iPTH response.117
Manufacturer recommends maintaining current dosage if decrease in iPTH concentration from baseline is ≥30% but ≤60%.117
If response is inadequate (i.e., iPTH concentration increases, remains unchanged, or is reduced by <30% from baseline), manufacturer recommends increasing dosage in increments of 1 mcg daily (e.g., from 1 mcg daily to 2 mcg daily) or 2 mcg 3 times weekly (e.g., from 2 mcg 3 times weekly to 4 mcg 3 times weekly).117
If iPTH concentration is decreased from baseline by >60% or declines to a value of <60 pg/mL, manufacturer recommends decreasing dosage by 1 mcg daily or by 2 mcg 3 times weekly.117
If patient is receiving dosage of 1 mcg once daily and requires dosage reduction, reduce dosage to 1 mcg 3 times weekly; if further reduction is needed, withhold the drug as needed and reinitiate therapy at a lower dosage by altering dosing interval.117
If hypercalcemia is observed, reduce dosage or withhold therapy until the concentration has normalized.117
Stage 5 CKD (Dialysis)
OralManufacturer recommends calculating initial dose (in mcg) by dividing baseline iPTH concentration (in pg/mL) by 80; administer calculated dose 3 times weekly.117
To minimize risk of hypercalcemia, initiate therapy only if adjusted baseline serum calcium concentration is ≤9.5 mg/dL.117
Individualize dosage based on iPTH, serum calcium, and serum phosphorus concentrations.117 Manufacturer recommends calculating new dose (in mcg) by dividing most recent iPTH concentration (in pg/mL) by 80.117
If hypercalcemia is observed, reduce dosage or withhold therapy until the concentration has normalized.117 If serum calcium concentrations are elevated, decrease dose by 2–4 mcg.117
As iPTH concentration approaches target range, small individualized dose adjustments may be necessary to achieve a stable iPTH concentration.117
In situations where iPTH, calcium, or phosphorus is monitored less frequently than once weekly, manufacturer states that a more modest initial and dose-titration ratio (e.g., iPTH concentration divided by 100) may be appropriate.117
IVInitial dosage of 0.04–0.1 mcg/kg (2.8–7 mcg) at dialysis (no more often than every other day).110
Manufacturer recommends adjusting dosage at 2- to 4-week intervals with the goal of reducing iPTH concentration to no more than 1.5–3 times ULN.110
Manufacturer recommends maintaining current dosage if decrease in iPTH concentration from baseline is ≥30% but ≤60% or if iPTH concentration is 1.5–3 times the ULN.110
If response is inadequate (i.e., iPTH concentration increases, remains unchanged, or is reduced by <30% from baseline), manufacturer recommends increasing dose by 2–4 mcg per dose at 2- to 4-week intervals.110
If iPTH concentration is decreased from baseline by >60%, reduce dosage.110
If serum calcium (in mg/dL) times serum phosphorus (in mg/dL) product (Ca × P) is >75, reduce or withhold dosage immediately until parameters are normalized; reinitiate drug at a lower dosage. 110
In patients receiving a calcium-containing phosphate binder, dosage of the phosphate binder may be reduced or withheld; alternatively, the patient can be switched to a non-calcium-containing phosphate binder.110
Special Populations
Hepatic Impairment
Mild to moderate hepatic impairment: Dosage adjustment not required.110 117 (See Hepatic Impairment under Cautions.)
Geriatric Patients
No specific dosage recommendations.110 117 (See Geriatric Use under Cautions.)
Cautions for Paricalcitol
Contraindications
-
Known hypersensitivity to paricalcitol or any ingredient in the formulation.110
Warnings/Precautions
Excessive Use
Excessive doses of vitamin D analogs (e.g., paricalcitol) may result in excessive suppression of PTH concentrations, hypercalcemia, hypercalciuria, hyperphosphatemia, and adynamic bone disease.110 117
Hypercalcemia
Progressive hypercalcemia resulting from vitamin D overdosage may require emergency treatment measures.110 117 If clinically important hypercalcemia develops, reduce or withhold paricalcitol therapy immediately, withdraw calcium supplements, administer a low-calcium diet, and monitor closely for changes in fluid and electrolyte balance and ECG (especially in those receiving a cardiac glycoside).110
Acute hypercalcemia may increase risk of cardiac arrhythmias and seizures, and potentiate toxic effects of cardiac glycosides.110 117
Chronic hypercalcemia increases risk of soft-tissue calcification, including vascular calcification.110 117
Concomitant use of high dosages of calcium or thiazide diuretics increases risk of hypercalcemia; high intake of calcium and phosphates may necessitate frequent patient monitoring and individualized dosage titration.110 117
Do not use prescription-based doses of vitamin D and its analogs during paricalcitol therapy.110 117
Cardiac Glycoside Toxicity
Hypercalcemia increases risk of cardiac glycoside toxicity; use concomitantly with caution.110 117 (See Specific Drugs and Foods under Interactions.)
Patient Monitoring
In patients receiving oral paricalcitol, monitor serum calcium, serum phosphorus, and serum or plasma iPTH concentrations at least every 2 weeks for 3 months after initiation of therapy or following any dosage adjustment, then monthly for 3 months, and every 3 months thereafter.117
In patients with stage 5 CKD receiving IV paricalcitol, monitor serum calcium and phosphorus concentrations frequently (e.g., twice weekly) during initial dosage adjustment and after subsequent dosage adjustments; once dosage has been established, monitor at least monthly.110 Monitor serum or plasma iPTH concentrations every 3 months; more frequent monitoring may be required during dosage adjustments.110
Predialysis Patients
Vitamin D analogs (e.g., paricalcitol, calcitriol) may increase Scr and therefore decrease eGFR in predialysis patients.117
Aluminum Toxicity
Avoid long-term concomitant use of aluminum-containing preparations (e.g., antacids, phosphate binders); risk of increased blood aluminum concentrations and aluminum bone toxicity.110 117
Specific Populations
Pregnancy
Category C.110
Limited data on paricalcitol use in pregnant women.117
Slight increase in embryofetal loss observed in animals; increased stillbirths and newborn mortality observed in animals at maternally toxic doses.110 117
CKD increases maternal risk for hypertension, spontaneous abortion, preterm labor, and preeclampsia and increases fetal risk for intrauterine growth restriction, prematurity, polyhydramnios, stillbirth, and low birth weight.117
Lactation
Distributed into milk in rats;110 117 not known whether paricalcitol distributes into human milk, affects milk production, or affects nursing infants.110 117
Avoid nursing during paricalcitol therapy.110 117
Pediatric Use
Safety and efficacy of oral paricalcitol not established in pediatric patients <10 years of age. 117
Safety and efficacy of IV paricalcitol not established in pediatric patients <5 years of age.110
Geriatric Use
No substantial differences in safety and efficacy in those ≥65 years of age relative to younger adults,110 117 but increased sensitivity cannot be ruled out.117
Hepatic Impairment
Not studied in patients with severe hepatic impairment.110 117
Mild or moderate hepatic impairment does not alter pharmacokinetics.110 117
Common Adverse Effects
Oral administration in patients with stage 3 or 4 CKD: Diarrhea,117 hypertension,117 viral infection,117 edema,117 hypersensitivity,117 nausea,117 arthritis,117 dizziness,117 headache,117 hypotension,117 vertigo,117 vomiting.117
Oral administration in patients with stage 5 CKD: Diarrhea,117 nasopharyngitis,117 dizziness,117 vomiting,117 constipation,117 fluid overload,117 insomnia,117 peritonitis.117
IV administration in patients with stage 5 CKD: Nausea,110 vomiting,110 edema,110 arthralgia,110 chills,110 GI hemorrhage,110 influenza,110 pneumonia,110 pyrexia,110 sepsis.110
Drug Interactions
Partially metabolized by CYP3A.110 117
Drugs Affecting or Metabolized by Hepatic Microsomal Enzymes
Potent CYP3A inhibitors: Potential pharmacokinetic interaction (increased plasma paricalcitol concentrations).110 117
CYP substrates: Does not appear to inhibit clearance of drugs metabolized by CYP isoenzymes 1A2, 2A6, 2B6, 2C8, 2C9, 2C19, 2D6, 2E1, or 3A, or induce clearance of drugs metabolized by CYP isoenzymes 2B6, 2C9, or 3A.110
Specific Drugs and Foods
|
Drug or Food |
Interaction |
Comments |
|---|---|---|
|
Antifungals, azoles (itraconazole, ketoconazole, posaconazole, voriconazole) |
Possible increased plasma paricalcitol concentrations110 117 Ketoconazole: Increased paricalcitol AUC and half-life110 117 |
Dosage adjustment of paricalcitol may be needed117 Closely monitor iPTH and serum calcium concentrations when initiating or discontinuing therapy with a potent CYP3A4 inhibitor117 |
|
Bile acid sequestrants cholestyramine, colestipol) |
Allow as long a time interval as possible between ingestion of paricalcitol and bile acid sequestrant117 d Cholestyramine: Administer oral paricalcitol >1 hour before or 4–6 hours after cholestyramine (or at longest possible interval)117 |
|
|
Cardiac glycosides |
Possible cardiac arrhythmiasd |
|
|
Clarithromycin |
Possible increased plasma paricalcitol concentrations110 117 |
Dosage adjustment of paricalcitol may be needed117 Closely monitor iPTH and serum calcium concentrations when initiating or discontinuing clarithromycin therapy117 |
|
Conivaptan |
Possible increased plasma paricalcitol concentrations117 |
Dosage adjustment of paricalcitol may be needed117 Closely monitor iPTH and serum calcium concentrations when initiating or discontinuing conivaptan therapy 117 |
|
Grapefruit juice |
Possible increased plasma paricalcitol concentrations117 |
Dosage adjustment of paricalcitol may be needed117 Closely monitor iPTH and serum calcium concentrations when initiating or discontinuing use of a potent CYP3A4 inhibitor117 |
|
HIV protease inhibitors (atazanavir, indinavir, lopinavir/ritonavir, nelfinavir, ritonavir, saquinavir) |
Possible increased plasma paricalcitol concentrations110 117 |
Dosage adjustment of paricalcitol may be needed117 Closely monitor iPTH and serum calcium concentrations when initiating or discontinuing therapy with an HIV protease inhibitor117 |
|
Mineral oil |
May interfere with intestinal absorption of vitamin D analogs117 d |
Administer oral paricalcitol >1 hour before or 4–6 hours after mineral oil (or at longest possible interval)117 |
|
Nefazodone |
Possible increased plasma paricalcitol concentrations110 117 |
Dosage adjustment of paricalcitol may be needed117 Closely monitor iPTH and serum calcium concentrations when initiating or discontinuing nefazodone therapy117 |
|
Omeprazole |
||
|
Telithromycin |
Possible increased plasma paricalcitol concentrations110 117 |
Dosage adjustment of paricalcitol may be needed117 Closely monitor iPTH and serum calcium concentrations when initiating or discontinuing telithromycin therapy117 |
|
Thiazide diuretics |
Paricalcitol Pharmacokinetics
Absorption
Bioavailability
Well absorbed following oral administration; absolute bioavailability is about 72–86%.117
Food
High-fat meal increased time to peak plasma concentration of paricalcitol capsules by about 2 hours but did not affect AUC or peak concentration.117
Special Populations
Hemodialysis does not appear to affect plasma concentrations.110 e h
Distribution
Distributed into milk in rats; not known whether distributed into human milk.110 117
Plasma Protein Binding
Elimination
Metabolism
Extensively metabolized (about 98%) by multiple hepatic and nonhepatic enzymes (e.g., CYP24, CYP3A4, uridine diphosphate-glucuronosyltransferase [UGT] 1A4).110 117 i
Elimination Route
Paricalcitol and its metabolites eliminated principally in feces via biliary excretion.110 117
Excreted in feces mainly (about 63–70%) as metabolites (2% as unchanged drug), and in urine as metabolites (18–19%).110 117
Half-Life
In healthy individuals: 4–7 hours.110 117
Special Populations
Pharmacokinetic profile of oral paricalcitol in patients with stage 5 CKD undergoing hemodialysis or peritoneal dialysis similar to that in patients with stage 3 or 4 CKD.117
Half-life following oral administration: 14–20 hours in patients with stage 3 or 4 CKD or stage 5 CKD undergoing hemodialysis or peritoneal dialysis.117
Half-life following IV administration: 13.9 hours in patients with stage 5 CKD undergoing hemodialysis and 15.4 hours in those with stage 5 CKD undergoing peritoneal dialysis.110
Mild or moderate hepatic impairment does not alter pharmacokinetics.110 117
Stability
Storage
Oral
Capsules
25°C (may be exposed to 15–30°C).117
Parenteral
Injection
25°C (may be exposed to 15–30°C).110
Multidose vial: Stable at room temperature for up to 7 days after initial use.110
Actions
-
A synthetic vitamin D analog of calcitriol (the metabolically active form of vitamin D).110 111 112 113 117
-
In patients with CKD, decreased metabolic activation of vitamin D in the kidneys results in secondary hyperparathyroidism,117 a b c characterized by increased PTH concentrations110 117 and disturbances in calcium and phosphorus homeostasis.110 117 These effects may affect bone turnover rate and may result in renal osteodystrophy.110 117 d
-
Biologic actions of paricalcitol are mediated through binding of the vitamin D receptor, which results in selective activation of vitamin D responsive pathways.110 117
-
Paricalcitol reduces serum or plasma PTH concentrations in patients with CKD.110 117 e f Appears to be as effective as calcitriol in suppressing PTH secretion.b e f g
Advice to Patients
-
Importance of adherence to diet and calcium supplementation regimen.110 117
-
Importance that patients with CKD use appropriate types of phosphate-binding compounds to control serum phosphate concentrations; importance of avoiding excessive use of aluminum-containing compounds.110 117
-
Importance of laboratory monitoring (e.g., serum calcium, phosphorus, and iPTH) during paricalcitol therapy.110 117
-
Importance of reporting potential manifestations of hypercalcemia (e.g., tiredness, difficulty thinking, loss of appetite, nausea, vomiting, constipation, increased thirst, increased urination, weight loss).110 117
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, and dietary or herbal supplements.110 117
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.110 117
-
Importance of informing patients of other important precautionary information.110 117 (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
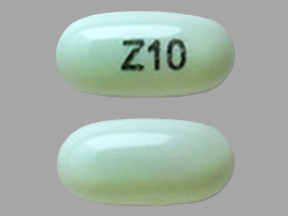
|
Oral |
Capsules, liquid-filled |
1 mcg* |
Paricalcitol Capsules |
|
|
Zemplar |
AbbVie |
|||
|
2 mcg* |
Paricalcitol Capsules |
|||
|
Zemplar |
AbbVie |
|||
|
4 mcg* |
Paricalcitol Capsules |
|||
|
Parenteral |
Injection, for IV use only |
2 mcg/mL* |
Paricalcitol Injection |
|
|
Zemplar |
AbbVie |
|||
|
5 mcg/mL* |
Paricalcitol Injection |
|||
|
Zemplar |
AbbVie |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions February 11, 2019. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
References
110. AbbVie Inc. Zemplar (paricalcitol) injection prescribing information. North Chicago, IL; 2013 Jan.
111. Goldenberg MM. Paricalcitol, a new agent for the management of secondary hyperparathyroidism in patients undergoing chronic renal dialysis. Clin Ther. 1999; 21:432-41. https://pubmed.ncbi.nlm.nih.gov/10321413
112. Slatopolsky E, Finch J, Ritter C et al. A new analog of calcitriol, 19- nor-1,25-(OH)2D2 suppresses parathyroid hormone secretion in uremic rats in the absence of hypercalcemia. Am J Kidney Dis. 1995; 26:852-60. https://pubmed.ncbi.nlm.nih.gov/7485144
113. Martin KJ, Gonzalez EA, Gellens M et al. 19-nor-1-α-25-dihydroxyvitamin D2(paricalcitol) safely and effectively reduces the levels of intact parathyroid hormone in patients on hemodialysis. J Am Soc Nephrol. 1998; 9:1427-32. https://pubmed.ncbi.nlm.nih.gov/9697664
116. Abbott, Abbott Park, IL: Personal communication.
117. AbbVie Inc. Zemplar (paricalcitol) capsules prescribing information. North Chicago, IL; 2016 Oct.
126. Kidney Disease: Improving Global Outcomes (KDIGO) CKD–MBD Work Group. KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease—mineral and bone disorder (CKD–MBD). Kidney Int. 2009; 76 (Suppl 113): S1–S130.
128. Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Update Work Group. KDIGO 2017 clinical practice guideline update for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease—mineral and bone disorder (CKD-MBD). Kidney Int Suppl. 2017; 7:1-59.
129. Isakova T, Nickolas TL, Denburg M et al. KDOQI US Commentary on the 2017 KDIGO Clinical Practice Guideline Update for the Diagnosis, Evaluation, Prevention, and Treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD). Am J Kidney Dis. 2017; 70:737-751. https://pubmed.ncbi.nlm.nih.gov/28941764
130. Uhlig K, Berns JS, Kestenbaum B et al. KDOQI US commentary on the 2009 KDIGO Clinical Practice Guideline for the Diagnosis, Evaluation, and Treatment of CKD-Mineral and Bone Disorder (CKD-MBD). Am J Kidney Dis. 2010; 55:773-99. https://pubmed.ncbi.nlm.nih.gov/20363541
131. Bover J, Ureña P, Ruiz-García C et al. Clinical and Practical Use of Calcimimetics in Dialysis Patients With Secondary Hyperparathyroidism. Clin J Am Soc Nephrol. 2016; 11:161-74. https://pubmed.ncbi.nlm.nih.gov/26224878
a. Standing Committee on the Scientific Evaluation of Dietary Reference Intakes of the Food and Nutrition Board, Institute of Medicine, National Academy of Sciences. Dietary reference intakes for calcium, phosphorus, magnesium, vitamin D, and fluoride. Washington, DC: National Academy Press; 1997. (Uncorrected proofs.)
b. Sakhaee K, Gonzalez GB. Update on renal osteodystrophy: pathogenesis and clinical management. Am J Med Sci. 1999; 317:251-60. https://pubmed.ncbi.nlm.nih.gov/10210362
c. Tan AU Jr, Levine BS, Mazess RB et al. Effective suppression of parathyroid hormone by 1 alpha-hydroxy-vitamin D2 in hemodialysis patients with moderate to severe secondary hyperparathyroidism. Kidney Int. 1997; 51:317-23. https://pubmed.ncbi.nlm.nih.gov/8995749
d. AHFS Drug Information. McEvoy GK, ed. Vitamin D Analogs General Statement. Bethesda, MD: American Society of Health-Systems Pharmacists.
e. Goldenberg MM. Paricalcitol, a new agent for the management of secondary hyperparathyroidism in patients undergoing chronic renal dialysis. Clin Ther. 1999; 21:432-41. https://pubmed.ncbi.nlm.nih.gov/10321413
f. Martin KJ, Gonzalez EA, Gellens M et al. 19-nor-1-α-25-dihydroxyvitamin D2 (paricalcitol) safely and effectively reduces the levels of intact parathyroid hormone in patients on hemodialysis. J Am Soc Nephrol. 1998; 9:1427-1432. https://pubmed.ncbi.nlm.nih.gov/9697664
g. Slatopolsky E, Dusso A, Brown A. New analogs of vitamin D3. Kidney Int. 1999; 73 (suppl) S46-51.
h. Cato A 3rd, Cady WW, Soltanek C et al. Effect of hemodialysis on the pharmacokinetics of 19-nor-1α,25-dihydroxy-vitamin D2. Am J Kidney Dis. 1998; 32(Suppl):S55-60. https://pubmed.ncbi.nlm.nih.gov/9808144
i. Robinson, DM, Scott LJ. Paricalcitol–A review of its use in the management of secondary hyperparathyroidism. Drugs. 2005; 65:559-76. https://pubmed.ncbi.nlm.nih.gov/15733015
Related/similar drugs
More about paricalcitol
- Check interactions
- Compare alternatives
- Pricing & coupons
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: vitamins
- En español
Patient resources
- Paricalcitol drug information
- Paricalcitol (Intravenous) (Advanced Reading)
- Paricalcitol (Oral) (Advanced Reading)